Trauma
Patient Presentation
- Age: 2 year-old girl
- Mechanism of Injury: Fell from bed at 4:30 a.m., landing on a glass nightstand which shattered.
- Initial Assessment by Mother: No bruises or bleeding immediately after the fall.
- Subsequent Observations:
- Noticed rubbing the R eye several times the next morning.
- Keeps the R eye closed by squinting constantly.
- Will not allow mother to look at the eye.
- Past Ocular History: No history of ocular surgery, trauma, amblyopia, or strabismus.
- General Health: Healthy child, born at term. Negative for blinding diseases.
- Social History: Lives with mother, no smoking in the house.
- Medications/Allergies: None.
- Recent Illnesses: None.
Ocular Examination
- Visual Acuity (cc):
- OD: Open eye to command but keeps eye closed most of the time. Central, unmaintained.
- OS: Central, steady and maintained.
- IOP (tonoapplantation):
- OD: Not performed.
- OS: Not performed.
- Pupils:
- Irregular, peaked OD.
- Round OS.
- No APD.
- Extraocular Movements: Full OU. No nystagmus.
- Confrontational Visual Fields: Not performed.
- External: Normal-appearing orbital structures, both sides.
- Slit Lamp:
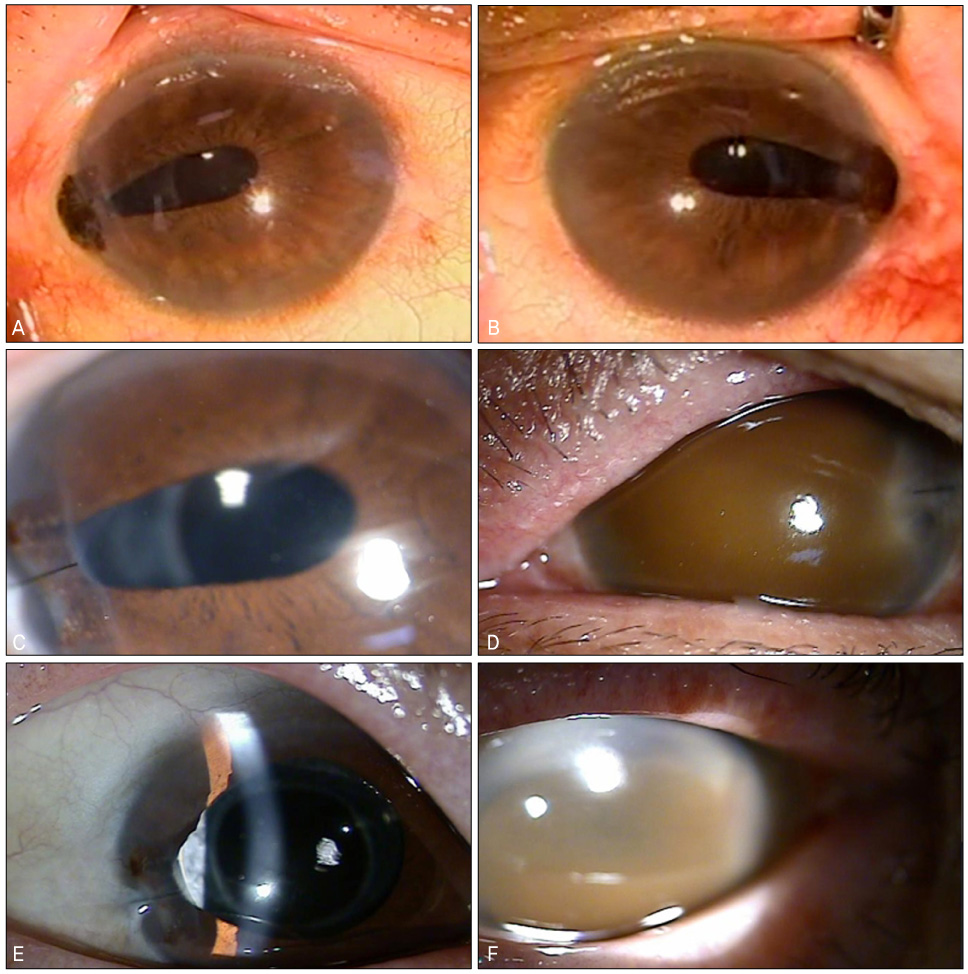
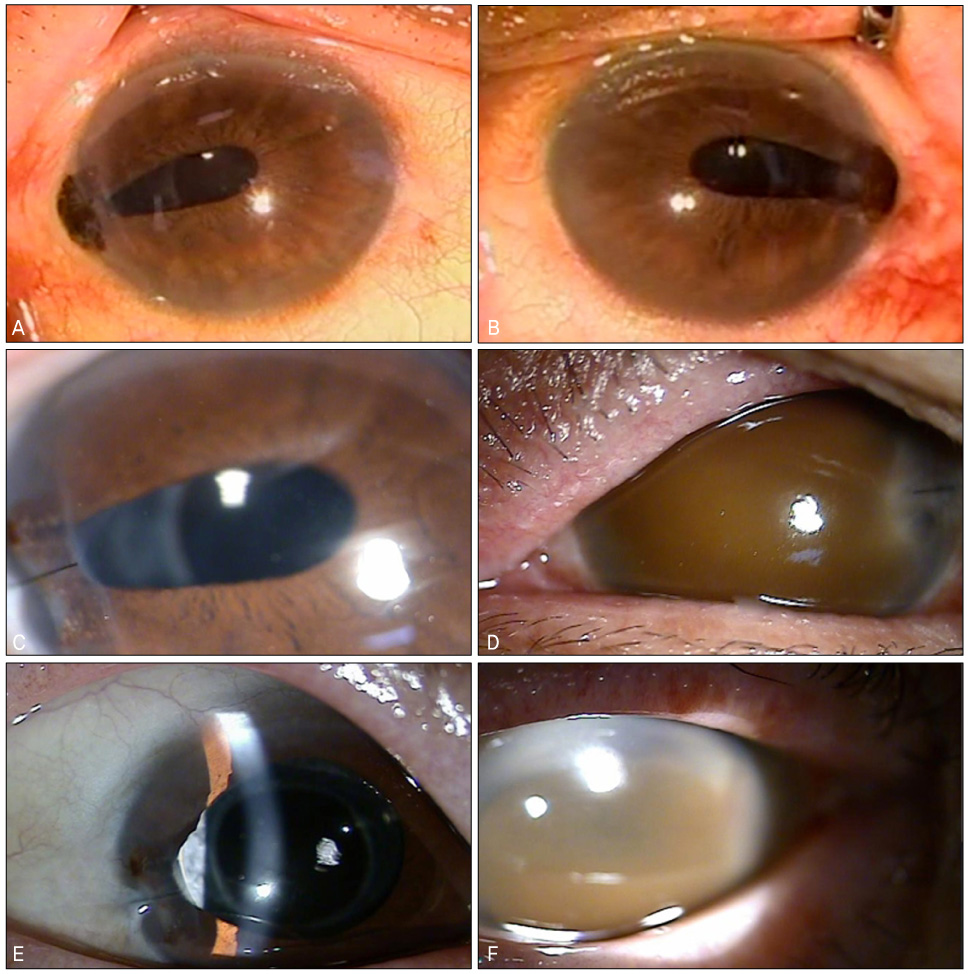
Normal pupil crrr Signs of ruptured globe:
- Hyphema
- Shallow AC
- Soft tension
- Irregular pupil
- Iris or uveal tissue prolapse
- Wound
Differential Diagnosis
Investigations
- Rapid and Full Hx
- Full Ocular Examination VA
- Wash the eye with antibiotic and cover
- X-ray
- CT & US (caution, better post operatively)
Contraindication
- MRI (never ask in ocular trauma - metallic magnetic foreign body very dangerous)
Images
Treatment
- Repair and suturing of the wound
- If prolapsed more 24 hours -Surgical Iridectomy
- If less than 24 hours you can wash and replace iris inside eye
You shouldn’t take iris tissue with suture, should be between cornea no sclera Perpendicular to the w