IM
Etiology
- Rheumatic heart disease: 77-99%
- Infective endocarditis
- Mitral annular calcification
- Autoimmune diseases: SLE, RA
- Mimic mitral stenosis: bacterial endocarditis of the mitral valve with large vegetation / left atrial myxoma
The mitral valve orifice normally has a cross-sectional area of 4 to 6 cm². Symptoms develop when the valve area is 2 to 2.5 cm².
- Congenital Mitral Stenosis
- Atrial Myxoma
- Malignant Carcinoid
- Calcification of the mitral valve annulus
- Congenital
- Some conditions may mimic mitral stenosis: bacterial endocarditis of the mitral valve with large vegetation, left atrial myxoma
- Degenerative aortic stenosis
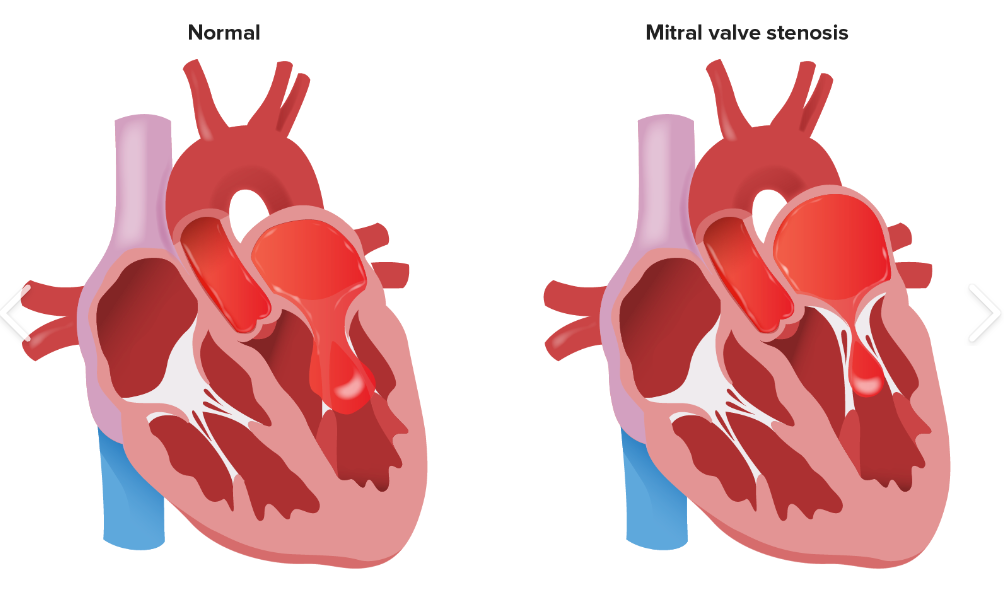
Mitral stenosis refers to narrowing of the mitral valve orifice that occurs as a result of fusion of the leaflet commissures.
Pathophysiology
-
Mitral valve stenosis → obstruction of blood flow into the left ventricle (LV) → limited diastolic filling of the LV (↓ end-diastolic LV volume) → decreased stroke volume → decreased cardiac output (forward heart failure)
-
Mitral valve stenosis → increase in left atrial pressure → backup of blood into lungs → increased pulmonary capillary pressure → cardiogenic pulmonary edema → pulmonary hypertension → backward heart failure and right ventricular hypertrophy
Clinical features
Key features
-
Dyspnea (pulmonary congestion and interstitial edema)
-
Fatigue (low cardiac output state)
-
Strong association with atrial fibrillation (47%)
-
Hemoptysis
-
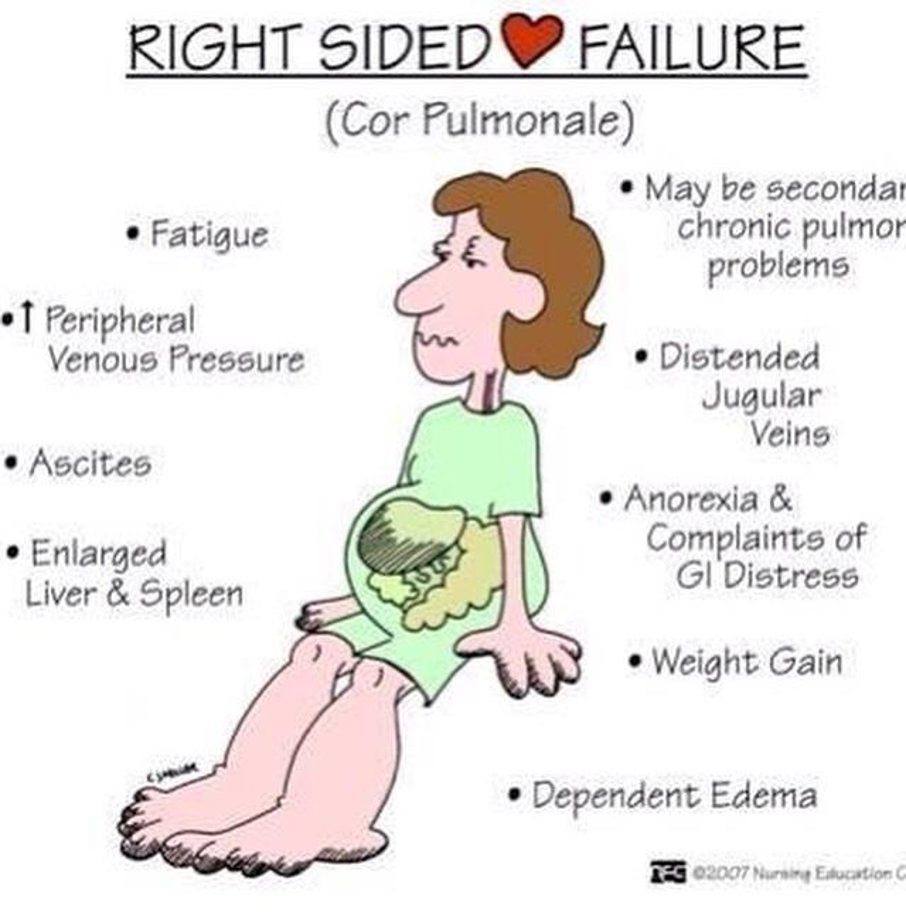
Cor pulmonale: right heart failure due pulmonary hypertension, presenting with abdominal pain (hepatomegaly) and peripheral edema.
-
Dysphagia: Large left atrium pressing on the esophagus
-
Hoarseness: Pressure on recurrent laryngeal nerve
-
Symptoms of embolic disease (e.g., stroke, mesenteric ischemia)
Acute symptoms: tachyarrhythmias or an increased cardiac output secondary to pregnancy, sepsis, or exercise.
Symptoms mimic those of left heart failure
Patients with MS typically progress over many years from being asymptomatic to having symptoms of profound heart failure.
- Dyspnea
- Fatigue
- Hoarseness
- Dysphagia
- Palpitations
- Symptoms of embolic disease (e.g., stroke, mesenteric ischemia)
Later stages
- Symptoms of right heart failure
- Paroxysmal nocturnal dyspnea
- Orthopnea
- Hemoptysis
Physical Exam Findings of MS
-
Prominent “a” wave JVP: Due to pulmonary hypertension and right ventricular hypertrophy
-
Tapping apex beat (palpable S1) is typical.
-
Palpable diastolic thrill in the mitral area best felt in the left lateral position in full expiration.
-
Parasternal heave
-
Signs of Rt heart failure: in advanced disease
-
Mitral facies: Severe MS with ↓ CO, vasoconstriction, resulting in pinkish-purple patches on the cheeks
-
Sequelae of embolic disease (stroke, cool and cyanotic extremity)
-
Atrial fibrillation

Heart Sounds in MS
Diastolic murmur:
-
Low-pitched diastolic rumble most prominent at the apex.
-
Heard best with the patient lying on the left side in held expiration
-
Intensity of the diastolic murmur does not correlate with the severity of the stenosis
-
Loud Opening S1 snap: heard at the apex when leaflets are still mobile
- Due to the abrupt halt in leaflet motion in early diastole, after rapid initial rapid opening, due to fusion at the leaflet tips.
- A shorter S2 to opening snap interval indicates more severe disease.
-
Diastolic murmur heard best at the 5th left intercostal space at the midclavicular line (the apex)
-
Loud first heart sound (S1)
-
Opening snap
-
A high frequency, early to middiastolic sound, heard after S2
-
Occurs when mitral leaflet motion suddenly stops during diastole because the stenosed valve has reached its maximum opening
-
A shorter interval between S2 and opening snap indicates more severe disease; occurs because left atrial pressure is greater than left ventricular end-diastolic pressure (LVEDP).
Signs of heart failure

Diagnosis
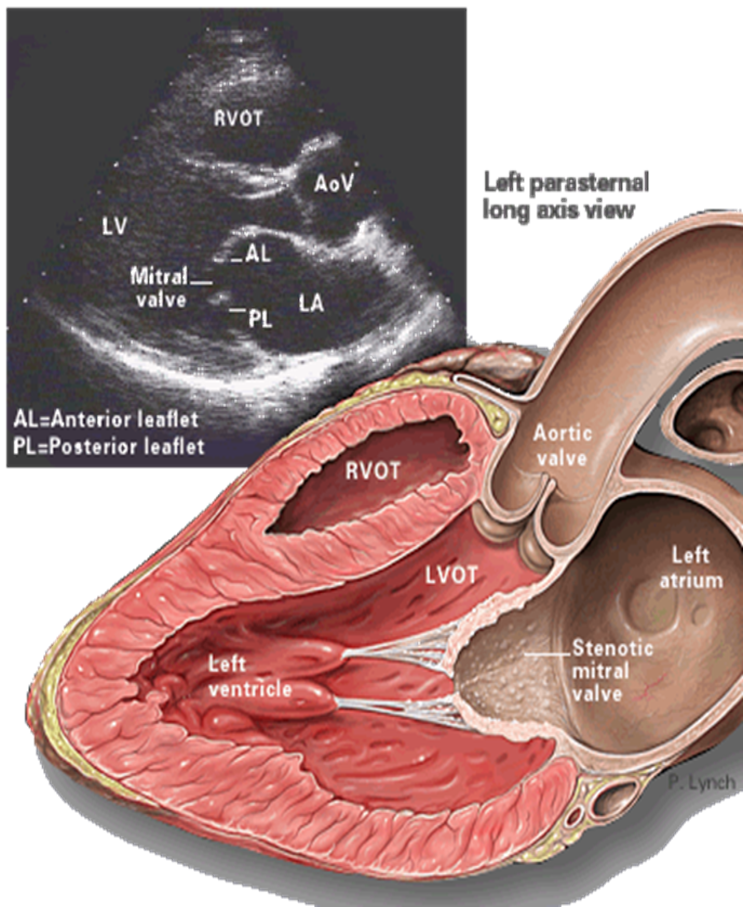
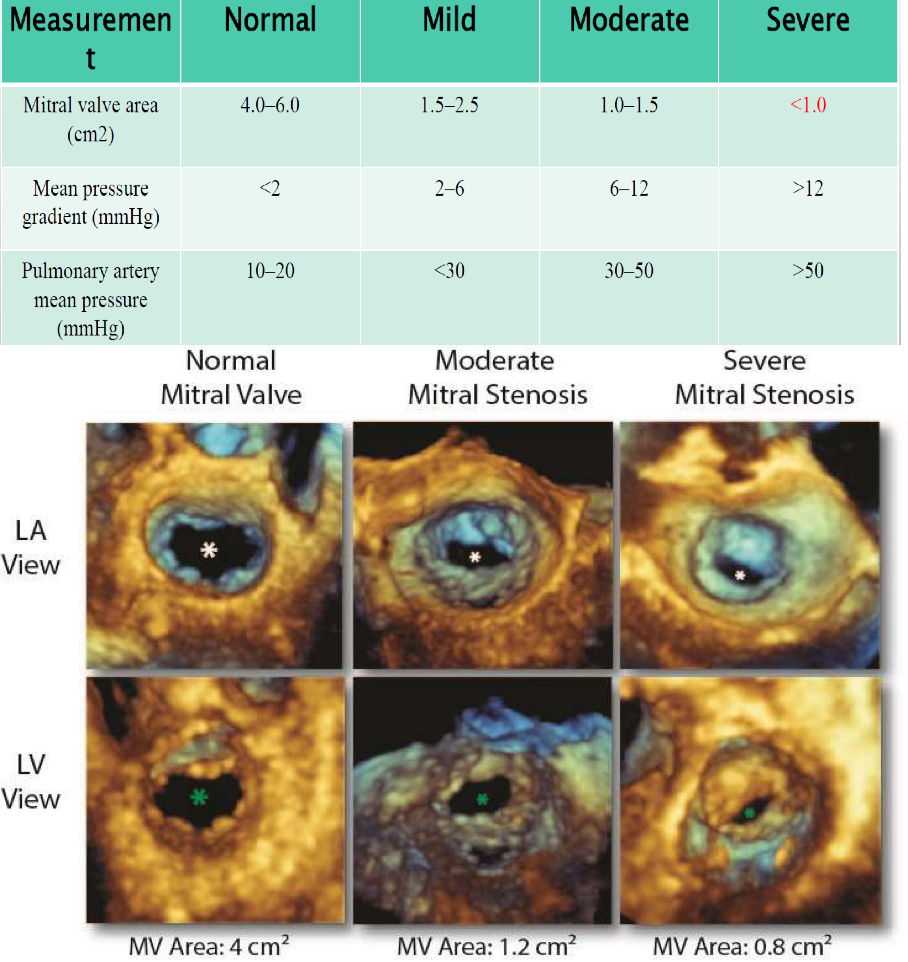
- TTE (Transthoracic echocardiography): best initial test to evaluate the mitral valve and quantify the anatomical extent of the stenosis.
Findings-
Reduced mitral valve area (MVA): ≤ 1.5 cm² (severe)
-
Thickened, calcified leaflets with commissural fusion
-
Increased mean diastolic pressure gradient across the mitral valve
-
RV dilation
-
LA enlargement
-
Evidence of pulmonary hypertension
-
Approach
-
All patients with suspected mitral stenosis should undergo transthoracic echocardiography (TTE).
- Discordance between the patient’s symptoms and the echocardiographic classification of the disease should prompt further testing.
-
Chest x-ray and ECG may show characteristic changes depending on the stage and extent of disease.
-
Laboratory studies are typically nonspecific, although they may support a diagnosis of associated heart failure.
Initial evaluation
(TTE) [3][4]
- TTE is the most important test for diagnosing and guiding the treatment of mitral stenosis.
Secondary cardiac changes, including:
- MVA, valve pressure gradient, and presence or absence of symptoms and pulmonary artery hypertension are used to grade the severity of disease
Severity of mitral stenosis
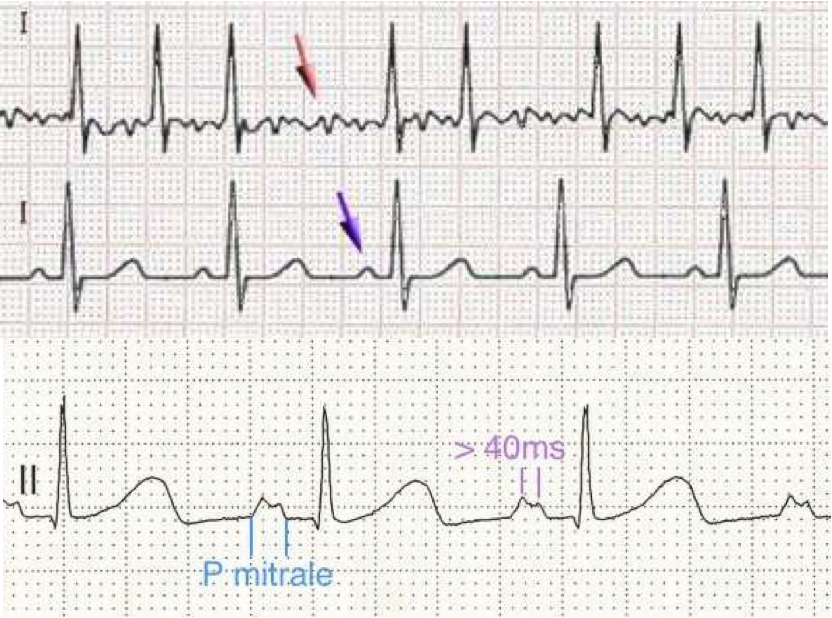
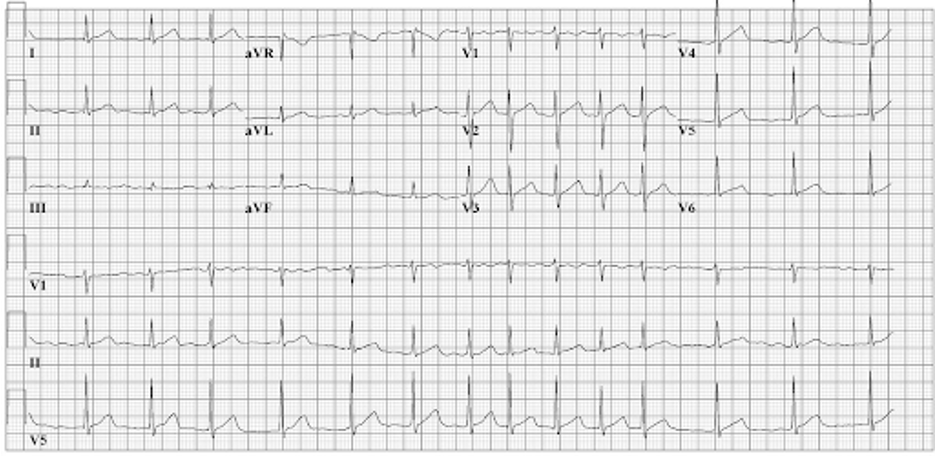
ECG findings in MS
-
BROAD NOTCHED “P” WAVES SIGNIFYING ATRIAL ENLARGEMENT.
-
ATRIAL FIBRILLATION (F- WAVES REPLACING P-WAVES)
-
RIGHT VENTRICULAR ENLARGEMENT
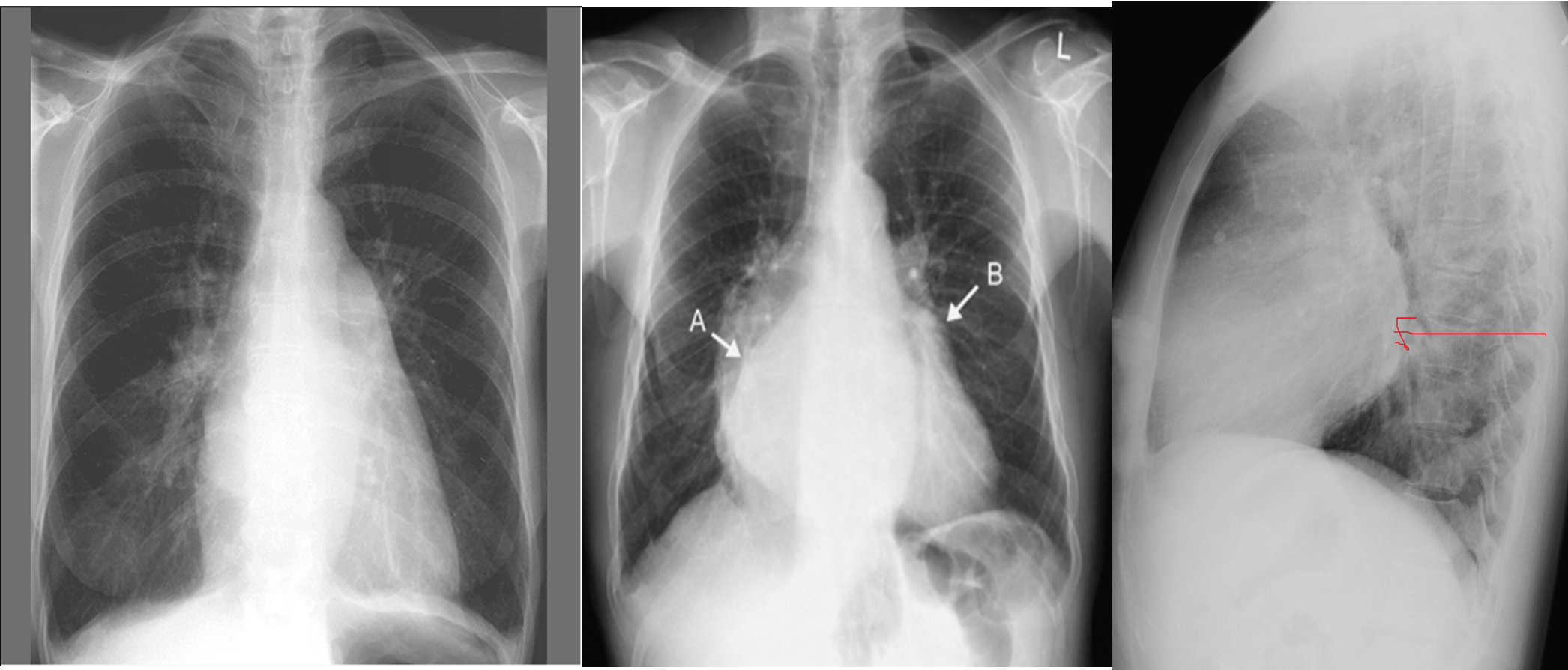
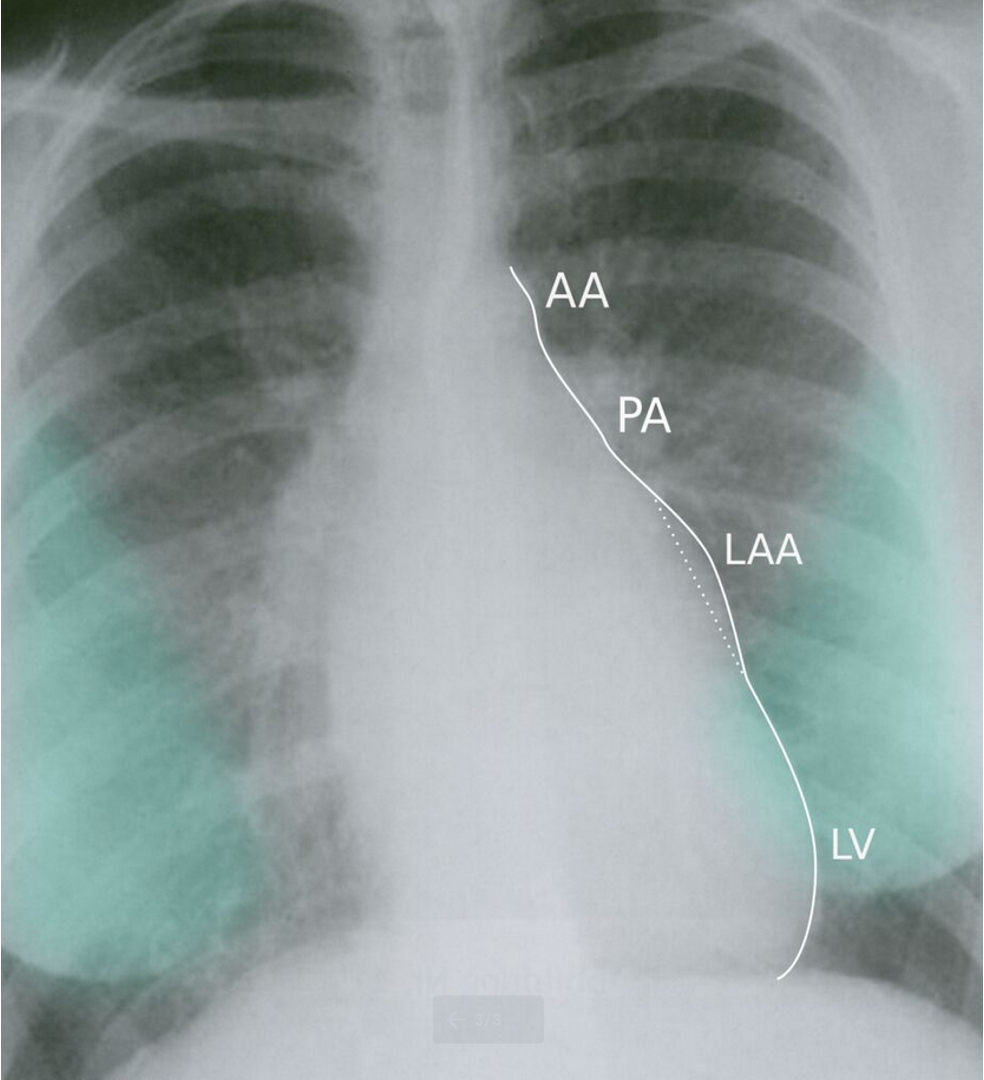
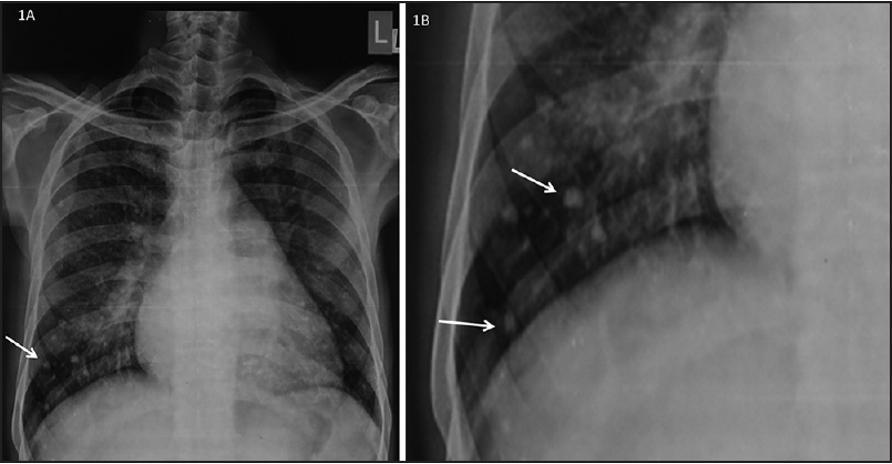
CXR Z
-
Left atrial enlargement
-
Mitralisation of heart: straightening of left heart border
-
Elevation of left mainstem bronchus
-
Evidence of mitral calcification
-
Evidence of pulmonary edema kerley’s b lines
-
Double contour of the right border of heart
Complication of mitral stenosis
-
Left atrial enlargement
-
Atrial fibrillation
-
Systemic embolization (strokes)
-
Pulmonary hypertension
-
Tricuspid regurgitation
-
Right heart failure
-
Hemoptysis
-
Hoarseness of voice
-
Infective endocarditis.
Management of MS
-
Serial echocardiography:
- Asymptomatic
- Mild: 3-5 years (MVA is > 1.5 cm²)
- Moderate: 1-2 years (MVA is 1–1.5 cm²)
- Severe: yearly (MVA is < 1 cm²)
- Asymptomatic
-
Medications: mechanical problem & medical therapy does not prevent progression
-
Screen for and treat all cardiac risk factors.
-
Heart rate control: β-blockers, CCBs, Digoxin which control HR and hence prolong diastole for improved diastolic filling.
-
Acute HF 2nd to onset of AF. Manage AF with rate control.
-
IE prophylaxis: Patients with prosthetic valves or a Hx of IE for dental procedures
-
Recurrent rheumatic fever with cardiac involvement: long-term, daily, antistreptococcal prophylaxis
Indications for interventional management include:
- Symptomatic MS
- MVA decreasing to < 1.5 cm²
- New-onset pulmonary hypertension
Anticoagulation with a vitamin K antagonist (VKA) to a target INR of 2.5 is indicated if any of the following are present: Z
- Atrial fibrillation; warfarin mitral stensosis (other causes thyrotoxicosis, CA bronchus, ischemic heart disease)
- History of embolic disease
- Intracardiac thrombus
- Mechanical prosthetic mitral valve
- First 3–6 months after bioprosthetic mitral valve
Cont…
-
Identify patients early who might benefit from percutaneous mitral balloon valvotomy: asymptomatic & low-risk of thrombosis
-
If PMBC is C/I: follow up every 6 month
Percutaneous mitral valve balloon commissurotomy (PMBC)
Surgical interventions: open commissurotomy and mitral valve (mechanical or bioprosthetic) replacement.
Indications
- Unfavorable anatomy for PMBC
- Presence of thrombus in the left atrium
- Mixed valvular disease (e.g., severe MR, tricuspid D)
Approach
The following recommendations are for rheumatic MS. For all other causes of MS, early consultation with cardiology is recommended as treatment can vary significantly.
Initial management
- General cardiac care and serial TTEs until signs or symptoms of disease progression occur
- In case of acute heart failure: immediate medical stabilizations and treatment of the precipitating cause
- Indications for interventional management include:
- Symptomatic MS
- MVA decreasing to < 1.5 cm²
- New-onset pulmonary hypertension
Conservative management
Many patients with mild to moderate disease can be managed conservatively for years. Patients should remain under the care of cardiology with regular monitoring of valve function.
Serial TTE examinations [1]
Serial TTEs are performed to monitor the progression of MS and guide the timing of interventions.
- Patients typically do not develop symptoms until they have severe disease.
- Early detection prevents irreversible cardiac changes.
Asymptomatic patients
- Every 3–5 years if MVA is > 1.5 cm²
- Every 1–2 years if MVA is 1–1.5 cm²
- Annually if MVA is < 1 cm² TTE should be repeated earlier if symptoms develop or change.
Optimizing medical therapy [1]
Patients should receive guideline-directed medical therapy (GDMT) for any concurrent heart failure.
- Screen for and treat all cardiac risk factors, e.g., diabetes, hyperlipidemia, and hypertension.
Anticoagulation
- Anticoagulation with a vitamin K antagonist (VKA) to a target INR of 2.5 is indicated if any of the following are present:
- Atrial fibrillation
- History of embolic disease
- Intracardiac thrombus
- Mechanical prosthetic mitral valve
- First 3–6 months after bioprosthetic mitral valve implantation
- It is controversial whether anticoagulation is indicated for patients with MS who do not have one of the above features.
- For dosages, see “Anticoagulation in atrial fibrillation”.
Additional measures
- Consider heart rate control (e.g., beta blockers) in younger patients in sinus rhythm with high resting or exercise-induced heart rates. Decreasing the heart rate in patients with symptoms of mild to moderate CHF may improve cardiac symptoms. Consider one of the following agents: [14] Beta blockers, e.g., metoprolol DOSAGE
- Ivabradine DOSAGE Treat atrial fibrillation with rate control.
- Decreased heart rate may also limit cardiac output and cause hypotension; monitor patients carefully.
Acute stabilization
- Abrupt onset of acute heart failure symptoms in patients with MS is usually secondary to tachycardia or increased cardiac output.
- Urgent cardiology consultation is recommended.
- Identify and treat the underlying cause, e.g., sepsis or atrial fibrillation.
- Heart failure symptoms are managed using standard therapy, e.g., diuretics.
- Nitrates may reduce pulmonary congestion but should be used with caution (see “Management of acute heart failure” for further information and dosages). [13]
Patients with mitral stenosis often develop acute heart failure following the onset of atrial fibrillation. Rapid and progressive treatment of atrial fibrillation is necessary in patients with severe mitral stenosis.
echocardiographic criteria: leaflet mobility, leaflet thickening, subvalvular thickening, and calcification.
Treatment is chosen based on the presence of symptoms. In asymptomatic individuals with a low risk of thrombosis, percutaneous mitral valvuloplasty is done.
If there are contraindications for percutaneous mitral valvuloplasty, the individual will be followed up for at least 6 months.
In symptomatic cases of mitral stenosis, percutaneous mitral valvuloplasty is performed, and if there are contraindications, then open surgery is recommended
Percutaneous mitral valve balloon commissurotomy (PMBC) [15]
- PMBC is the preferred intervention in most patients with severe MS.
- A balloon catheter is advanced percutaneously through the mitral valve and inflated to break open commissural stenosis and increase the mitral valve area. The Wilkins score is used to determine eligibility.
Surgery
- Surgical interventions include open commissurotomy and mitral valve (mechanical or bioprosthetic) replacement.
Indications- Unfavorable anatomy for PMBC
- Presence of thrombus in the left atrium
- Mixed valvular disease (e.g., severe MR, tricuspid disease)
- Contraindicated if there is a prohibitively high surgical risk
Case 1
A 55-year-old man presented with sudden onset palpitations and lightheadedness. His symptoms began one hour ago while working in his garden. Temperature is 37.0°C, pulse is 110/min irregularly irregular, respirations are 20/min, and blood pressure is 135/85 mmHg. On physical examination, a rumbling mid-diastolic murmur is heard over the cardiac apex when the patient lies in the left lateral decubitus position. Further history will most likely reveal which of the following?
- Recurrent juvenile arthropathy
- Low T4 level
- Family history of sudden cardiac death
- Myxomatous valve degeneration
- Hypercoagulable state
Case 2
A 50-year-old woman presented with new-onset shortness of breath and fatigue. She reports shortness of breath while lying flat, and she occasionally wakes up at night gasping for air. She also endorses an occasional productive cough with a “brown” tinge. Her medical history includes a “cardiac condition” in her youth that was treated with antibiotics. She immigrated to the United States from India at age 10. Temperature is 37.0°C, pulse is 100/min, respirations are 15/min, and blood pressure is 120/85 mmHg. ECG is obtained and demonstrated below. Cardiac auscultation will most likely demonstrate which of the following findings?
- Systolic murmur over the left paravertebral interscapular area
- Diastolic murmur over the cardiac apex
- Continuous murmur at the left infraclavicular area
- Holosystolic murmur over the left sternal border
- Systolic ejection murmur over the 3rd right intercostal space
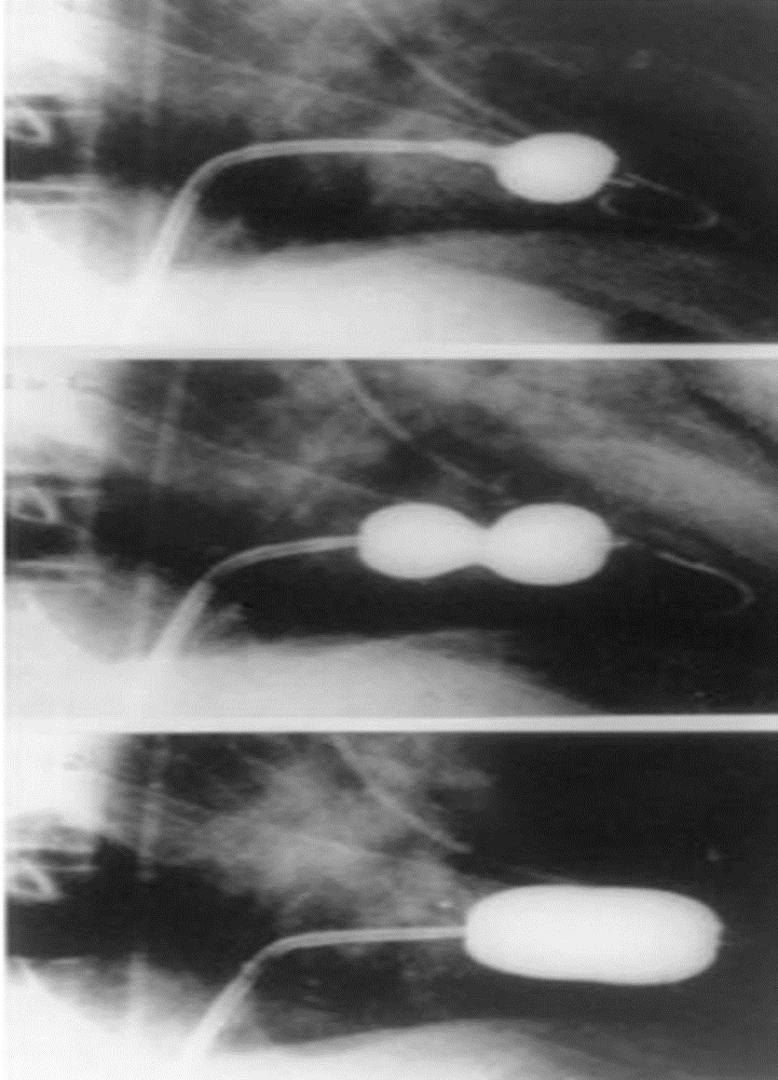
Imaging
PA view: ⇒ Left atrial enlargement:
- Convexity or straightening of the left atrial appendage.
- Left heart border is straight or convex
- Double density of RT cardiac border
- Elevation of the left main bronchus and splaying of the carina
LA view: posterior protrusion of the upper part of posterior heart border.