Brucellosis
Dr. Nada Abdelrahman Brucellosis is a highly contagious bacterial zoonosis, i.e., a disease which spreads from animals to humans. It is a major public health problem in many countries, especially in the Kingdom of Saudi Arabia (KSA).
- Caused by ingestion of unsterilized milk or meat from infected animals or close contact with their secretions (sheep, cattle, goats, pigs).
- Occupational hazard for veterinarians and slaughterhouse workers.
- Examples of other zoonotic diseases: rabies, West Nile virus infection, leptospirosis.
Other Names:
- Malta fever, Maltese fever
- Mediterranean fever
- Rock fever, or undulant fever
Epidemiology
Etiologic Agent: Caused by Gram-negative bacteria called Brucella. Four types can infect humans:
- Brucella Abortus (Cattle)
- Brucella Canis (Dogs)
- Brucella Melitensis (Sheep & Goats - commonest in KSA)
- Brucella Suis (Pigs)
Prevalence is related to the prevalence of domestic animals:
- B. abortus - mainly cattle
- B. melitensis - sheep & goats (most common worldwide)
- B. suis - pigs
- B. canis - dogs
- B. ovis - sheep (not a human pathogen)
- B. neotomae - desert wood rat (not a human pathogen)
Occurrence in KSA: Brucellosis is endemic (very common) in:
- Mediterranean countries (Malta, Greece, Cyprus)
- Arabian Gulf
- Asia
- Latin America
- KSA
Why Brucella is Common in KSA:
- Close contact with camels, sheep, etc. in desert communities.
- Custom of drinking unpasteurized camel milk in deserts & villages.
Organism
- Gram-negative, intracellular coccobacilli bacteria.
- Non-motile, non-capsulated, non-spore forming.
- Brucella spp. are intracellular organisms that survive for long periods within the reticulo-endothelial system.
- Formation of non-caseating granulomas.
- This explains the disease chronicity and tendency to relapse.
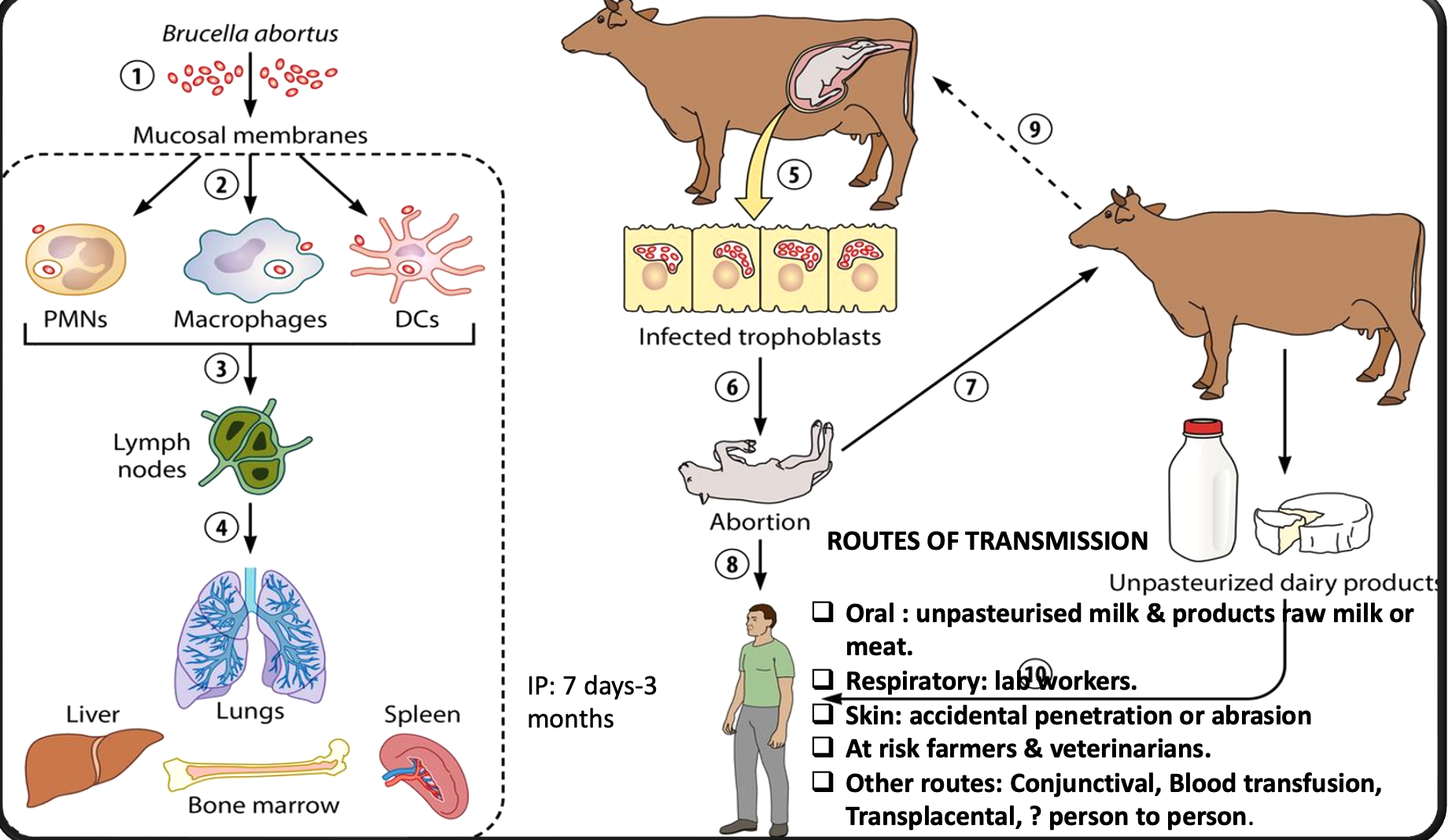
Transmission
Routes of Transmission:
- Oral: Unpasteurized milk & products, raw milk or meat.
- Respiratory: Lab workers.
- Skin: Accidental penetration or abrasion.
- Other: Conjunctival, blood transfusion, transplacental, person-to-person (?).
At-Risk Individuals:
- Farmers
- Veterinarians
Clinical Features
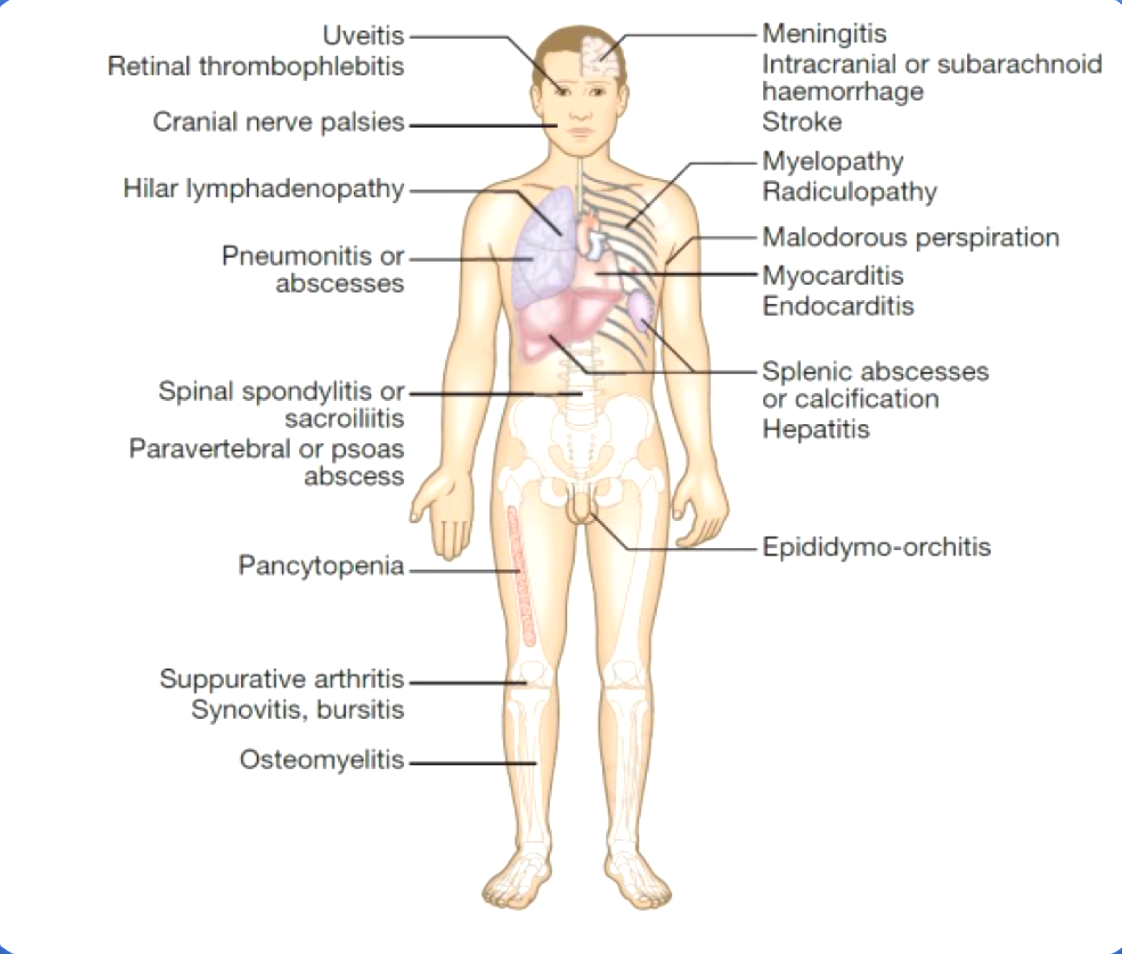
Brucellosis is a systemic disease, and almost any system can be affected. It can present in acute or chronic forms, with symptoms persisting for months or years.
Most Common Symptoms:
- Body & joint pains
- Fatigue
- Fever
- Excess sweating (foul-smelling)
Other Features:
- Chronic ill health
- Hepatomegaly/splenomegaly
- Lymph node enlargement
- Gastrointestinal symptoms (nausea, vomiting, weight loss)
- Sacroiliitis (very characteristic)
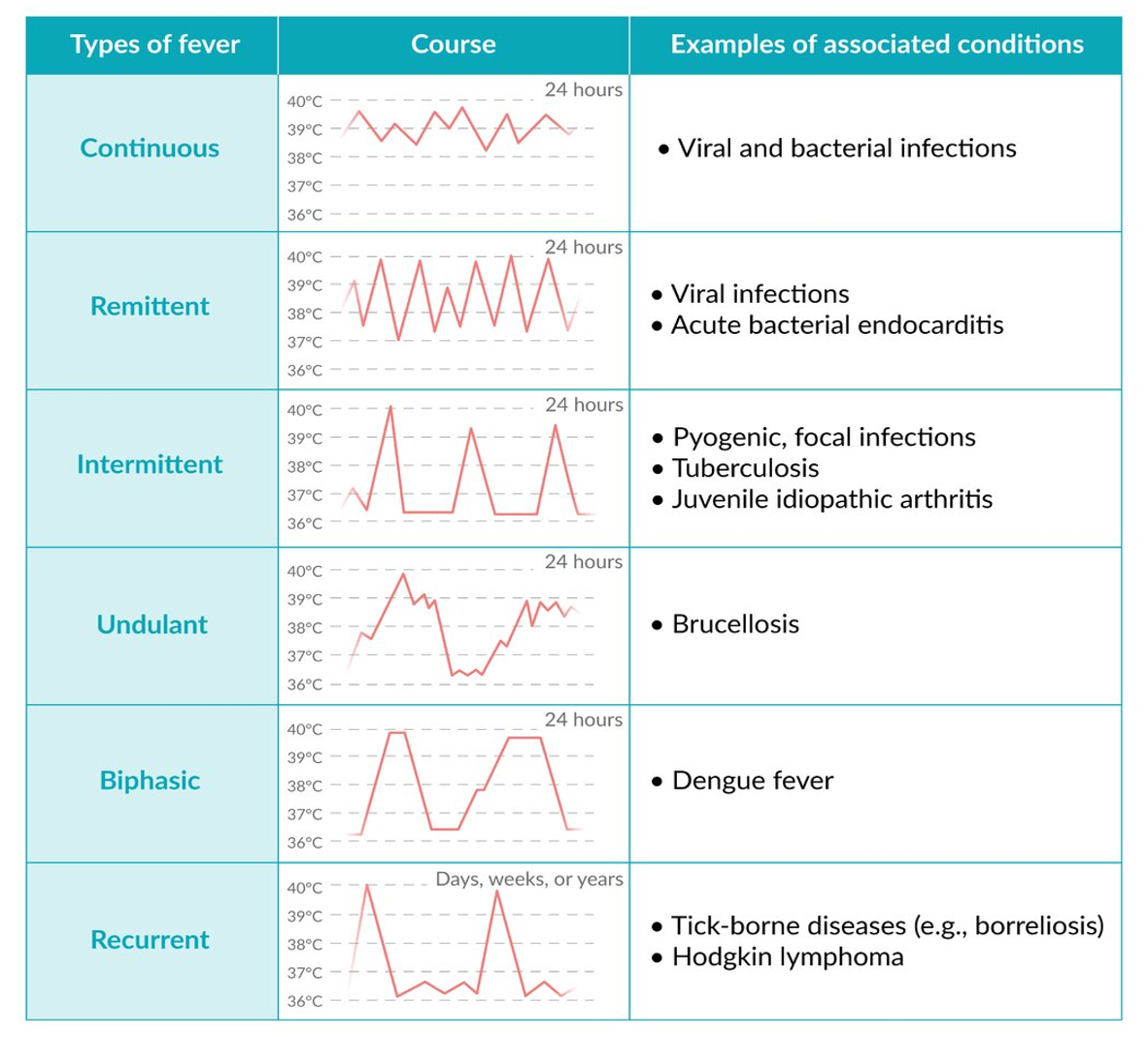
Types of Fever: Acute Brucellosis:
- Incubation period: 1-3 weeks
- Mild, transient illness (B. abortus or canis)
- Toxic illness with multiple complications (B. melitensis)
- 50% have an abrupt onset over days.
Symptoms in brucellosis are nonspecific.
- 90% malaise, chills, sweats, fatigue.
- 50% myalgias, anorexia, and weight loss.
- Sacroilitis ( very characteristic)
- Others: arthralgias, cough, testicular pain, dysuria, ocular pain, or blurring of vision.
- Splenomegaly is present in 10% - 15%
- Painful Lymphadenopathy
Chronic Brucellosis:
- Fever can be intermittent or undulant, persisting for months or years.
Neurologic (Neurobrucellosis):
- Usually presenting as meningitis (1-2%)
- Encephalitis, radiculopathy & peripheral neuropathy, intracerebral abscesses
- Neck rigidity < 50%
- CSF
- Lymphocytic pleocytosis (Same as TB)
- (N) or low sugar
- increase protein
- Culture +ve < 50% - Differentiates TB/Bru
- Agglutination +ve in >95% - Differentiates TB/Bru
Diagnosis
- Clinical features: CBC (Neutropenia, anemia, pancytopenia)
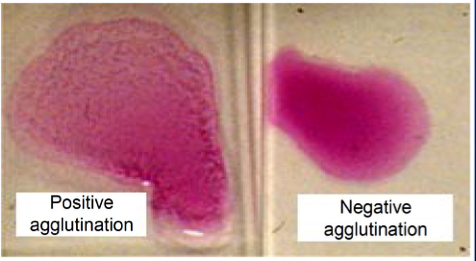
- Serology (Rose Bengal test): Brucella agglutination test
- Blood or tissue culture: Definitive diagnosis but time-consuming (> 2 months). Lymph node or bone marrow biopsy specimen and culture. Histopathology: non-caseating granulomas.
- Polymerase Chain Reaction (PCR)
Serology
Main diagnostic method
- Serum agglutination test - most widely used
- Measures agglutination for IgG, IgM, IgA
- which level is diagnostic ??
- 1 : 160 – non-endemic area
- 1 : 320 - endemic area
- or fourfold rise in titre
Treatment:
Treatment of Choice: Combination therapy has the best efficacy.
Standard Regimen: Oral Doxycycline daily for six weeks in combination with gentamycin injection for 1 week. Best management option
Alternative Regimen: Another option: Oral Doxy. + oral Rifampicin both for 6 wks
Bone disease: - Doxycycline + Rifampicin for 6 weeks + Gentamicin for 7 days, or - Ciprofloxacin + Rifampicin for 3 months.
Neurobrucellosis: Doxycycline + Rifampicin for 6 weeks + Ceftriaxone.
Endocarditis: - Surgical intervention - Doxycycline + Rifampicin + Co-trimoxazole + Gentamicin for 2-4 weeks.
Brucellosis in Pregnancy: Can cause maternal symptoms, abortion, and intrauterine fetal death.
- Treatment of choice:
- Co-trimoxazole (sulfamethoxazole + trimethoprim) + Rifampicin for 4 weeks.
- Weigh risk and benifits
- Caution in the last week of pregnancy due to the risk of kernicterus.
Prevention
- Control of disease in domestic animals (immunization).
- Routine pasteurization of milk.
- Strict biosafety precautions in labs.
- Protective measures in slaughterhouses (wound dressing, protective glasses and clothing, prohibition of raw meat ingestion, use of immune individuals in high-risk areas).
Reference
Kumar & Clark’s Clinical Medicine, page 548.