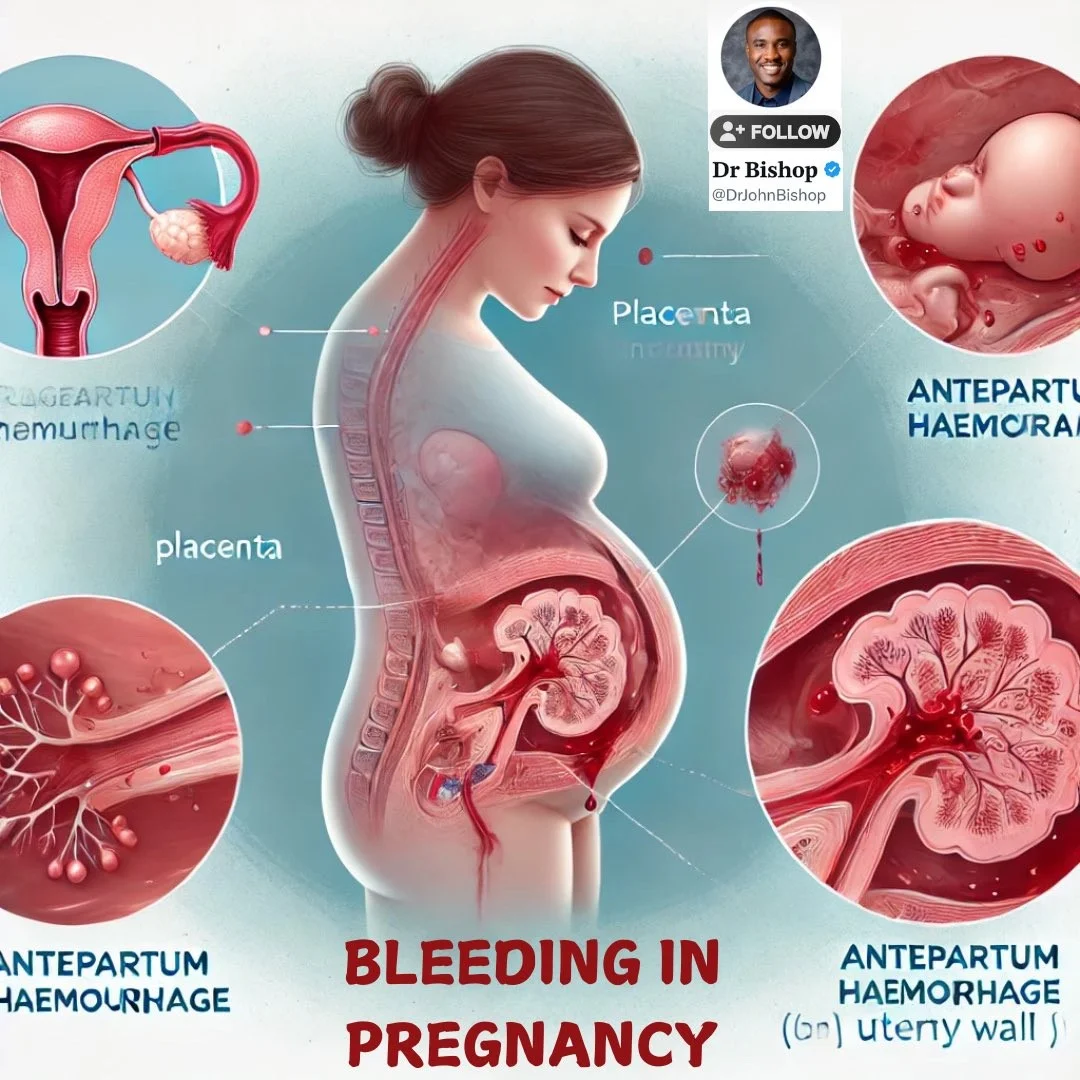
Antepartum Haemorrhage
By Dr. Mona Ahmed

Learning Objectives
At the end of this lecture, the students will be able to:
- Define antepartum hemorrhage.
- Identify the risk factors for placenta previa, abruptio placenta, and placenta accreta.
- Describe the clinical features and diagnostic criteria for placenta previa, placental abruption, and placenta previa accreta.
- Distinguish between placenta previa, abruptio placenta, and other possible causes.
- Describe the appropriate management based on the cause.
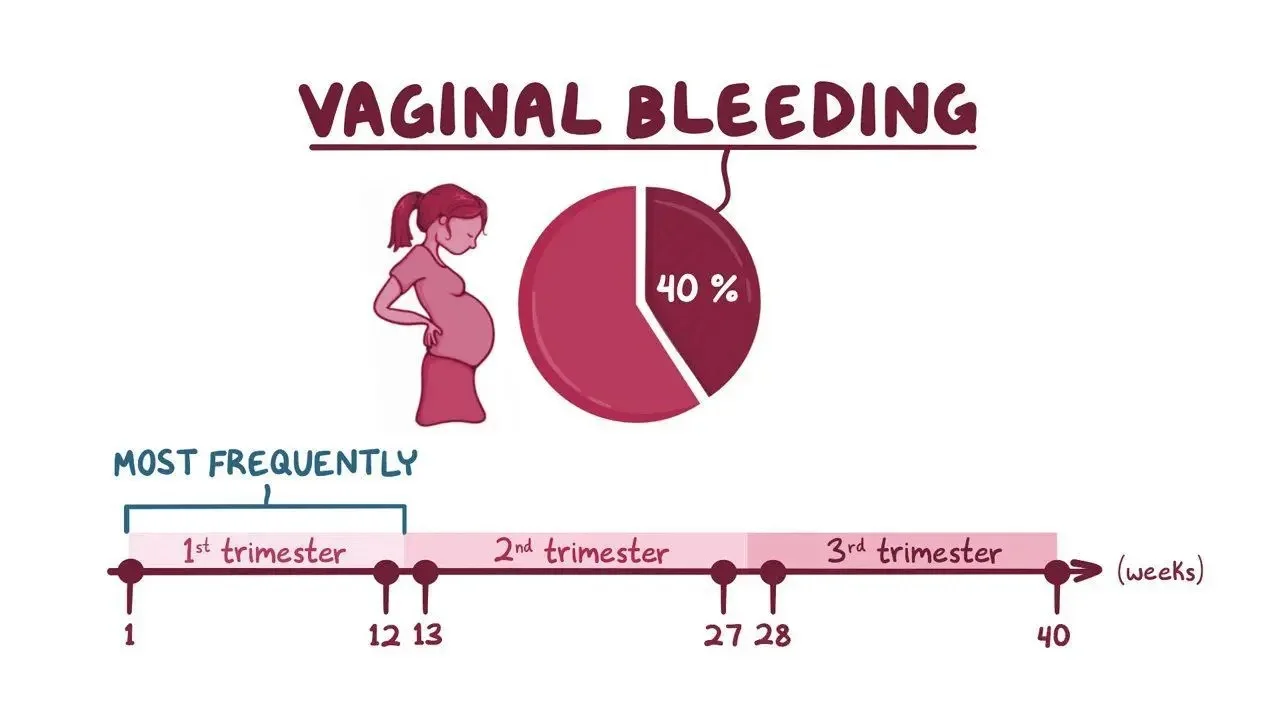
Vaginal Bleeding
APH
Definition:
This is defined as vaginal bleeding after 20 weeks’ gestation.
Incidence:
It complicates 2–5% of pregnancies.
Causes
The causes can be classified into:
- Placental
- Fetal
- Maternal
Placental Causes
Fetal Cause
Maternal Causes
- Vaginal Trauma
- Cervical Ectropion
- Cervical Carcinoma
- Vaginal Infection
- Cervicitis

Key Questions
The key questions are:
- Whether the bleeding is placental or not?
- Is it compromising the mother and/or fetus?
- Or whether it has a less significant cause.
History
- Triggering factors (e.g., trauma).
- Associated with pain or contractions?
- Timing & Amount of Bleeding
- Fresh or old associated with mucus?
- Site of placenta on anomaly scan
- Is the baby moving?
- Last cervical smear (date/normal/abnormal)?
Examination
- Signs of Shock (Pulse, Blood Pressure, Pallor)
- Abdominal Examination:
- Fundal Level
- Is the Uterus Soft or Tender and Firm?
- Fetal Heart Auscultation/CTG
- Speculum Vaginal Examination
- .PV: Should be Avoided if PP Suspected
Investigations
- Full Blood Count
- Clotting Factors
- Kleihauer Test
- Cross-Match (Save 6 Units of Blood)
- Urea & Electrolytes
- Ultrasound (Fetal Size, Presentation, Amniotic Fluid, Placental Position and Morphology)

Initial Management
- Depend on
- ✔️ Cause
- ✔️ Maternal & Fetal Conditions
- ✔️ GA
- ✔️ Degree of Bleeding
- Two Large Bore Cannula
- Resuscitation
- Liaison with Hematologist
- Prepare 4-6 Units of Blood


Acute Management Checklist
- ABC
- Hemodynamic Monitoring: Continuous ECG, Pulse Oximetry, Oxygenation: e.g., Supplemental O2
- Immediate Hemodynamic Support: Including Emergency Blood Transfusion for Hemorrhagic Shock
- Focused Gynecologic History: and Pelvic Examination
- Laboratory Studies: CBC, Coagulation Studies, Type and (Screen CC ??)
- Fetal Heart Rate Tracing
- Transvaginal Ultrasound: to Confirm Placental Location
- Rh(D)-Negative Mothers: Kleihauer-Betke Test, Anti-D Immunoglobulin
- Urgent OB/GYN Consult to Determine Further Management
Complications of APH
- Hypovolemic Shock
- Preterm Labour
- DIC
- PPH
- Emergency C-Section
- Hysterectomy
- Complications of Blood Transfusion
- Fetal Death
Key Learning Points
- Placenta Previa is most dangerous for the mother.
- Placental Abruption is more dangerous for the fetus than the mother.
- Vasa Previa is not dangerous for the mother but is nearly always fatal for the baby.
- Management involves resuscitation and stabilization of mother and senior input regarding timing of delivery.