Hemorrhoids
 Swollen of normal blood vessels at lower rectum (hemorrhoidal venous cushions)
Swollen of normal blood vessels at lower rectum (hemorrhoidal venous cushions)
Hemorrhoidal venous cushions are a normal part of the human anorectum and arise from subepithelial connective tissue within the anal canal.
Normal hemorrhoidal tissue:
- 15-20% of resting anal pressure
- Provides important sensory information, enabling the differentiation between solid, liquid, and gas
- Help in defecation
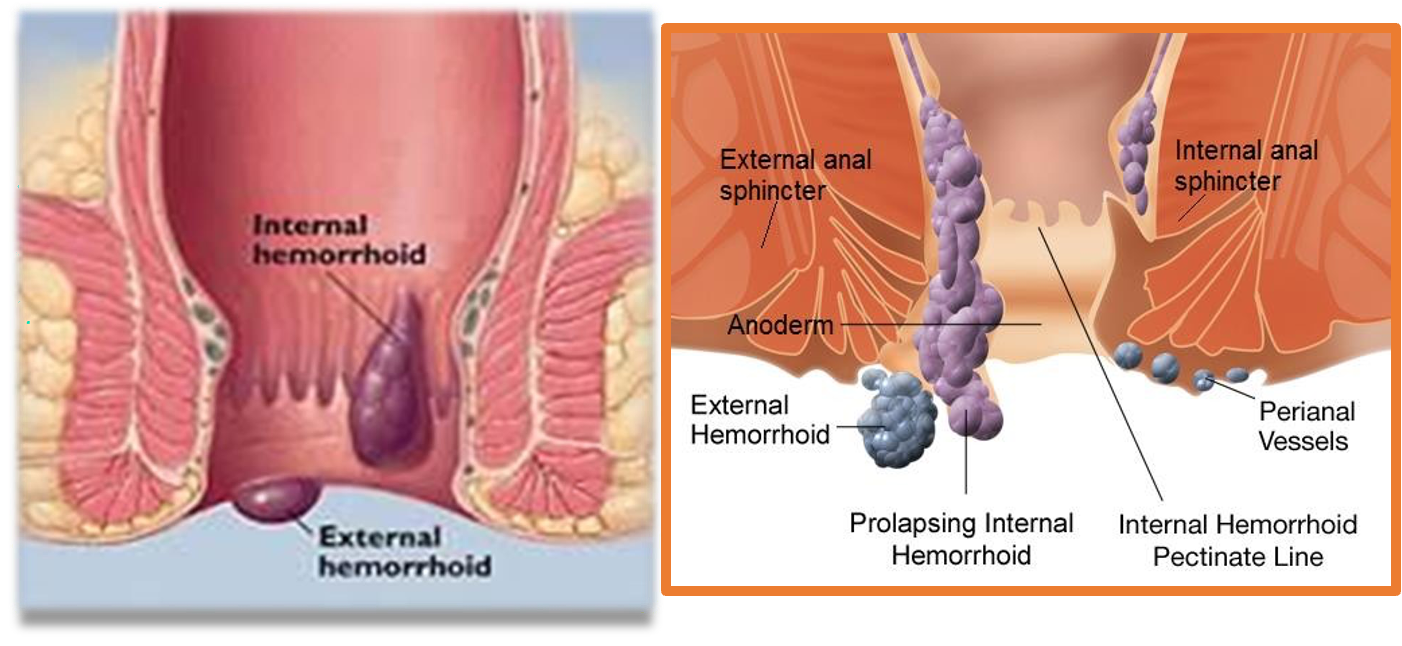
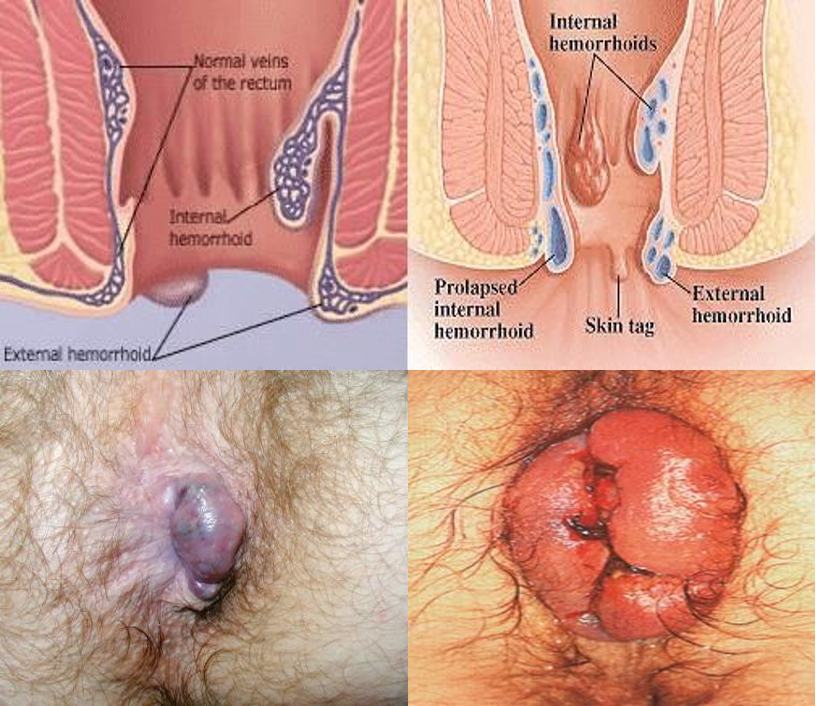
Classified by their anatomic origin within the anal canal and by their position relative to the dentate line into internal and external
External hemorrhoids:
-
Develop from ectoderm and are covered by squamous epithelium.
-
Innervated by cutaneous nerves that supply the perianal area. These nerves include the pudendal nerve and the sacral plexus.
-
External hemorrhoids drain through the inferior rectal vein into the inferior vena cava.
- External hemorrhoidal veins are found circumferentially under the anoderm
Internal hemorrhoids:
-
Derived from endoderm and lined with columnar epithelium of anal mucosa.
-
No somatic sensory nerves
-
Internal hemorrhoids drain through the superior rectal vein into the portal system.
-
Rich anastomoses exist between these 2 and the middle rectal vein, connecting the portal and systemic circulations.
Internal hemorrhoids have 3 main cushions:
- Left lateral
- Right posterior (most common)
- Right anterior areas
- Minor tufts can be found between the major cushions.
Etiology:
- Degeneration of the supporting fibroelastic tissue and smooth muscle
- Decreased venous return
- Portal hypertension and anorectal varices
- Increased intra-abdominal pressure:
- Straining and constipation
- Pregnancy (Combined !!)
- Weight lifting
Symptoms:
- Depends on the type
- Fresh PR bleeding
- Anal pain with swelling
Complications:
- Thrombosis
- Prolapse
- Erosions
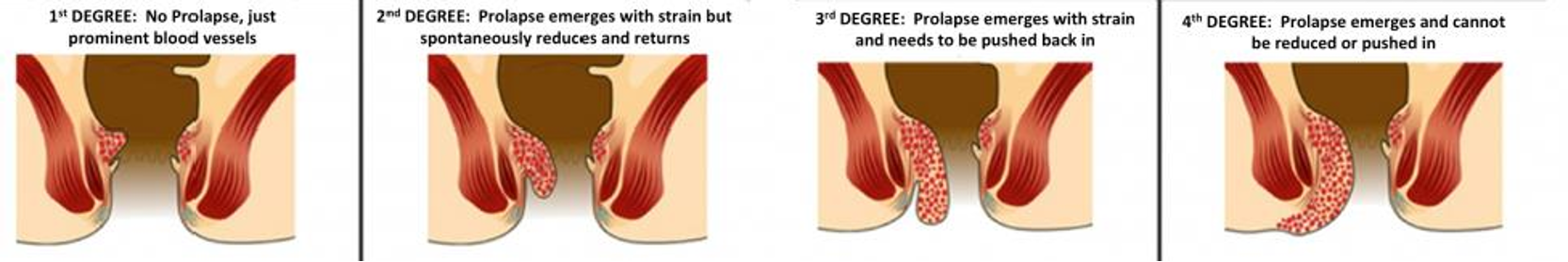
Grades of internal types:
- Grade I: Project into the anal canal and often bleed
- Grade II: Protrude beyond anal verge with straining but reduced spontaneously
- Grade III: Protrude spontaneously and require manual reduction
- Grade IV: chronically prolapse and cannot be reduced
Diagnosis:
- Clinically, DRE, Anoscope
Management:
- Type, symptoms, and grades
- Local vs systemic
- Conservative therapy
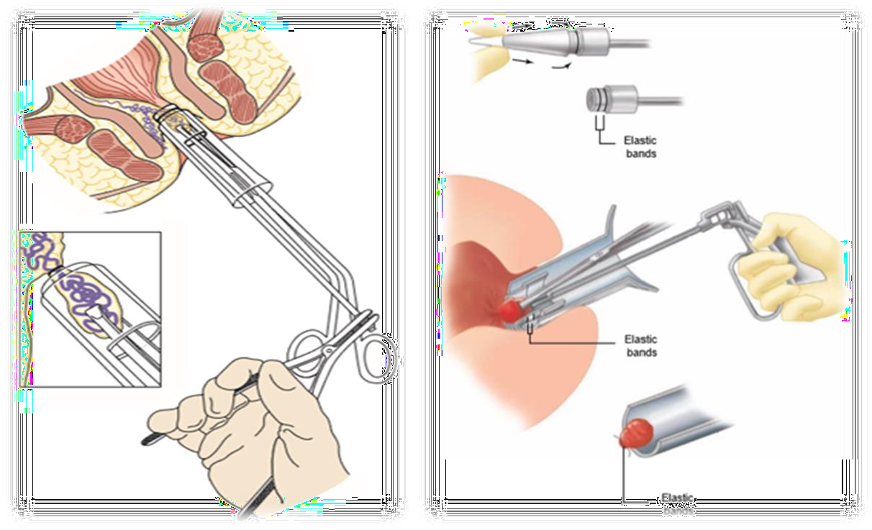
- Surgical therapy:
- Indications
- External haemorrhoides: Incision, & clot evacuation
- Internal haemorrhoides: Banding, Conventional, Stappled, ligasure