DR H M ABDELRAHIM
OBJECTIVES
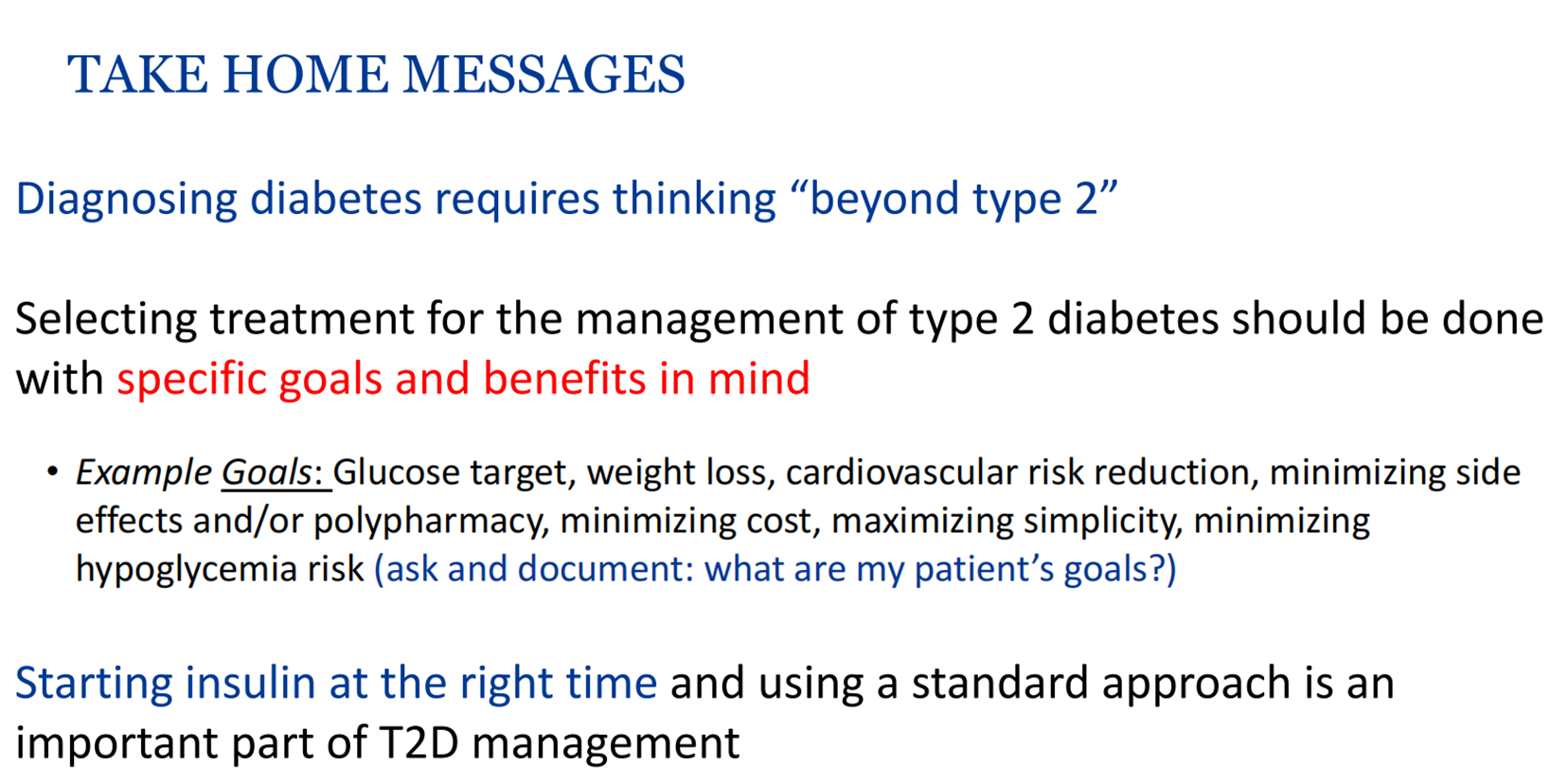
• Review basics of diagnosis and when to think beyond type 2 & type 1 DM
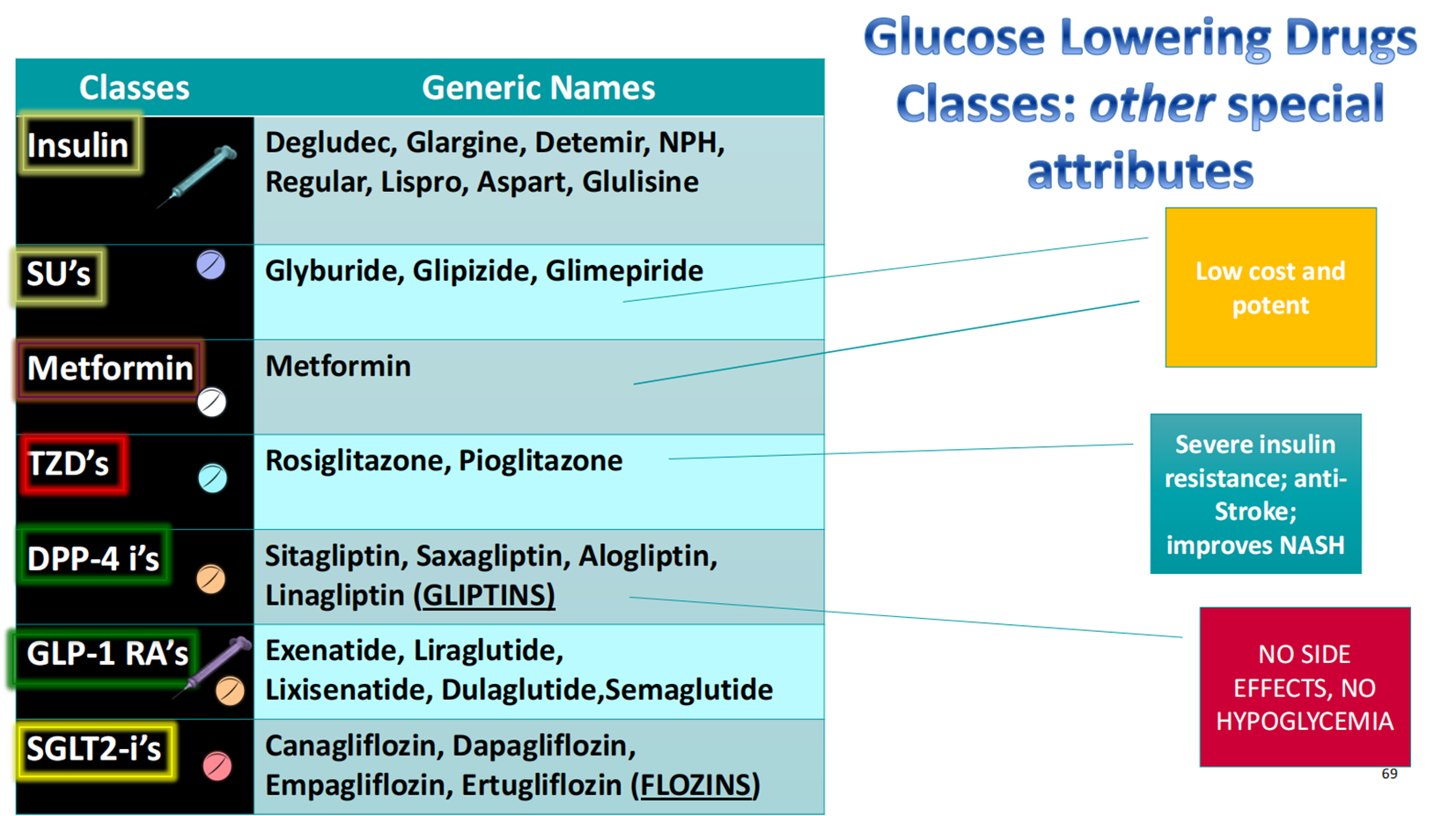
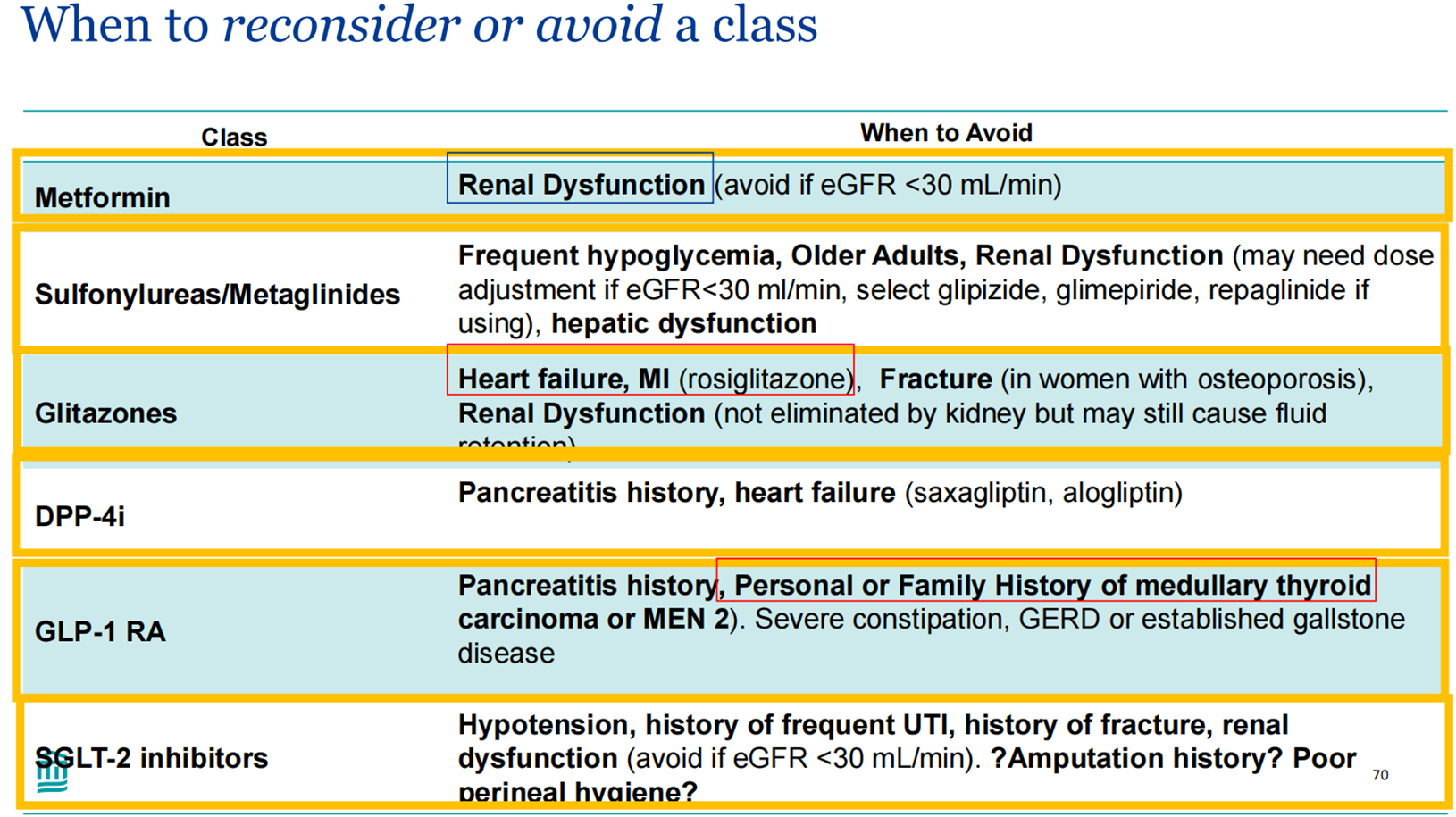
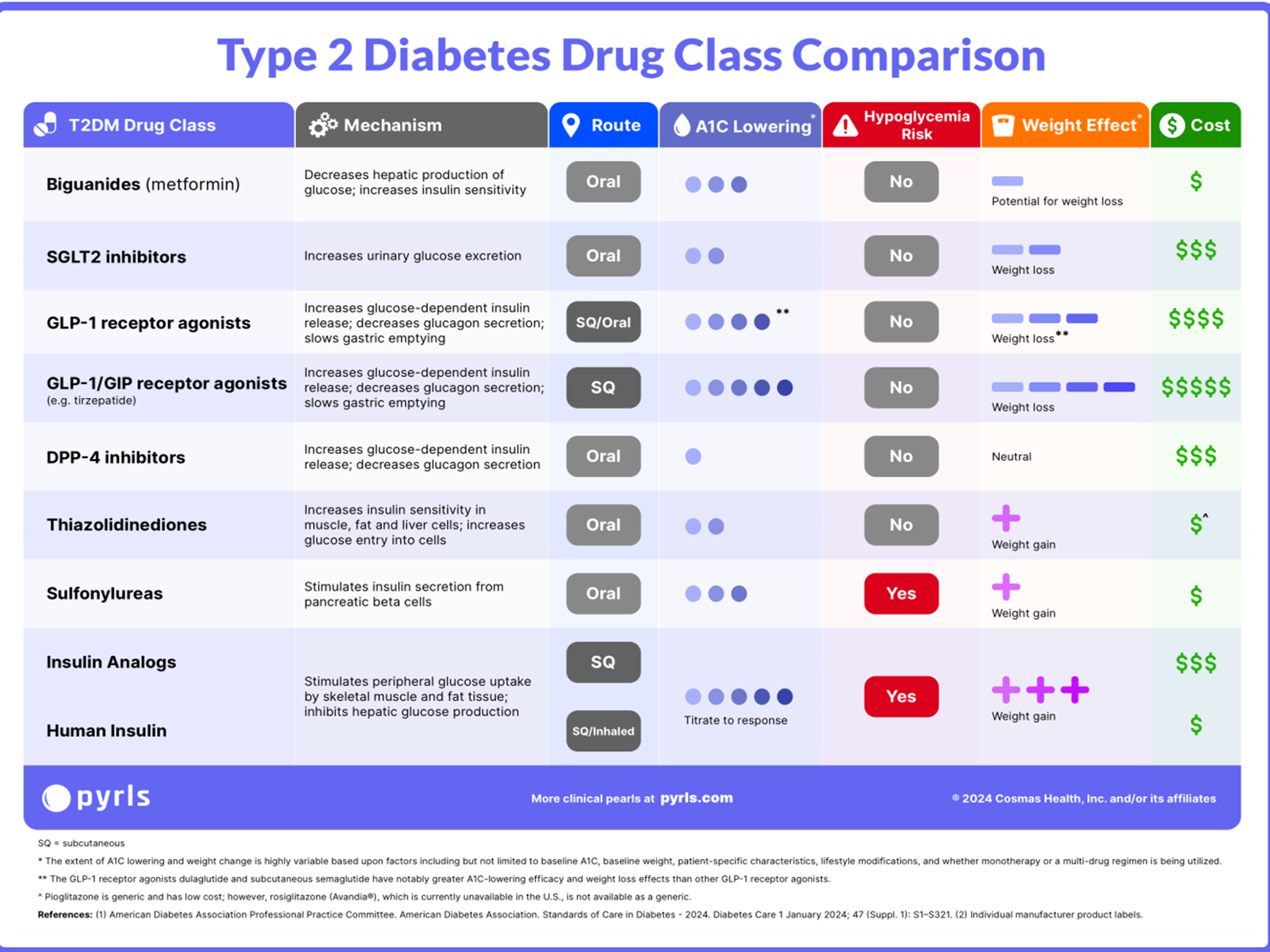
• Understand how to prescribe the available noninsulin pharmacologic therapies for type 1 & 2 diabetes
• Learn how to individualize therapeutic strategies for type 2 diabetes based on comorbidities, goals as well as concerns and side effects
Diabetes - Diagnosis & Classification
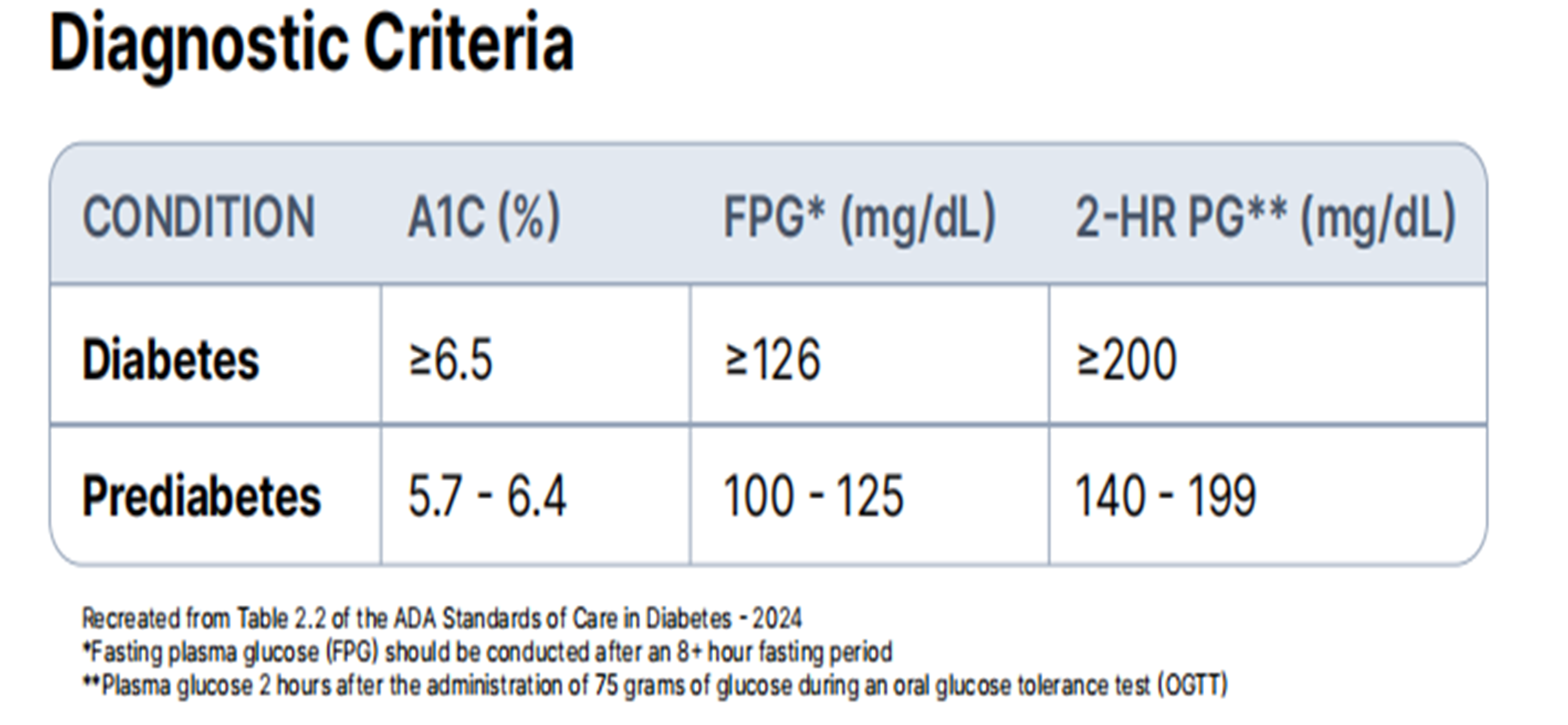
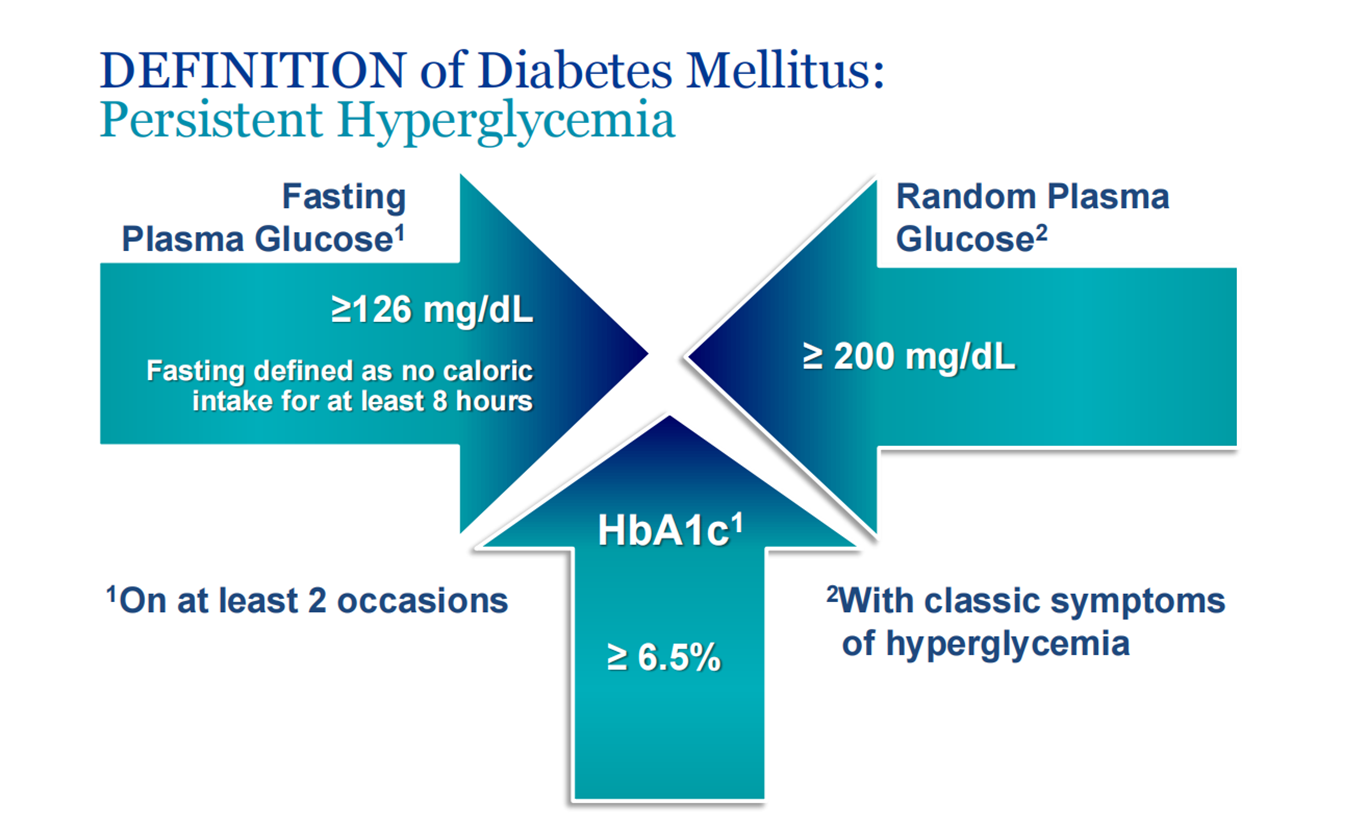
Diagnosis of Diabetes with any of :
- Fasting glucose ≥ 7mmol/L (Prediabetes: 6.1-6.9) OR
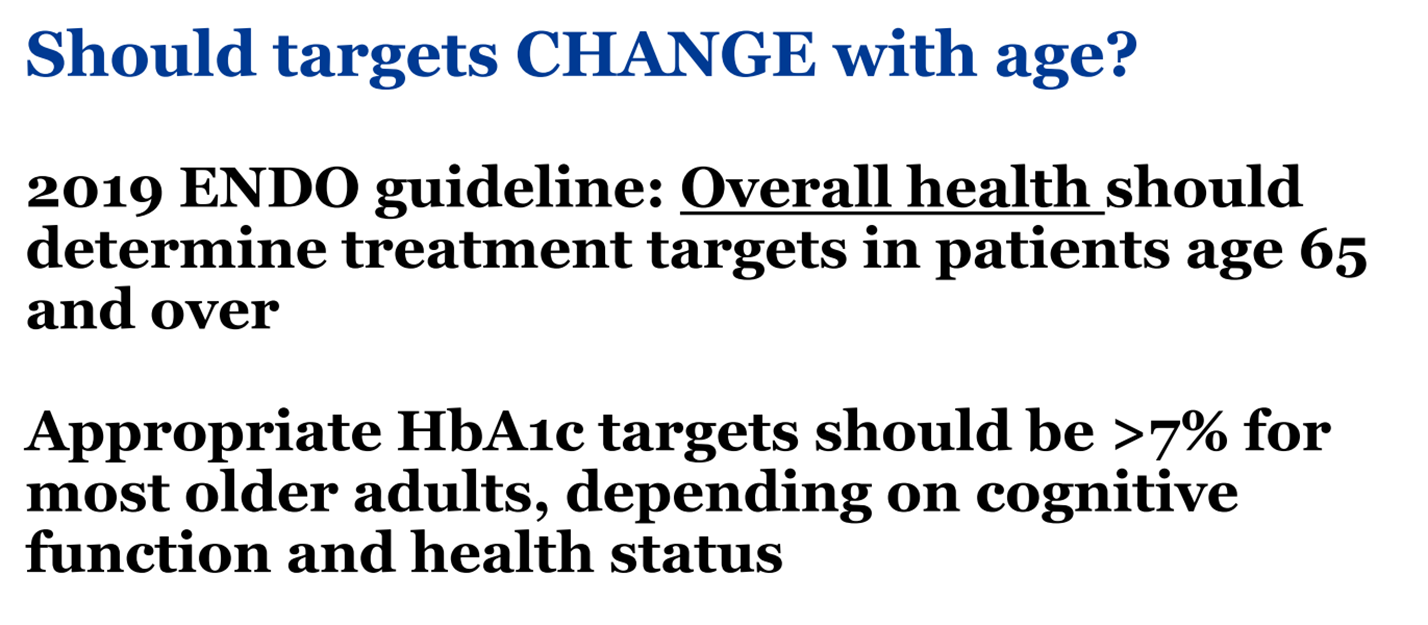
- HbA1c ≥ 6.5% (Prediabetes: 6.0-6.4%) OR
- 2h 75g OGTT ≥ 11.1 mmol/L (Impaired glucose tolerance: 7.8-11.0) OR
- Random glucose ≥ 11.1 mmol/L
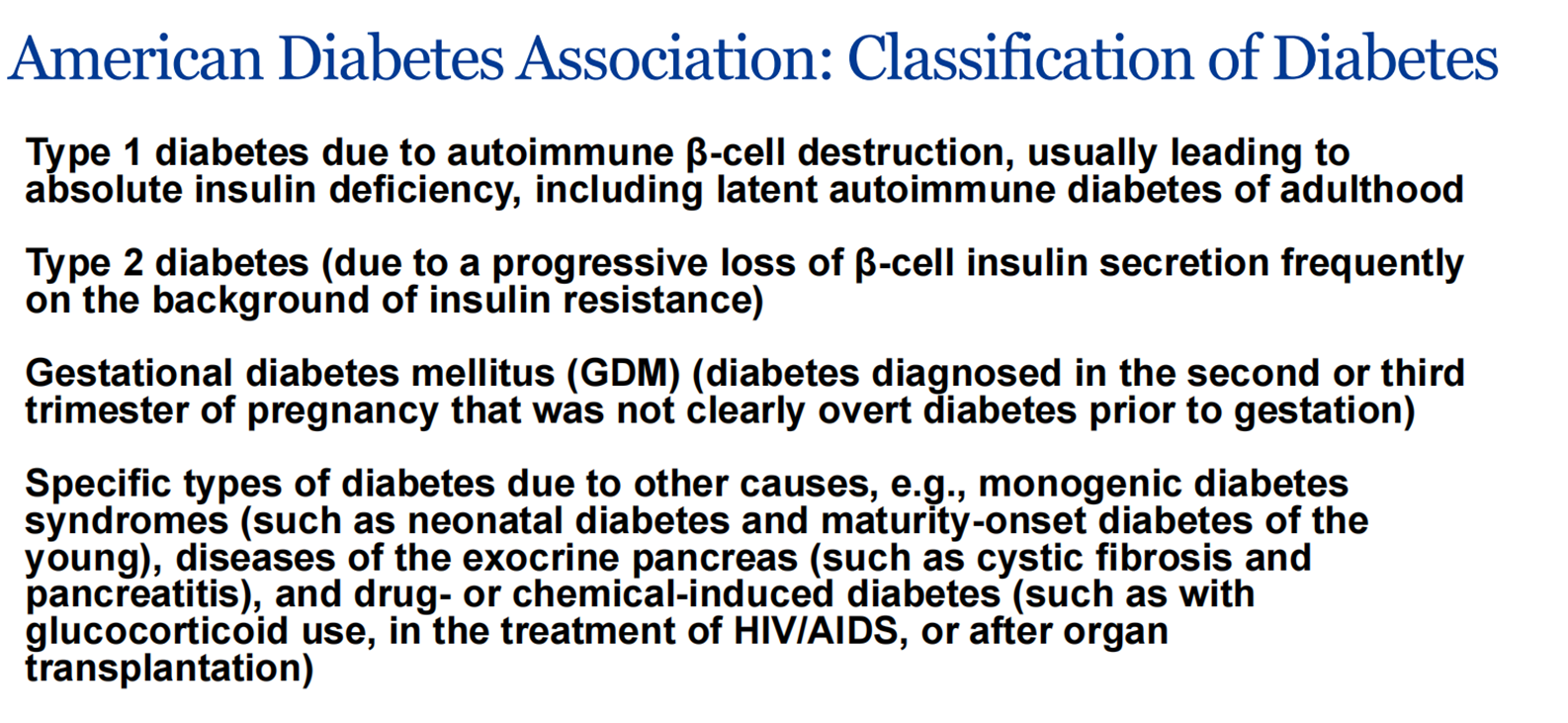
Type of Diabetes:
-
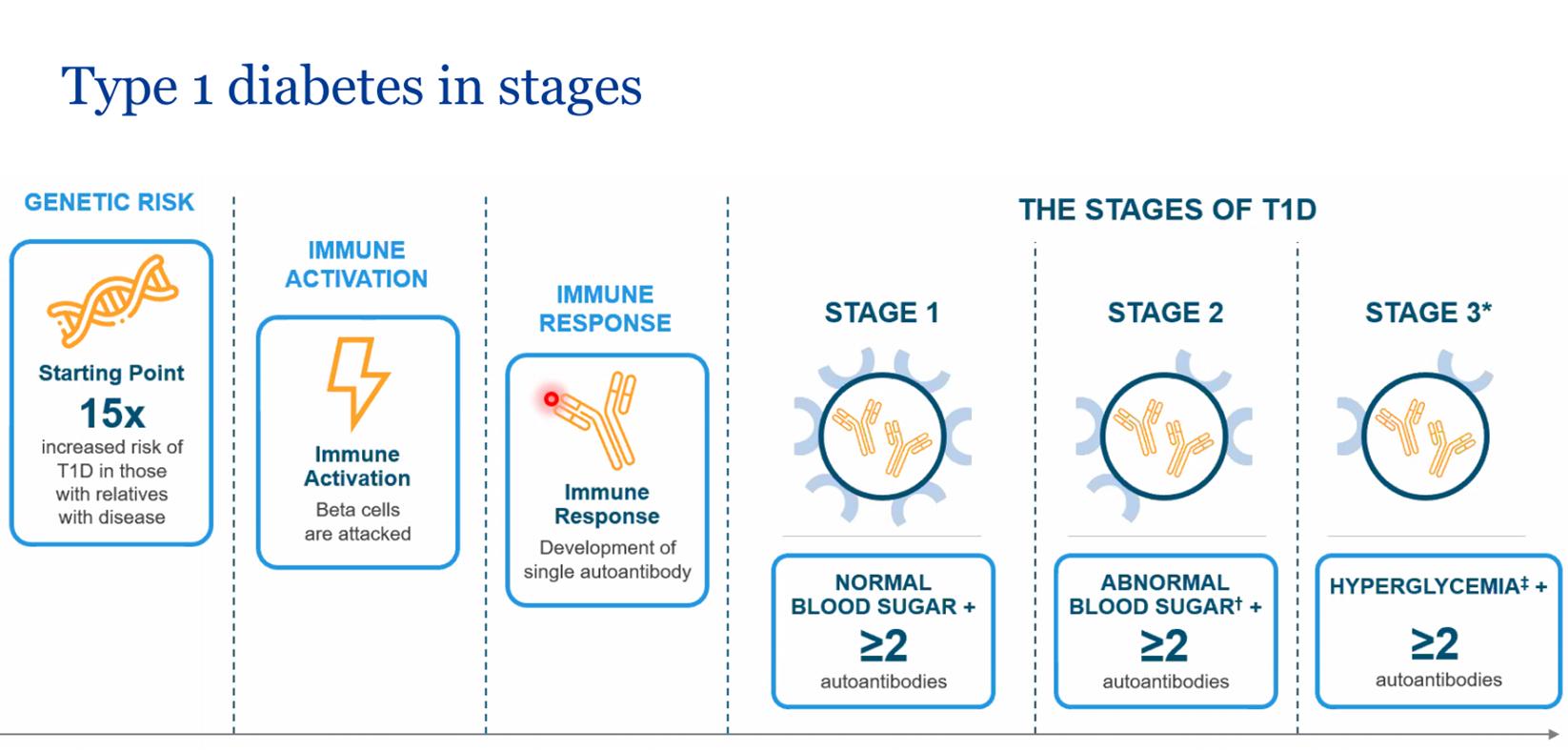
Type 1: insulin deficiency (pancreatic β cell destruction), DKA prone, Usually Anti-GAD/Anti-Islet Cell +
-
Type 2: insulin resistance (tissue resistance, secretory defect), metabolic syndrome
-
Latent autoimmune diabetes in adults (LADA): type 2 diabetes who also have immune-mediated loss of pancreatic β cells
-
Monogenic: familial autosomal dominant mutation leading to beta cell defects, neonatal or <25 yo
-
GDM: glucose intolerance during pregnancy
 #Z
#Z
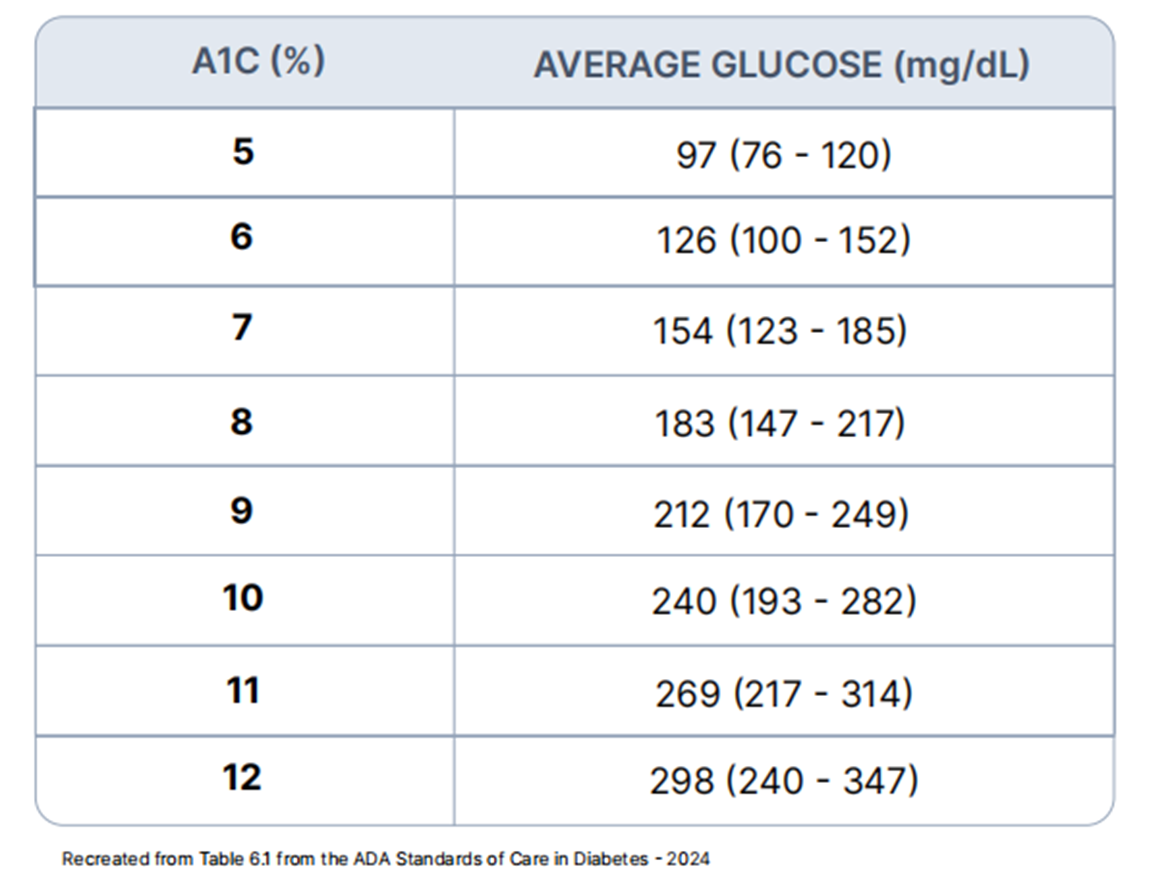
Overview of Hemoglobin A1C
-
Before discussing the hemoglobin A1C (A1C) lab value itself, it is important to understand the relationship between A1C and hemoglobin. Hemoglobin is an iron containing transport protein found in red blood cells.
-
Over the lifespan of red blood cells (~120 days) the hemoglobin protein becomes glycated (chemically linked to sugar).
-
The greater the concentration of glucose in the bloodstream, the greater amount of hemoglobin becomes glycated. The A1C test is a measurement of the percentage of glycated hemoglobin in the bloodstream.
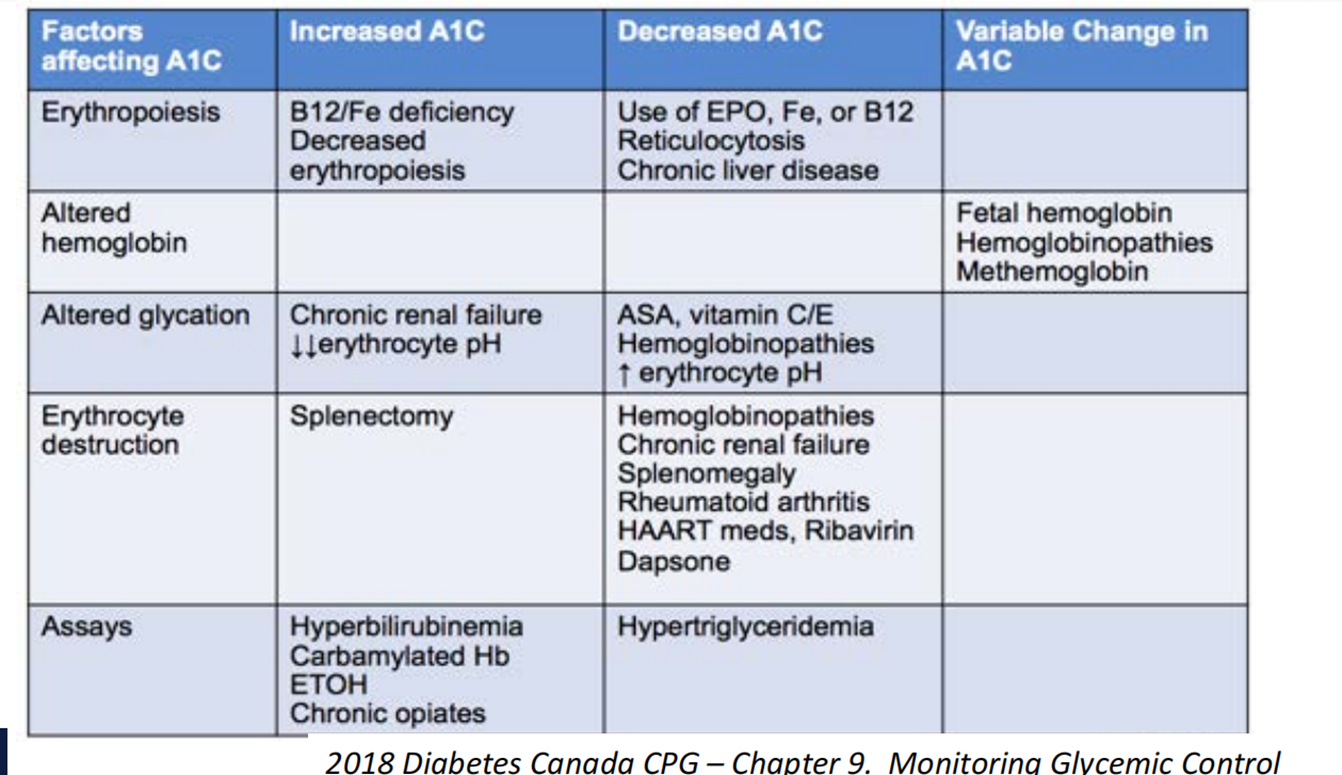
Limitations of Hemoglobin A1C
-
It is important to note that hemoglobin A1C (A1C) is an indirect measure of a patient’s average blood glucose levels. It does not provide information regarding glycemic variability (i.e., the frequency of hyper- and hypoglycemia) which is why assessing a collection of plasma glucose levels in addition to A1C is necessary to most effectively evaluate glycemic control.
-
Additionally, hemoglobin abnormalities may falsely increase or decrease A1C lab values. This should be considered when the reported A1C value(s) do not correlate with the patient’s plasma glucose levels.
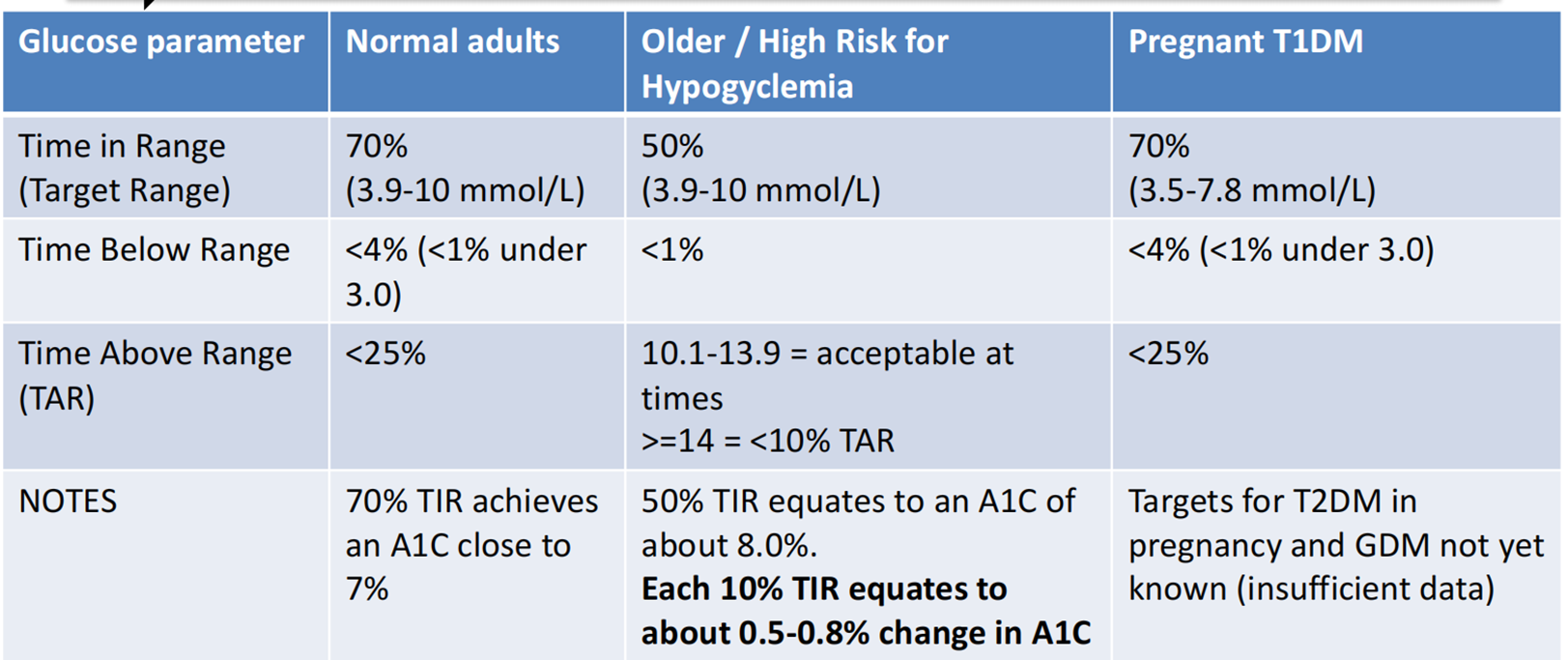
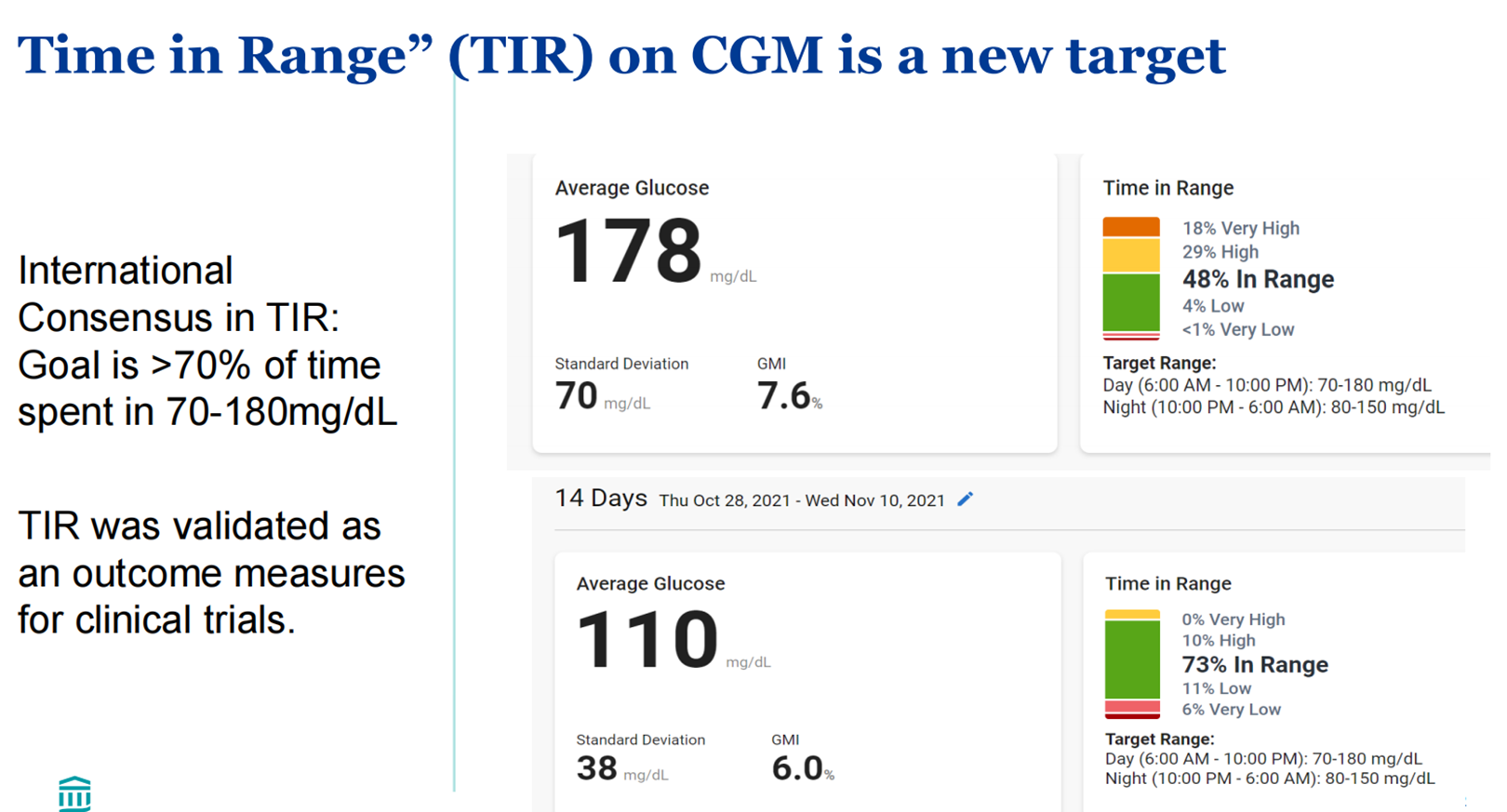
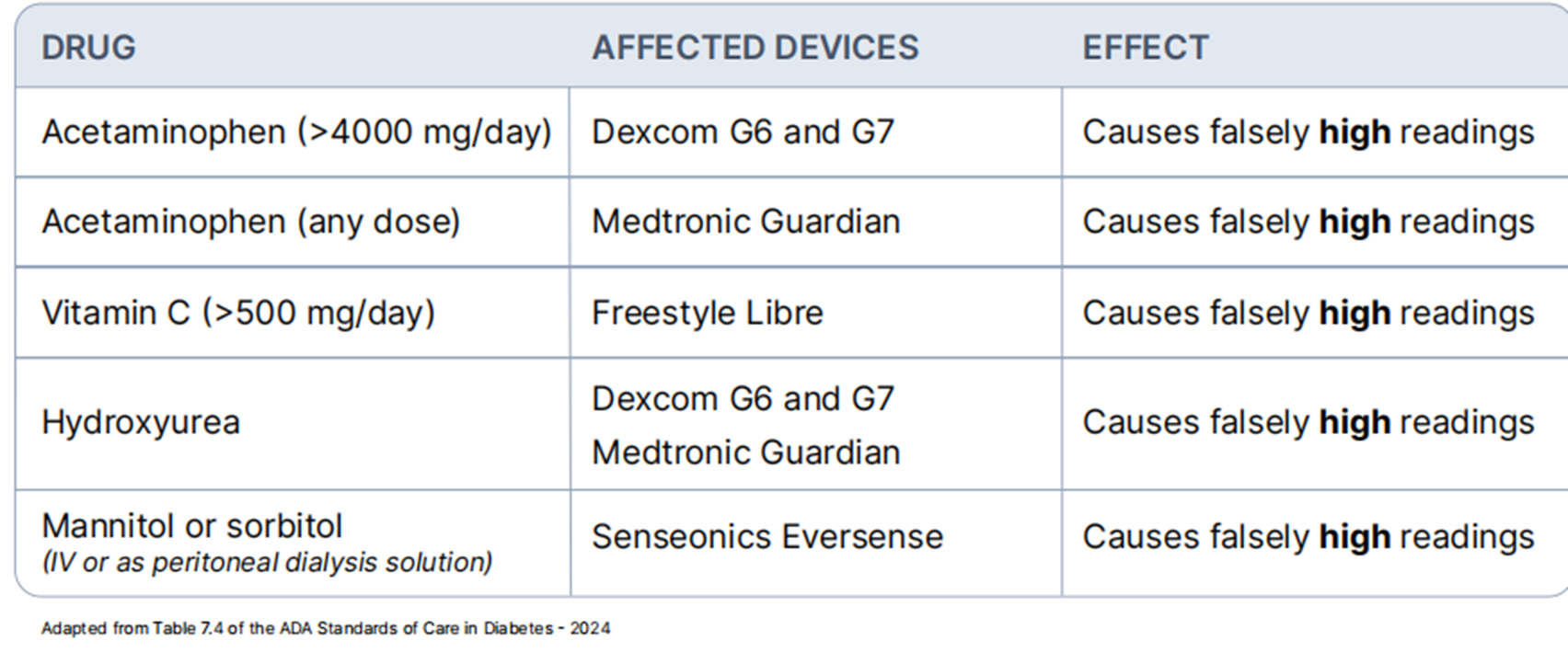
Continuous glucose monitor (CGM) – Targets Z.
(timebelowrange; hypoglycemia ---- X <25%)
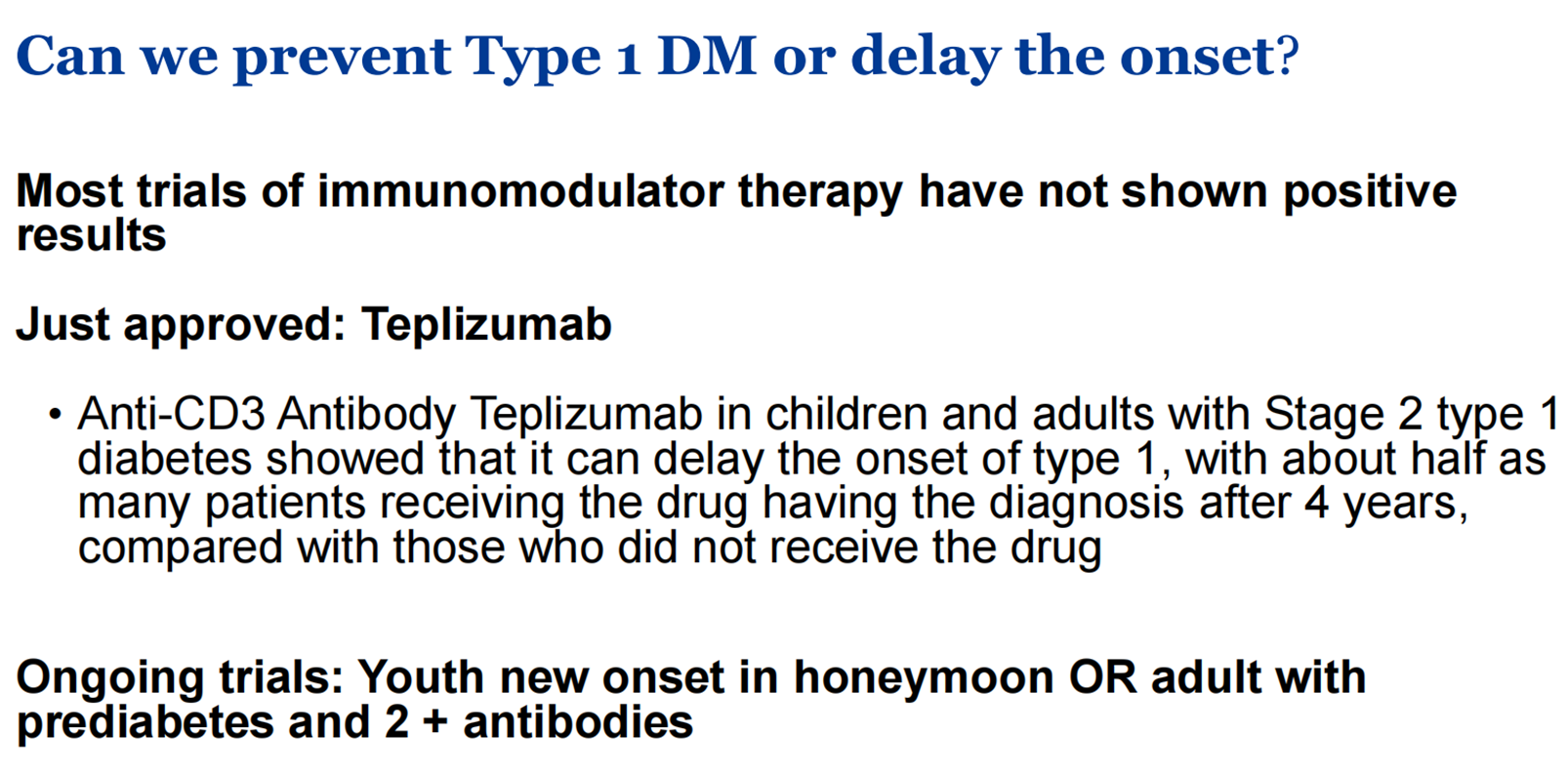
Type 1 Diabetes Management
Benefits of Adding CGM to BBI or CSII Adding Continuous Glucose Monitoring (CGM) w high sensor adherence can
- ↓ A1C with no increase in hypoglycemia
- ↑ QOL, diabetes distress, fear of hypoglycemia and treatment satisfaction
Note: Benefits of CGM are only seen when patients are actually wearing the sensor/CGM at all times = high sensor adherence (>70% in 14d period)
MDI (Multiple Daily Injections) Regimen Tips Z
- High glucose? Look at the dose before…
- High fasting glucose? May need to increase bedtime basal
- High pre-lunch glucose? May need to increase breakfast bolus
- Exception is GDM where targets are post-prandial, so look at the bolus at that meal
MDI (Multiple Daily Injections) Regimen Tips
• Ratio Basal-bolus
- – Individualized, there’s no recommended ratio
- – e.g. 50:50, 60:40, 40: 60 • Some Math • Insulin Sensitivity: 100/total daily insulin dose • Carb ratio : 500/total daily insulin dose • In Hospital Situations
- – Targets BG <12
- – Glucocorticoids, TPN
Nocturnal Hypoglycemia
- May lower basal
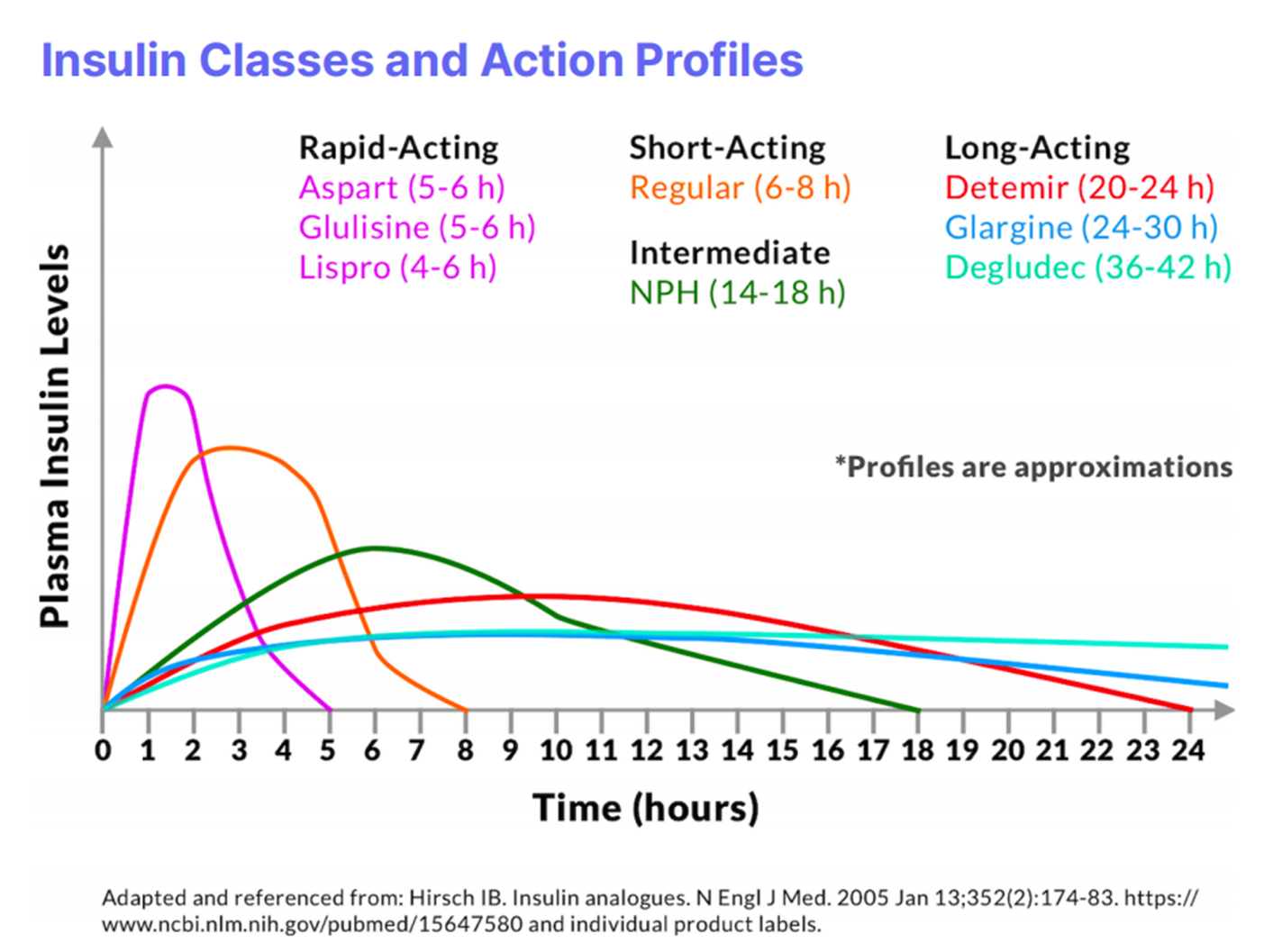
- Use ultra long acting basal (e.g. Tresiba (insulin degludec) –Note make dose changes every )
- May introduce a mixed meal bedtime snack
- Obtain history re: dinner and dinner bolus
Type 1 Diabetes – Autoimmune Screening
-
Autoimmune thyroid disease develops in 10% (up to 30% of females) – Check TSH, anti-TPO Ab at diagnosis and q2-5 years thereafter
-
Autoimmune adrenal insufficiency is rare – Screen if symptoms, unexplained hypoglycemia
-
Celiac disease in about 5%, asymptomatic – Screen if any symptoms, including iron deficiency, unexplained hypoglycemia, vitamin D deficiency, osteoporosis
Type 2 Diabetes Management
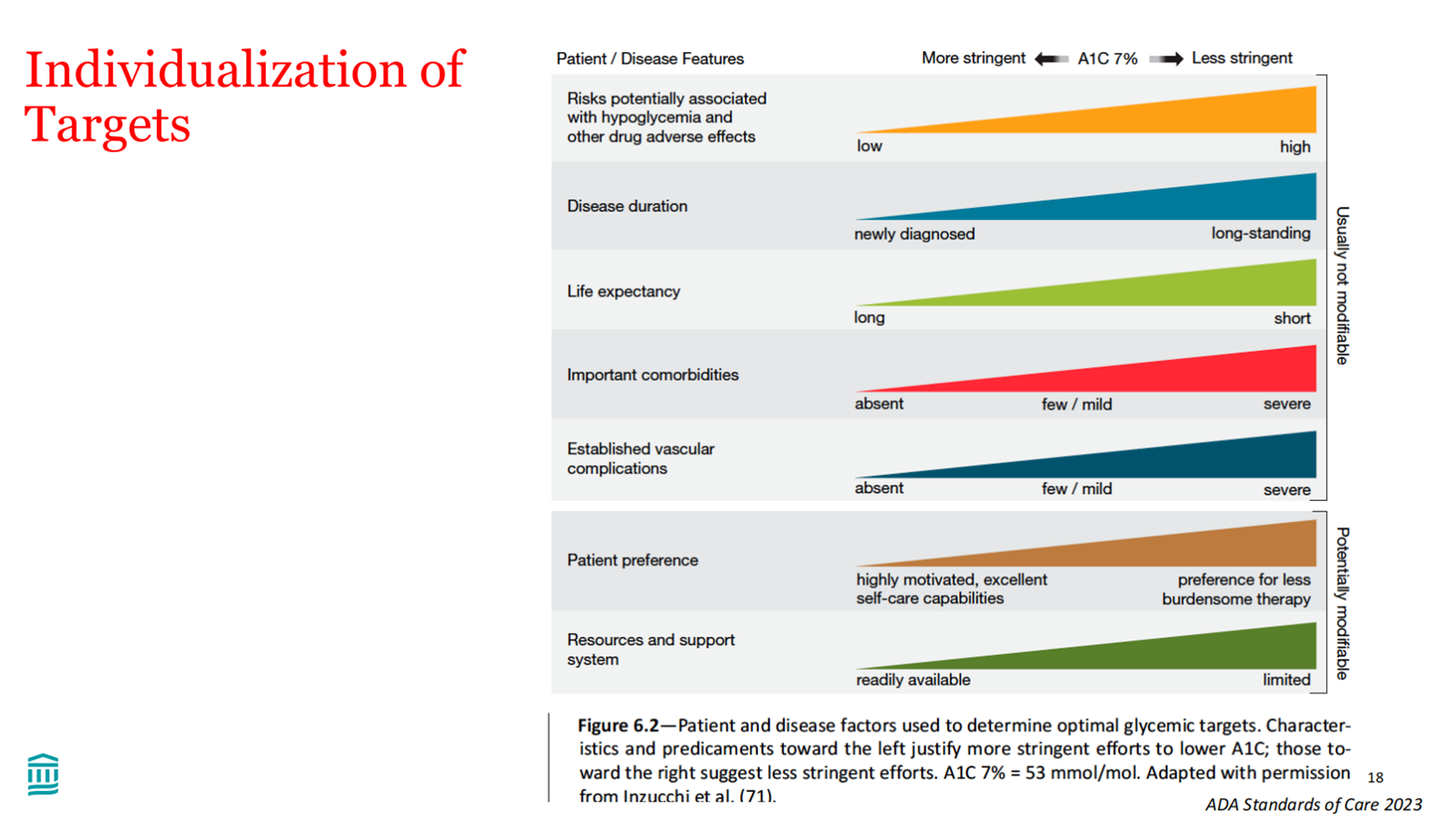
T2DM Treatment: At Time of Diagnosis
-
Non-pharmacological management (refer to Diabetes Education Centre, Set A1C target, assess CV status, smoking cessation etc)
-
Diet/Lifestyle changes for all
-
Metformin if A1C ≥ 1.5% above target at diagnosis – Insulin + Metformin if symptomatic hyperglycemia and/or metabolic decompensation
-
Reassess in 3-6 months
Metabolic Decompensation
What does “symptomatic hyperglycemia with metabolic decompensation” mean? Suggests a state of relative or absolute insulin deficiency.
- • Polyuria
- • Polydipsia
- • Blurry Vision
- • ***Unintentional Weight loss ***
- • Volume depletion
- • Ketosis
- • HHS/DKA
- • SHOULD BE STARTED ON INSULIN +/- metformin until glycemic control is achieved! (then you back off insulin if you can, while adding on oral agents)
±
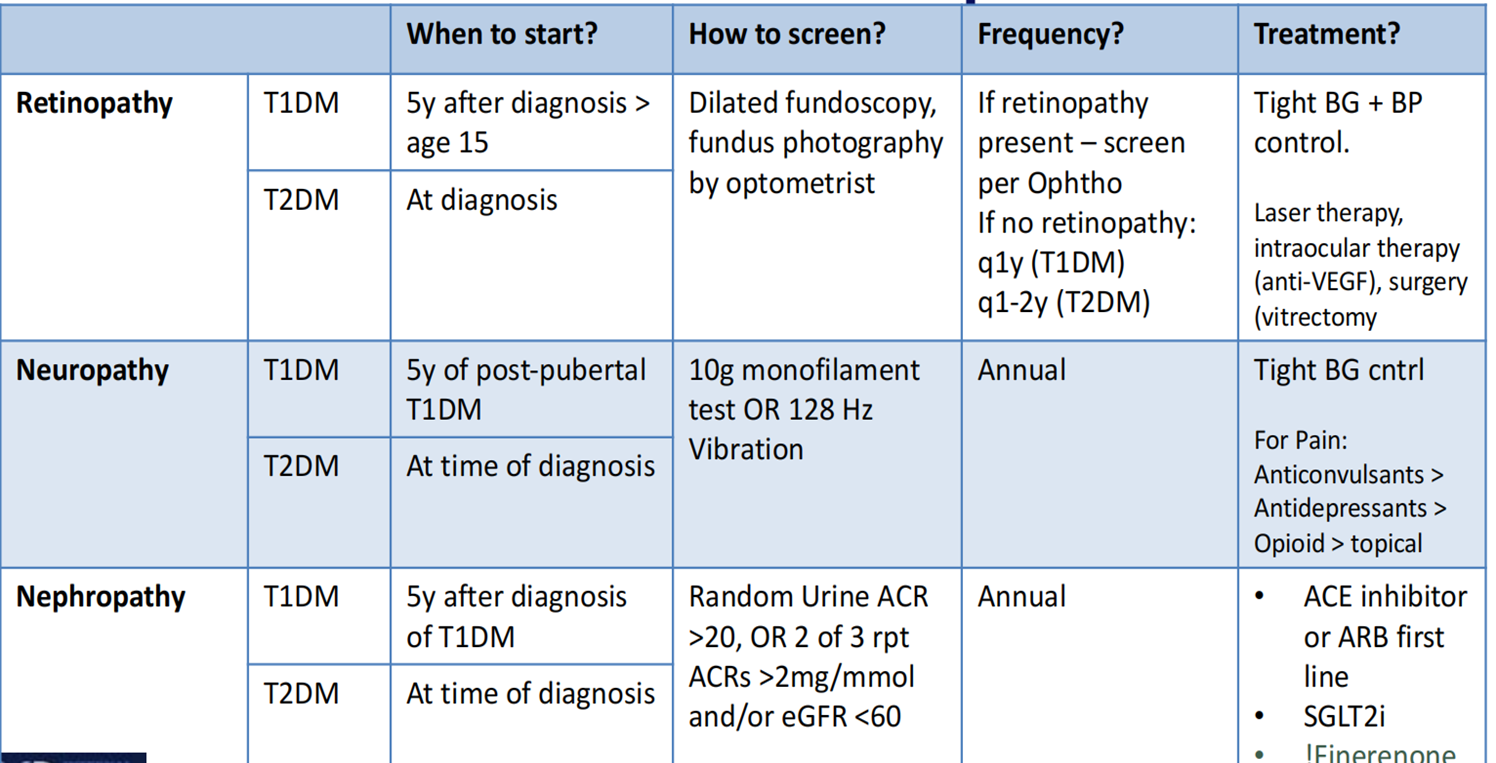
Microvascular Complications