Patients with a generalized peritonitis present with some characteristic features:
- Patients often lay completely still, not to move their abdomen, and look unwell
- This is especially important when compared to a renal colic, whereby patients are constantly moving and cannot get comfortable.
- Tachycardia and potential hypotension
- A completely rigid abdomen with percussion tenderness
- Involuntary guarding – the patient involuntarily tenses their abdominal muscles when you palpate the abdomen
- Reduced or absent bowel sounds, suggesting the presence of a paralytic ileu
-
Pathogenesis
- Free bowel perforation (commonest cause)
- Inflammation leads to exudation & transudation
- Exudates inhibits peristalsis & glues greater omentum
- Fibrinous adhesion prevents spread
- Fluid accumulates in lumen & peritoneum
- Intravascular hypovolaemia
-
Clinical features
- Abdominal pain: localized initially, spreading to whole abdomen,
- Aggravated with movement
- Fever, tachycardia
- Restricted abdominal wall movement,
- Generalized tenderness, guarding, rigidity, rebound tenderness – (peritonism)
- Absent bowel sounds
- Late cases: Septic shock, silent abdomen, increasing distension, anxious face
-
Investigations:
- Labs: CBC, u/e, amylase,
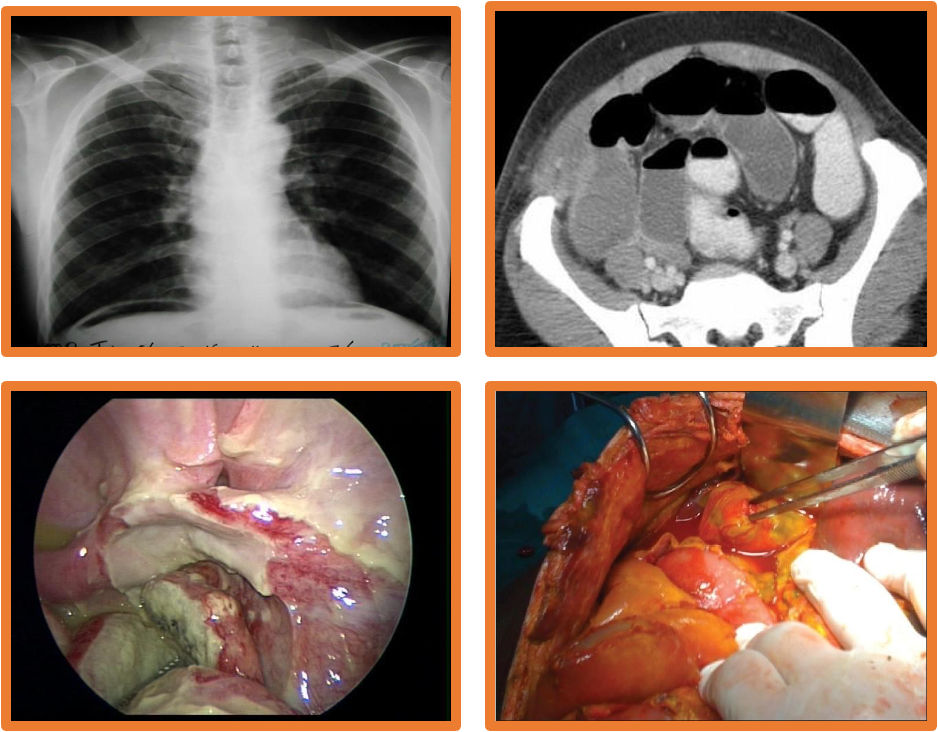
- Imaging: upright CXR, AXR, U/S, CT scan, peritoneal aspiration
-
Treatment:
- NPO, IV fluid- correct fluid & electrolyte imbalance
- NG tube: Aspiration & drainage
- Broad spectrum antibiotics
- Analgesia
- Operative management: Excision, repair, lavage & drainage