Pediatric Block Objectives and Contents For P1
INTRODUCTION TO PEDIATRIC COURSE (PED 632)
DEFINITION
Pediatrics is that branch of medicine concerned with the study and care of infants, children, and youth in health and disease, their growth and development.
THE CURRICULUM
The Pediatric topics are divided between (PED 632) and (PED 635) courses; however, it is impossible to cover all topics in detail, and emphasis is put on graduating general physicians who have enough basics in pediatrics. The theory portion of the curriculum, which includes lectures, tutorials, and seminars, is divided equally between (PED 632) and (PED 635), but the clinical training in pediatric wards, OPD, ER, Nursery, and PICU depends on the availability of cases, so students may confront cases not covered by lectures yet.
OBJECTIVES
1. General Objectives:
To graduate a physician who:
- is aware of the personal qualities and attitudes required by a physician caring for children and their families, e.g., empathy, concern, gentleness, etc.
- has acquired adequate basic knowledge and skills in pediatrics which enable him/her to proceed into subsequent general practice, specialty training, or research activities.
2. Specific Objectives:
-
Obtain a full history for a preschool and school-aged child:
- Engage, interview, and communicate skillfully with children and families.
- Obtain comprehensive information from parent/caregiver in a structured and organized method.
- Obtain comprehensive information from parent/caregiver in a structured and organized method.
-
Seek further relevant information related to differential diagnosis.
-
Perform examination of preschool and school-aged child:
- Perform a complete system-based physical examination.
- Explain how the age of the child influences the physical examination, including the approach to the patient, the sequence of the examination, and the specific components of the examination.
- Explain how age-appropriate behaviors, such as stranger anxiety, affect the ability of the examiner to perform the examination, and describe strategies to perform a successful examination.
- Recognize the value of observation as an important assessment tool.
- Determine when it is appropriate to perform a complete vs. a focused physical examination.
- Explain how physical exam findings have different clinical significance depending on the age of the child.
- Elicit, competently, system-based physical findings such as the gastrointestinal, respiratory, cardiovascular, hematological, neurological, endocrine, and renal system findings.
-
Develop a complete problem list and prioritize problems, taking into account the age of the child.
-
Combine problems where appropriate to develop a specific differential diagnosis for the patient’s combination of symptoms.
0-60 Months
5-19 Years
Procedural Skills
-
Measure vital signs, demonstrating knowledge of the appropriate blood pressure cuff size and normal variation in temperature depending on the route of measurement (oral, rectal, axillary, or tympanic). Identify variations in vital signs based on age of the patient and presence of disease.
-
Perform pulse oximetry and recognize its limitations:
- Ensure correct use and positioning of equipment.
- Give an account of the effect of peripheral blood flow on results.
-
Measure and plot on the charts the head circumference, weight, and height for an infant, older child:
- Demonstrate correct use of equipment and tools, e.g., positioning of tape on the head, and accurate plotting on age- and sex-appropriate percentile charts and calculation of body mass index (BMI).
-
Perform ear examination using the Otoscope.
Investigations
-
Choose appropriate laboratory and diagnostic tests, and be able to justify those decisions.
-
Interpret results of full blood count and blood film:
- Recognize normal values for children of different ages.
- Recognize important abnormal findings.
- Recognize important features from blood film.
-
Interpret results of blood biochemistry report:
- Recognize normal values for children of different ages.
- Recognize some important abnormal patterns such as abnormal liver function and abnormal renal function.
-
Interpret results of arterial blood gas report recognizing normal and abnormal findings.
-
Interpret microbiological analyses of specimens of urine, nasopharyngeal aspirate, and cerebrospinal fluid.
-
Interpret and explain the findings in plain x-rays of the chest, abdomen, skull, and musculoskeletal system in a child:
- Demonstrate systematic approach.
- Identify information such as name, date, and medical record number.
- Identify normal landmarks.
- Describe normal and abnormal findings.
Management and Communication
-
Describe the basic management and therapies of common general pediatric problems and of the different subspecialties.
-
Calculate and chart a pediatric drug dosage correctly using weight or surface area.
-
Recognize and use sources of recommended dosages and chart correctly.
-
Calculate and chart a child’s fluid requirement:
- Estimate oral fluid intake required for rehydration.
- Calculate and chart fluid requirements for a child requiring intravenous fluid therapy in different settings such as in shock and burns.
- Reconstitute an oral electrolyte solution.
-
Convey information about investigations required and investigation results in appropriate language and with accuracy based on evidence and verify patient/parent/caregiver understanding.
-
Observe performing cardiopulmonary resuscitation in children of all ages:
- Demonstrate correct technique.
- Identify correct equipment.
- Select different procedures for different ages.
-
Observe providing information to families and caregivers of chronically ill and disabled children.
-
Provide simple explanations of common conditions to parents and children such as asthma, croup, gastrointestinal illness, febrile seizures, otitis media, and upper respiratory tract infections.
-
Observe conveying information appropriate to levels of understanding of the receiver in appropriate linguistic terms.
-
Communicate effectively with families from disadvantaged backgrounds and from non-Arabic speaking backgrounds or of different cultural, ethnic, or religious backgrounds.
3-Objectives from Subspecialty Rotations:
1. Emergency Room:
- Identify the patient who requires immediate medical attention and intervention using the “ABCD” assessment.
- The student is expected to perform history and physical examination, formulate a differential diagnosis, and suggest laboratory and/or radiological evaluation after discussion with the attending on duty.
- Demonstrate knowledge of the acute management of common pediatric emergencies.
- Observe important pediatric procedures including: intubation, lumbar puncture, IV cannulation, inter-osseous needle insertion, cleaning and dressing of minor wounds and burns.
2. Nursery:
- Gather history from the parents and the medical record regarding the pregnancy, labor, and delivery, and interpret the information obtained.
- Demonstrate the ability to perform a complete physical examination of the newborn infant, noting key physical findings.
- Perform an assessment of gestational age using the Ballard Scale and describe how gestational age affects risks in the newborn period.
- Recognize patterns of illness in the newborn infant, including jaundice, respiratory distress, cyanosis, and lethargy. Discuss the major causes of each.
- Be familiar with the basic steps in the resuscitation of a newborn.
3. Outpatient Clinics:
- Compare and contrast the components of the history that should be obtained for different types of visits (e.g., first visit, acute care, health supervision).
- Determine when it is appropriate to obtain a complete medical history vs. a focused or interval history.
- Describe how to modify the interview depending on the age of the child, with particular attention given to the following age groups: toddler/preschooler, school-aged child, adolescent, including when to address questions to the child versus parent.
- Develop communication skills that will facilitate the clinical interaction and collaboration with children, adolescents, and their families.
- Become acquainted with the steps in the development of a differential diagnosis in a wide range of pediatric diagnoses in an ambulatory setting.
- Know when to employ screening during health supervision, including domestic violence screening, CBC, urinalysis, and bone profile.
4. LEARNING OBJECTIVES
Educational Methods for Theory Portion:
A variety of teaching-learning activities are planned:
-
A) Case-based discussion: 5 sessions.
-
B) Lectures: 33 lectures.
-
C) Tutorials: 6 sessions.
-
D) Seminars: 6 sessions.
-
E) College Clinical Training Day (CCTD): 4 days during the course (1 day per week). 15 sessions.
-
Series of lectures, tutorials, and seminars covering selected topics in pediatrics will be delivered to all students together during the whole course. Students are expected to come fully prepared for the seminar sessions. The tutors were encouraged to send the topic content to the students before the seminars to help them prepare.
-
Case-based discussions include case scenarios of various diseases, and students are encouraged to participate actively in the discussion.
-
College Clinical Training Day (CCTD): The objectives of CCTD are:
- Raise the students’ clinical competencies, to assure that the bedside teaching objectives have been achieved, to take prompt feedback from students regarding the past hospital days. Learning approaches include small group discussion, demonstration, doing, and immediate debriefing sessions. The day will be only practical, including but not exclusively simulations, simulators, standardized patients, clinical reasoning, etc., using manikins, stadiometers, infantometers, weighing devices, and growth charts.
TOPIC CONTENTS OF THE COURSE (PED 632)
TOPICS COVERED BY LECTURES AND TUTORIALS:
Introduction to History Taking For Children (L):
- To understand the differences in obtaining a medical history on a pediatric patient compared to an adult.
- To understand all the ramifications of the parent as historian in obtaining medical history in pediatric patients.
- To understand the appropriate wording of open-ended and directed questions, and appropriate use of each type of question.
- To obtain an accurate and complete history of pediatric patients in different age groups. (<1, 1-5 y., >5y).
Introduction to Physical Examination For Children (L):
Pediatric Endocrine:
- Assessment of Growth, Teething, and Skeletal Maturation and Use of Percentile Charts (L):
- Discuss the normal growth patterns from birth to adolescence.
- Recognize the normal growth indices in childhood.
- Discuss the factors affecting normal growth.
- Explain the importance of monitoring the growth of a child.
- Explain the use and interpretation of growth charts in the longitudinal evaluation of height, weight, and head circumference.
- Recognize abnormalities of growth that warrant further evaluation and discuss their basic causes (e.g., crossing lines on a growth chart, discrepancies among height, weight, and head circumference, microcephaly, and macrocephaly).
- Explain methods of assessment of bone age in children.
- Mention causes of delayed and advanced bone age in children.
- Recognize the sequence of premature teeth eruption in children.
- Mention causes of delayed teeth eruption.
- Approach to Short Stature (T):
- Recognize and define short stature.
- Present a brief list of differential diagnosis of short stature.
- Discuss the initial evaluation of a child with short stature.
-
Precocious & Delayed Puberty (L):
- Define delayed puberty in both boys & girls.
- Understand the pathophysiology of delayed puberty.
- Outline the investigations of delayed puberty.
- Outline the management strategies of delayed puberty.
- Define precocious puberty in both boys & girls.
- Signs of precocious puberty in both sexes.
- Understand the pathophysiology behind central & peripheral precocious puberty.
- Outline the investigations of precocious puberty.
- Outline the management strategies of precocious puberty.
-
Development (L):
- Discuss the normal developmental milestones.
- Describe age-related developmental changes in children and explain why they are important.
- Infant - Disappearance of primitive reflexes; changes in tone and posture; cephalocaudal progression of motor milestones during the first year; stranger anxiety.
- Toddler/child – Separation and autonomy in two to three-year-olds; sequence of language development; concept of school readiness.
- Explain the importance of monitoring the development of a child.
- Present a brief list of the differential diagnosis of developmental delay.
- Understand the concept of the multidisciplinary approach to the evaluation of a child with suspected developmental problems.
- Behavioral Disorders (L):
- Identify behavioral and psychosocial problems using the medical history and physical examination.
- Describe the typical presentation of common behavioral problems and issues in different age groups such as:
- Toddler: temper tantrums, breath-holding spell.
- School age: enuresis, encopresis, attention deficit disorder.
- Adolescent: anorexia nervosa/bulimia nervosa.
- Understand the process of behavioral modification, and know how to apply these principles to specific situations.
- Discuss the etiology, clinical presentation, and management of autism.
- Nutrition: Feeding of Infant (L):
- State the components of a routine dietary history for infants, children, and adolescents.
- Discuss the nutritional requirements in infancy, childhood, and adolescence.
- Explore the principles of infant feeding, including appropriate introduction of solids into the diet.
- Identify the major differences between human milk and commonly available formulas.
- Describe the advantages of breastfeeding and recognize common difficulties experienced by breastfeeding mothers.
- Recognize that chronically ill children may have special nutritional needs often requiring the assistance of a nutritionist.
- Nutritional Disorders (L):
- Protein Energy Malnutrition, Failure to Thrive (L):
-
Recognize nutritional factors that contribute to the development of childhood obesity and to failure to thrive.
-
Discuss the etiology, clinical presentation, and management of protein energy malnutrition including marasmus, kwashiorkor.
-
Define failure to thrive.
-
Classify failure to thrive.
-
Discuss the common etiologies that lead to failure to thrive.
-
Explore the clinical presentation and outline the initial investigations of FTT.
-
Outline the initial management strategies and discuss the goals of therapy.
-
Understand the concept of the multidisciplinary approach in the treatment of FTT.
- Rickets & Common Vitamin Deficiencies (L):
-
Understand calcium and phosphate homeostasis.
-
Discuss the common causes of rickets in children.
-
Describe the pathophysiology and clinical presentation of various types of rickets.
-
List the laboratory and radiological findings.
-
Explain the management of different types of rickets.
-
List the consequences of common vitamin deficiencies and excesses and indicate which vitamins and minerals may require supplementation in infants, children, and adolescents.
- Common Neonatal Problems (L):
- Discuss the transition from the intrauterine to the extrauterine environment, including temperature regulation, cardiovascular/respiratory adjustment.
- Discuss how gestational age can be assessed and identify key indications of gestational maturity, and discuss the effects of gestational age on the newborn infant.
- Recognize the major causes of prematurity and its common complications.
- List the information from the history of pregnancy, labor, and delivery and physical examination that have implications for the health of the newborn.
- Describe the presentation of the following common problems:
- Skin discoloration: Mongolian spots, salmon patches, erythema toxicum, and milia.
- Head and neck abnormalities: caput succedaneum, ranula, cleft lip, and palate.
- CNS disorders: myelomeningocele, spina bifida, and encephalocele.
- Musculoskeletal: dislocation of the hip and TEV.
- Birth Injuries (L):
- Recognize causes and pathogenesis of birth injuries.
- The presentation of common birth injuries including cephalohematoma, Erb’s palsy, clavicle fracture, fat necrosis, and facial injuries.
- Recognize the differential diagnosis of birth injuries.
- Recognize management of birth injuries.
- Common Respiratory Disease in Neonate (L):
- Enumerate the key components necessary for neonatal resuscitation.
- Discuss the clinical presentation and management of the following conditions:
- Neonatal respiratory distress syndrome (RDS).
- Meconium aspiration.
- Transient tachypnea of the newborn.
- Other Respiratory Diseases in Neonate (L):
- Discuss the clinical presentation and management of diaphragmatic hernia, congenital pneumonia, and pneumothorax.
- List the radiological findings of diaphragmatic hernia, congenital pneumonia, and pneumothorax.
- Neonatal Jaundice I/II:
- Define hyperbilirubinemia.
- Recall the physiological steps in the metabolism of bilirubin.
- List the key components from the history and physical examination in patients with jaundice.
- Differentiate between physiological and pathological causes of jaundice.
- Discuss the differential diagnosis of both direct and indirect hyperbilirubinemia.
- Define and enumerate the laboratory findings in cholestatic jaundice.
- List the commonest causes of cholestatic jaundice in infancy.
- Discuss the pathogenesis, clinical presentation, and outline the management of biliary atresia.
- Elaborate on the different treatment modalities in jaundice and list the common indications and side effects of each.
- Describe the most fatal complications of hyperbilirubinemia.
- Genetic (L):
- Understand the principles of genetic inheritance and define single gene (autosomal dominant, autosomal recessive, X-linked dominant, and X-linked recessive) and multifactorial inheritance and chromosomal disorders.
- List common prenatal diagnostic assessments (e.g., maternal serum screening, amniocentesis, chorionic villus sampling, and ultrasonography) and understand their use.
- Explain the use of the family history to construct a pedigree in the evaluation of a possible genetic disorder.
- List the indications for obtaining chromosome studies.
- Dysmorphology (L):
- Recognize the role of careful history-taking and physical examination in the evaluation of a patient with structural or developmental abnormalities (e.g., facial features, palmar crease, measurements, symmetry).
- Recognize the various genetic disorders and have a basic knowledge of the appropriate diagnostic tests and clinical course for common disorders such as: Trisomy 21, Trisomy 18, Trisomy 13, Turner syndrome, Klinefelter Syndrome, Marfan syndrome, Achondroplasia, and Williams syndrome.
Pediatric Cardiology
Acyanotic Congenital Heart Disease (L)
- Describe the clinical features that point to the presence of a congenital heart malformation.
- Describe the general classification of heart diseases in pediatrics.
- Differentiate cyanotic from non-cyanotic heart disease.
- Understand the anatomy and physiology of common acyanotic congenital cardiac defects: VSD, ASD, PDA, pulmonary stenosis, aortic stenosis, COA, HLHS.
- Discuss the clinical presentation and outline the management of acyanotic heart diseases: VSD, ASD, PDA, pulmonary stenosis, aortic stenosis, COA, HLHS.
Cyanotic Congenital Heart Disease (L)
- Define cyanosis and methods of detection.
- Mention causes and types of cyanosis in newborns.
- Understand the anatomy and physiology of common cyanotic congenital cardiac defects: TGA, TOF, tricuspid atresia, pulmonary atresia, Ebstein anomaly, TAPVD.
- Discuss the clinical presentation and outline the management of common cyanotic congenital cardiac defects: TGA, TOF, tricuspid atresia, pulmonary atresia, Ebstein anomaly, TAPVD.
Approach to the Cyanotic Infant (CBD)
- Outline methods to differentiate cardiac from non-cardiac causes of cyanosis.
- Formulate an appropriate approach to evaluate an infant with cyanosis.
- Discuss confirmatory diagnostic tools for cyanotic disorders in neonates or infants.
- Discuss the clinical presentation and outline the management of persistent pulmonary hypertension of the newborn.
Acquired Heart Diseases (L)
- List the common acquired heart diseases in pediatrics.
- Understand the etiology, symptoms, signs, diagnosis, and management of acute rheumatic fever and Kawasaki disease.
Respiratory System
Upper Respiratory Tract Infections (L):
- Recognize the etiology and clinical presentation of pharyngitis, tonsillitis, and otitis media.
- Discuss the management and complications of tonsillitis and otitis media.
Lower Respiratory Tract Infections (L):
- Discuss the causative agent, pathogenesis, clinical presentation, radiological findings, management, and complications of bronchiolitis.
- Discuss the common causes of pneumonia in normal infants and children.
- Describe the laboratory investigation, management, and complications of various types of pneumonia.
Pediatric Gastroenterology
Acute Diarrheal Diseases in Infancy (L):
- Explain the general classification of diarrhea.
- Describe the criteria for establishing a diagnosis of diarrhea.
- Identify the common etiologies, clinical presentation, laboratory findings, and management of acute diarrhea.
- Explain the major risks associated with diarrhea and identify the signs and symptoms that indicate high risk to the patient.
Chronic Diarrheal Disease in Children (L):
- Recognize the common causes of chronic diarrhea in infancy such as celiac disease, toddler’s diarrhea, lactose intolerance, giardiasis, cystic fibrosis, chloride losing diarrhea, and Crohn’s disease.
- Outline the basic laboratory investigations and management of chronic diarrhea.
- Discuss the pathogenesis, clinical presentation, laboratory findings, management, and complications of celiac disease and cystic fibrosis.
Hematology
Iron Deficiency Anemia and Megaloblastic Anemia (L)
- Describe the findings from the history, physical exam, and blood count that suggest a hematological disorder.
- Define anemia.
- Discuss and categorize the various etiologies of anemia in infancy and childhood.
- Classify anemia in infancy and childhood.
- Discuss briefly the pathogenesis, clinical presentation, and management of anemia due to:
- Nutritional deficiencies: iron, vitamin B12, and folate deficiencies.
Hemolytic Anemia (L)
- Discuss the pathogenesis, clinical presentation, complications, and management of sickle cell anemia, thalassemia, and hereditary spherocytosis.
- Discuss the pathogenesis, clinical presentation, complications, and management of G6PD deficiency.
Approach to Child with Anemia (T):
- Define a simple approach to the pale child based on age and clinical presentations.
- Outline the basic laboratory investigations and more specific investigations for a child with anemia.
Infection
Common Pediatric Viral Infections (L):
- Recognize the incubation period, mode of transmission, pathogenesis, clinical presentation, and management of the major viral pathogens of childhood including:
- Measles, mumps, rubella, roseola infantum, EBV, and erythema infectiosum.
- Provide guidelines for the management of these infections, including prevention.
Common Pediatric Bacterial Infections (L):
- Recognize the clinical presentation of common bacterial infections including: scarlet fever, H. influenza infection, tetanus, and pertussis.
- Provide guidelines for the management of these infections, including prevention.
Serious Pediatric Infections (L):
- Recognize the signs and symptoms of encephalitis and meningitis.
- Outline the proper management and prevention of these infections.
Pediatric Nephrology
Glomerulonephritis (L):
- Identify the clinical features that suggest renal or urinary tract disease.
- Discuss the clinical presentation of glomerular diseases in pediatrics.
- Relate historical, physical, and laboratory findings to glomerulonephritis.
- Develop an appropriate management plan for glomerulonephritis.
- Recognize clinical situations that mandate urgent intervention or consultation.
Nephrotic Syndrome (L):
- Relate historical, physical, and laboratory findings to nephrotic syndrome.
- Develop an appropriate management plan for nephrotic syndrome.
- Recognize clinical situations that mandate urgent intervention or consultation.
Approach to Hematuria (CBD):
- Define hematuria.
- Discuss the methods of detection of hematuria.
- Recognize the general classification of hematuria.
- Discuss the commonest causes of hematuria in pediatrics.
- Discuss the key components from the history and physical examination in evaluating a child with hematuria.
- Identify the distinguishing features between glomerular and non-glomerular causes of hematuria based on urine analysis.
- Formulate an appropriate management plan to evaluate an infant with hematuria.
- List the indications for renal biopsy in the evaluation of hematuria.
Approach to Proteinuria (T):
- Discuss the pathophysiology behind normal and abnormal protein excretion.
- Describe the different methods of measurement and detection of urinary proteins.
- Define and classify proteinuria.
- Discuss the various etiologies of proteinuria.
- List the key components from history and physical examination of a child with proteinuria.
- Explore the investigation and initial management plan for a patient with proteinuria.
Nervous System
Seizures in Pediatrics (L):
- Describe the features of the history and physical examination important to the evaluation of a child with a nervous system complaint.
- Common definitions in neurology (seizures, epilepsy, status epilepticus, aura, ictal, and postictal phase).
- Discuss and categorize the various etiologies of seizures in infancy and childhood.
- Describe the different types of seizure disorders in children.
- Discuss the clinical presentation of various epileptic syndromes in pediatrics.
- List the diagnostic criteria for the establishment of febrile seizures.
- Describe the general management and prognosis of febrile seizures.
Approach to Child with Seizure (T):
- Discuss the initial steps of evaluation of seizure in infancy.
- Provide a general outline for the management of seizures.
- List the common complications of seizures.
Evaluation of Abnormal Head Size (Hydrocephalus, Microcephaly, and Craniocynostosis) (L):
- Recall the normal head growth from infancy to childhood.
- Enumerate the common abnormalities in head size.
- Define microcephaly.
- Discuss and classify the different etiologies behind microcephaly.
- Identify the key components from the history and physical examination to formulate the differential diagnosis, including history of pregnancy, neonatal, and postnatal period.
- Explore the initial evaluation step of an infant with microcephaly.
- Define macrocephaly.
- Discuss and categorize the various causes of macrocephaly.
- Describe the initial laboratory investigations and radiological imaging required while evaluating a child with macrocephaly.
- Define and discuss the different types of hydrocephalus.
- Describe and categorize the various etiologies of hydrocephalus.
- Discuss the clinical presentation of hydrocephalus depending on the age.
- Identify the components from the physical examination that aid in the diagnosis.
- Outline the initial evaluation steps and discuss management strategies of hydrocephalus.
- Identify the indications for urgent CT scan imaging.
- Outline the initial evaluation steps and discuss management strategies of craniocynostosis.
Pediatric Emergency
Fluid and Electrolyte Disturbance (L):
- Recall the physiological process that maintains fluid and electrolyte homeostasis.
- List the daily water and electrolyte requirements for children of all ages.
- List the factors that increase daily fluid requirements.
- Recognize the causes and types of dehydration.
- Identify the physical and laboratory indications of dehydration.
- Discuss fluid management in pediatrics, including calculation of the deficit, maintenance fluid, and ongoing losses.
- Identify the indications for the use of oral rehydration therapy and IV solutions, the proper constitution of rehydration fluids, and the benefits and limitations of the therapy.
- Identify the common electrolyte imbalances in pediatrics (sodium and potassium).
- Describe a common clinical scenario in which each might develop.
- Discuss the common causes and outline the management of electrolyte disturbances in pediatrics.
- Know the conditions in which fluid administration may need to be restricted (such as the syndrome of inappropriate ADH secretion, congestive heart failure, or renal failure).
Acid-Base Disturbance (L):
- Recall the physiology involved in the acid-base balance of the body.
- Describe the normal values and factors that influence normal variables.
- Identify abnormal values and their interpretation.
- Describe and list the differential diagnosis of both respiratory acidosis and alkalosis.
- Describe and list the differential diagnosis of both metabolic acidosis and alkalosis.
5. Clinical Teaching:
1. Formal Teaching:
Fifteen (15) bedside teaching sessions are conducted by teaching staff during the course. Usually, cases are prepared by students who present them to the group for discussion to demonstrate the relevant historical data and physical findings. Activity takes place from 10:00 – 12:00 PM.
Students will be divided into groups to be posted into different hospitals for them to swap postings at a certain time of the cycle.
2. ER, OPD, Nursery & Ward Rotations:
During rotations, students in each subgroup are divided into small groups of 3-4 students each. They rotate through: Ward, ER, OPD, or Nursery (level 1 and 2 only).
During the ward rotation, each student should follow 1-2 patients at a time. The student is expected to function as a “sub-intern” with direct involvement in patient care. They are expected to clerk patients, observe different aspects of inpatient care, and share in the rounds with the team. In OPD or Nursery or ER sessions, each subgroup is divided into 2, each half attends with a consultant.
Topics Covered in College Clinical Training Day (CCTD):
-
Measure weight, height, and head circumference and plot on growth charts (manikin). (Skill & Seminar):
- Measure and plot on the charts the head circumference, weight, and height for an infant, older child:
- Demonstrate correct use of equipment and tools, e.g., positioning of tape on the head, and accurate plotting on age- and sex-appropriate percentile charts and calculation of body mass index (BMI).
- Explain the use and interpretation of growth charts in the longitudinal evaluation of height, weight, and head circumference.
- Recognize abnormalities of growth that warrant further evaluation and discuss their basic causes (e.g., crossing lines on a growth chart, discrepancies among height, weight, and head circumference, microcephaly, and macrocephaly).
-
Bedside abdomen assessment skills in simulation system (manikin).
-
Bedside cardiac assessment skills in simulation system (manikin).
-
Bedside respiratory assessment skills in simulation system (manikin).
-
Demonstration of urine sample collection, using and interpretation of urine dipstick. Skill.
-
Demonstrate how to do a case report and case presentation, examples of 3 ideal case presentations. Tutorial.
-
Obtaining a medical history for a pediatric patient from a role player. CBD skill.
-
Physical examination for children (pitfalls in OSCE). Seminar.
-
Data interpretation part 1 (x-ray, CSF, blood gases, hematology, growth charts). Seminar.
-
Data interpretation part 2 (urine, LFT, electrolytes, renal profile). Seminar.
-
Slides show practice and spot diagnosis. Part 1 (syndromes, pedigree). Seminar.
-
Slides show practice and spot diagnosis. Part 2 (developmental, nutritional, skin). Seminar.
-
Case scenarios practice and management (seminar).
-
Neonate with respiratory distress (CBD).
-
Neonate with jaundice (CBD).
-
Approach to the cyanotic infant (CBD).
-
Approach to hematuria (CBD).
3. Medical Skills Application (Skill Lab):
- Observe IV cannulation and describe the correct technique.
- Observe performing urinary catheterization of infants.
- Observe lumbar puncture technique, describe the procedure, and explain safety with infants and children.
- Observe performing intra-osseous needle insertion on model/mannequin.
- Adopt suitable measures for safety and infection control.
- Demonstrate an ability to perform immediate first-aid procedures for common life-threatening conditions (Pediatric Basic Life Support & Pediatric Choking Treatment).
4. Attending the Continuous Medical Education in the Department:
(See attached schedule)
NOTES:
- Students who are doing ward and those who are having clinical sessions, except those who are preparing cases, are required to attend the morning report at 8:00 in the Pediatric Seminar Room.
- Each student should:
- Wear a white coat.
- Wear his/her I.D.
- Bring his/her own equipment.
- Dress according to the dress code assigned by the college.
5. Methods of Assessment:
During each rotation, medical students will be evaluated by: i. Theory (30 marks)
- Assessment of knowledge (theoretical) shall be performed through written examinations by ALMAAREFA College as outlined below:
- At the middle of each specialty rotation, there will be one theoretical examination (mid-block) by 60 MCQ (15 marks).
- At the end of each specialty rotation, there will be one theoretical examination by 60 MCQ (15 marks).
- It should be emphasized that examinations are based on the intended learning objectives (ILO) of the course and the reference books defined by Almaarefa colleges for each specialty. Each MCQ will last for 1.5 minutes.
ii. Clinical rotation assessment (70 marks)
Marks Distribution:
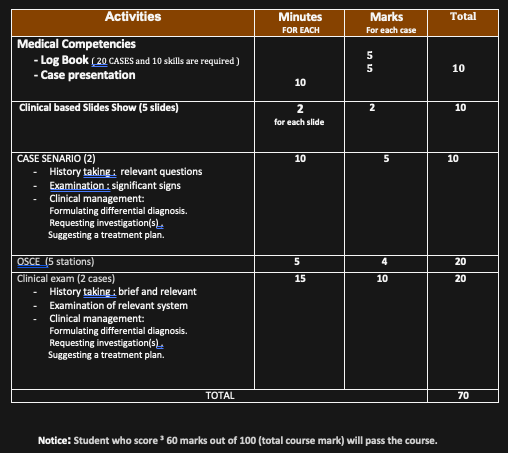
Notice: Students who score ≥ 60 marks out of 100 (total course mark) will pass the course.
6. Attendance:
Students are required to attend ALL activities.
- Students should notify any difficulties relating to attendance to their supervisor.
- In the clinical attachments and rotations, attendance is expected to be 100%. This includes the scheduled teaching sessions (seminars, clinical tutorials, lectures, and bedside teaching sessions) as well as the clinical attachments with the teams/subspecialties assigned.
- It is the responsibility of every student to sign in the attendance sheet.
- The attendance sheet will be placed on the front desk for the first 15 minutes of each and every session/lectures, etc., and to be collected by the administrative assistant.
- Failure on the part of the student to sign-in renders them absent for the entire period.
- Latecomers, who failed to sign-in, are also considered absent.
- Students are responsible for describing briefly their daily activities/cases on the attendance form.
- The attendance form should be submitted EVERY Wednesday to the Department.
The overall attendance will be calculated by gathering the student total attendance. The bylaws of the College of Medicine will be applied whenever the attendance records are less than 75%. A letter regarding the concerned student will be sent to the Vice Dean of Academic Affairs, and the student will not be allowed to take the final examination.
RECOMMENDED BOOKS FOR THE PEDIATRIC COURSES
- A. Illustrated Textbook of Pediatrics 6th edition, 2021 by Tom Lissauer, Will Carroll.
- B. Nelson Essential Pediatrics 9th edition 2022.
- C. Pediatric Clinical Examination Made Easy 6th edition, 2017 By Gill and O’Brien.
- D. Manual of Clinical Pediatrics (for Medical Students and Postgraduate Doctors) Edited by Dr. Mansour N. Al Howasi. 8th edition 2018.
- E. Nelson Text Book of Pediatrics 22nd edition, 2024 by Kliegman & St. Geme.