Screening for Children
Childhood health record books provide an excellent opportunity for communication between different health care givers; parents should be provided with the record books and encouraged to bring them to every visit. Various recommendations for screening are made under the following headings.
-
Height/Weight/Head Circumference: Record length/height, weight, and head circumference at regular intervals. Head circumference can be recorded until 2 years and should increase by 1 cm per month in the first 3 months, then 0.5 cm per month from 3–6 months. The adequacy of a child’s growth cannot be assessed on one measurement and serial recordings on growth charts are recommended.
-
Hips: Screen for congenital dislocation at birth, 6–8 weeks, 6–9 months, and 12–24 months. The flexed hips are abducted, checking for movement and a ‘clunk’ of the femoral head forwards (the test is most likely to be positive at 3–6 weeks and usually negative after 8 weeks). Shortening or limited abduction is also abnormal. Ultrasound examination is more sensitive than the clinical examination, especially up to 3–4 months. Observe gait when starting to walk.
-
Strabismus: Strabismus should be sought in all infants and toddlers by occlusion testing (not very sensitive), examining light reflexes and questioning parents, which must be taken very seriously. Amblyopia can be prevented by early recognition and treatment of strabismus by occlusion and surgery. Early referral is essential.
-
Visual Acuity: At birth and 2 months, eyes should be inspected and examined with an ophthalmoscope with a 3+ lens at a distance of 20–30 cm to detect cataracts and red reflexes. At 9 months gross vision should be determined by assessing ability to see common objects. Visual acuity should be formally assessed at school entry using Sheridan Gardiner charts.
-
Hearing: Hearing should be tested by distraction at 9 months or earlier; also by pure tone audiometry at 1000 and 4000 hertz when a child is 4 years (preschool entry) and 12 years.
- Note: Formal audiological evaluation should be carried out at any time if there is clinical suspicion or parental concern. No simple screening test is very reliable for sensorineural or conductive deafness.
-
Testes: Screen at birth, and 6–8 weeks, 6–9 months, and 3 years for absence or maldescents. Those who have been treated for maldescents have a higher risk of neoplastic development in adolescence.
-
Oral Health/Dental Assessment/Fluoride: Advise daily fluoride drops or tablets, if water supply is not fluoridated. Children’s teeth should be checked regularly, particularly if a school dental service is not available. Advice should be given on sugar consumption, especially night-time bottles, and tooth cleaning with fluoride toothpaste to prevent plaque.
-
Scoliosis: Screening of females by the forward flexion test, which is carried out around 12 years of age, is of questionable value because of poor sensitivity and specificity.
-
Congenital Heart Disease: The heart should be auscultated at birth, in the first few days, at 6–8 weeks, and on school entry.
-
Femoral Pulses: Testing for absence of femoral pulses or delay between brachial/femoral pulses at birth and 8 weeks will exclude coarctation of the aorta. Refer the child immediately if concerned.
-
Speech and Language: A child’s speech should be intelligible to strangers by 3 years. It is related to hearing.
Screening for Adults
-
Weight: Weight should be recorded at least every few years. Obesity is a major reversible health risk for adults, contributing to many diseases (e.g., heart disease, diabetes, arthritis). Body mass index (BMI) should ideally be between 20 and 25.
-
Abdominal Obesity: Abdominal obesity is a major risk factor for adults. The waist:hip circumference ratio is regarded as a useful predictor of cardiac disease. Recommended waist:hip ratios are:
- males <0.9
- females <0.8
-
Blood Pressure: Blood pressure should be recorded at least every 1–2 years on all people 16 years and over. There is no dispute that control of blood pressure results in reduced mortality from cerebrovascular accidents and, to a lesser extent, heart disease, kidney failure, and retinopathy.
-
Cholesterol: All adults aged 45 and over should have a 5-yearly estimation of serum cholesterol. Total cholesterol is adequate for screening purposes. HDL levels give additional information.
- The National Heart Foundation recommends keeping cholesterol levels below 4.0 mmol/L. For most, dietary modification is sufficient to achieve these levels; some may require drug treatment.
-
Fasting Blood Glucose: Screen every 3 years for all patients >40 years of age.
-
Cervical Cancer: From age 25 (to age 74), women who have ever been sexually active should commence cervical screening with a HPV test 2 years after their last Pap test. If negative, this can be performed every 5 years. If positive, cervical cytology will be checked with the sample and follow-up is determined according to the national guidelines.
-
Breast Cancer: Mammography should be performed at least every 2 years on women aged 50–74 years. It is not useful for screening prior to age 40 years due to difficulty in discriminating malignant lesions from dense tissue. Women aged 40–49 years may also choose to have a mammogram. Mammography must not be used alone to exclude cancer if a lump is palpable.
-
Colorectal Cancer: A history should be taken, with specific enquiry as to family history of adenomas or colorectal cancer, past history of inflammatory bowel disease, and rectal bleeding.
- Rectal examination should be performed as part of an examination. Immunochemical faecal occult blood testing (FOBT) every 2 years is now recommended for screening for people over 50 years (continuing to 74 years) without symptoms and with average or slightly above average risk.
-
Prostate Cancer: Screening is controversial. Patients should make their own decision after being fully informed of the potential benefits, risks, and uncertainties of testing.
-
Oral Hygiene/Cancer: Patients should be counselled about cessation of smoking and alcohol consumption, and dental hygiene should be taught. The oral cavity should be inspected annually in patients over the age of 40 years.
Immunization
-
Influenza: Influenza immunisation is recommended on an annual basis for persons of all ages with chronic debilitating diseases, especially chronic cardiac, pulmonary, kidney, and metabolic diseases, persons over 65 years of age.
-
Pneumococcal Disease: Those at higher risk of fatal pneumococcal infection (e.g., post-splenectomy or Hodgkin lymphoma) should receive a booster every 5 years.
-
Hepatitis A: It is recommended for health workers, child care workers, sewage workers, non-immune homosexual men, those with chronic liver disease, recipients of blood products, or travelers to hepatitis A-endemic areas.
-
Hepatitis B: Immunisation is recommended routinely for health care personnel, personnel and residents of institutions, prisoners and prison staff, persons with frequent and/or close contact with high-risk groups, and persons at increased risk due to their sexual practices and their household contacts. Booster doses are recommended for immunosuppressed individuals.
-
Q Fever: People at reasonable risk from Q fever, particularly abattoir workers, should be given this vaccine, which is virtually 100% effective.
-
Measles-Mumps-Rubella: All non-immune women who are postpartum or of child-bearing age should be immunised.
-
Varicella Vaccine: Those over 12 years have a course of two injections.
-
Meningococcal Vaccine: The main vaccine that is available is a quadrivalent polysaccharide vaccine against serogroups A, C, Y, and W125 for use in individuals over 2 years as a single injection. Universal prevention remains unsatisfactory.
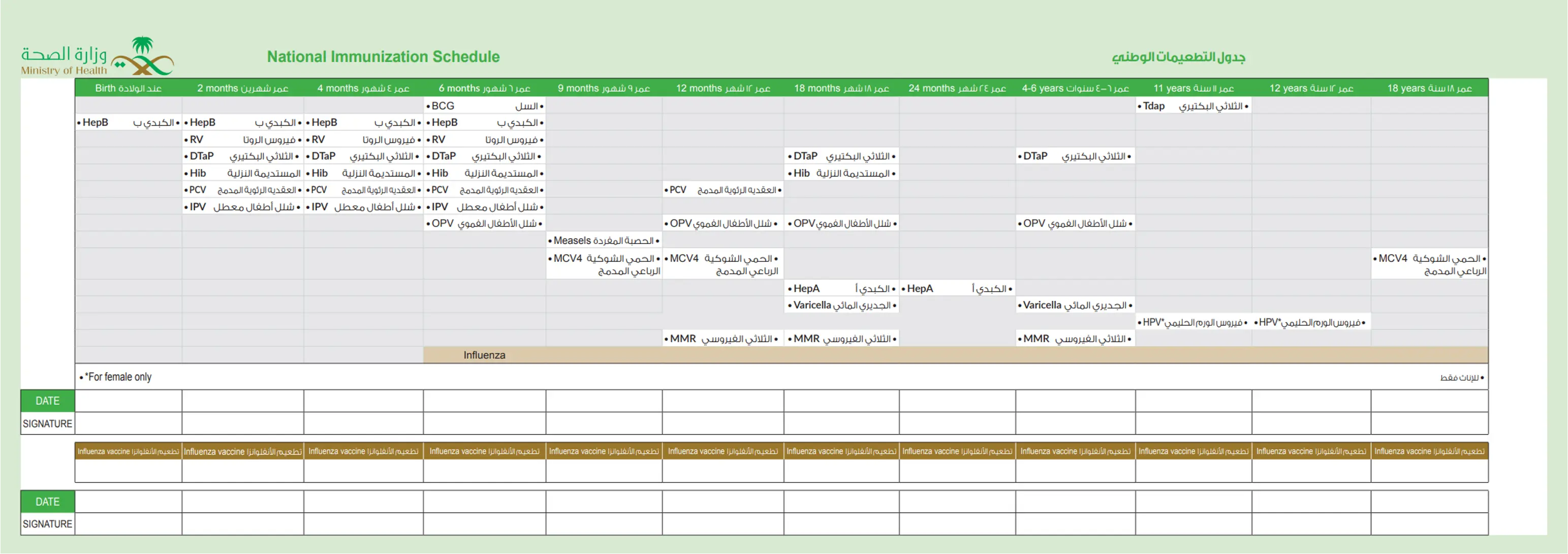
National Immunization Schedule
Screening in General Practice
WHO Criteria for a Good Screening Test: Policy perspective
- The condition screened for should be an important one
- The facilities for diagnosis and treatment should be available
- There should be a recognised latent or early symptomatic stage
- There should be a suitable test or examination which has few false positives - specificity - and few false negatives - sensitivity
- There should be an acceptable treatment for patients with the disease
- The test or examination should be acceptable to the population
- The cost, including diagnosis and subsequent treatment, should be economically balanced in relation to expenditure on medical care
Wilson’s Criteria for Screening: scientific perspective
- The condition should be an important health problem
- The natural history of the condition should be understood
- There should be a recognisable latent or early symptomatic stage
- There should be a test that is easy to perform and interpret, acceptable, accurate, reliable, sensitive, and specific
- There should be an accepted treatment recognised for the disease
- Treatment should be more effective if started early
- There should be a policy on who should be treated
- Diagnosis and treatment should be cost-effective
- Case-finding should be a continuous process