Breast Changes & Lactation
Overview
Dr. Rayan Albarakati
Objectives
- Identify the normal physiologic & anatomic changes of breasts during pregnancy and postpartum.
- Define colostrum.
- Describe the differences between colostrum and human breast milk.
- Describe how to treat common postpartum abnormalities of the breast.
- Identify the advantages of breast-feeding.
- Describe common challenges in the initiation and maintenance of lactation.
Physiologic & Anatomic Changes of Breast
- The breasts gland, tissue, and nipples increase in size, areola color darkens, and some veins under the skin might become visible.
- Estrogen, progesterone, human chorionic gonadotropin, cortisol, insulin, prolactin, and placental lactogen all play an important role in preparing the breasts for lactation.
Anatomical Changes
Breast
- Hypertrophy (asymmetrical)
- Stretch marks
- Sore or tender
- Visible veins
- Lumps & bumps
- Points downwards
Nipples
- Darkens
- Widens
- Montgomery tubercles hypertrophy
- Pronounced & elongated
- Leaks
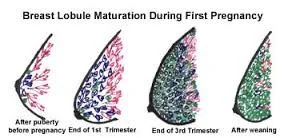
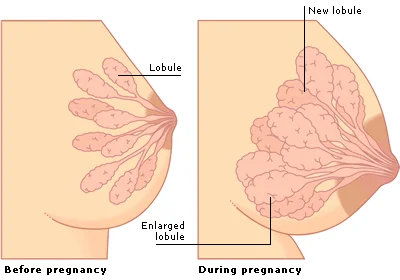
Breast Lobule Maturation During First Pregnancy
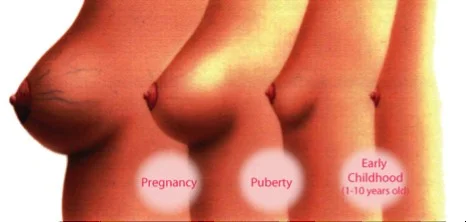
Breast Changes Across Different Life Stages
- Early Childhood (1-10 years old)
- Puberty
- Early Pregnancy
Comparison of Breast Lobules
- Before Pregnancy
- Lobule
- Enlarged lobule
- During Pregnancy
- New lobule
Stages of Breast Lobule Maturation
- After puberty before pregnancy
- End of 1st Trimester
- End of 3rd Trimester
- After weaning
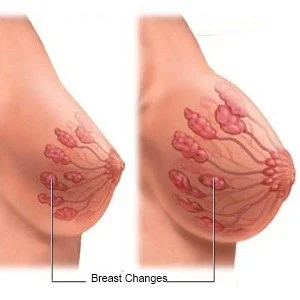
Physiologic Changes
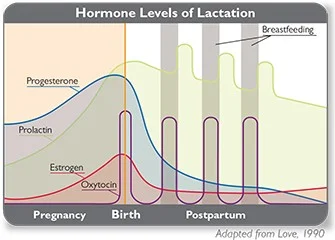
Estrogen and progesterone prepare breasts to make milk. *Released by the placenta during pregnancy.
They have two major roles:
- They increase the size and number of milk ducts.
- They suppress the body from making large amounts of breast milk until after the baby is born.
Once the baby is born and the placenta is delivered, these hormones decrease. This decrease signals the body that it is time to make milk.
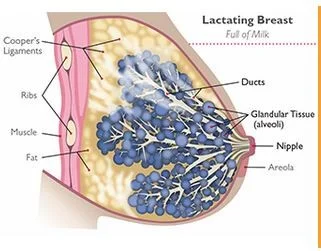
Lactating Breast
Full of Milk
- Cooper’s Ligaments
- Ribs
- Muscle
- Fat
- Ducts
- Glandular Tissue (alveoli)
- Nipple
- Areola
Role of Prolactin
- Prolactin helps breasts make milk.
- After the birth, prolactin levels increase.
- With suckling prolactin is released.
- With each release, the body produces and stores more milk in the breast alveoli.
- If the level of this hormone gets too low, milk supply will decrease.
This is why it is important to breastfeed or pump right after delivery and then at regular time frames.
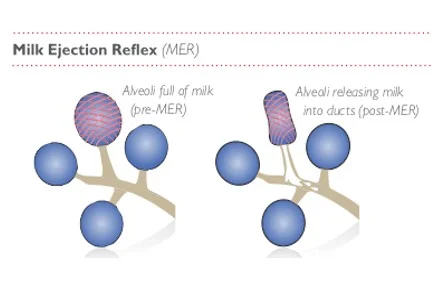
Oxytocin
- Releases milk from breasts.
- Suckling releases this hormone. This release causes milk to be squeezed out of the alveoli, into the ducts, and out.
- This process is called Milk Ejection Reflex (MER).
Milk Ejection Reflex (MER)
- Alveoli full of milk (pre-MER)
- Alveoli releasing milk into ducts (post-MER)
Initiating Lactation
At delivery, two events are essential in initiating lactation:
- A drop in placental hormones, particularly estrogen.
- Suckling stimulates the release of prolactin and oxytocin.
- Oxytocin causes contraction of the myoepithelial cells in the alveoli and milk ducts (ejection).
- Prolactin promotes the production of milk in breast alveoli.
Hormone Levels of LactationZ
Colostrum Definition
A form of milk which is the first secretion from the mammary glands after giving birth, rich in antibodies, and yellowish in color.

Colostrum & Breast Milk
- Colostrum is secreted 2nd day after delivery for 3-6 days.
- It is the colostrum that contains secretory IgA.
- The major components of breast milk are proteins, lactose, water, minerals, and fat.
- The major proteins synthesized exclusively in human breast milk are casein, lactalbumin, and ß-lactoglobulin.
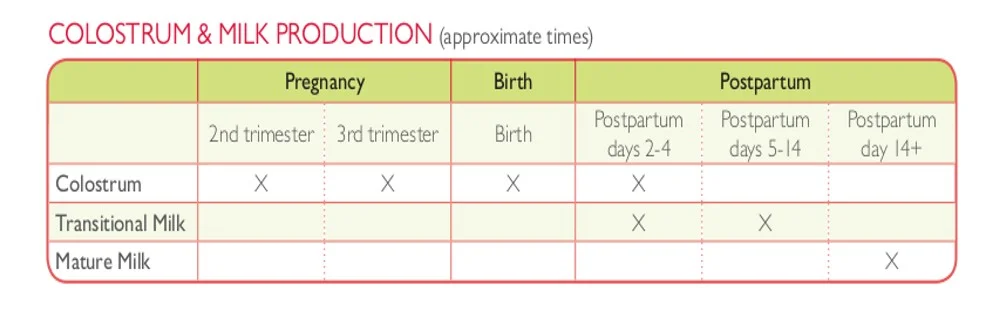
COLOSTRUM & MILK PRODUCTION (approximate times)
| Pregnancy | Birth | Postpartum | ||||
|---|---|---|---|---|---|---|
| 2nd trimester | 3rd trimester | Birth | Postpartum days 2-4 | Postpartum days 5-14 | Postpartum day 14+ | |
| Colostrum | X | X | X | X | ||
| Transitional Milk | X | X | ||||
| Mature Milk | X |
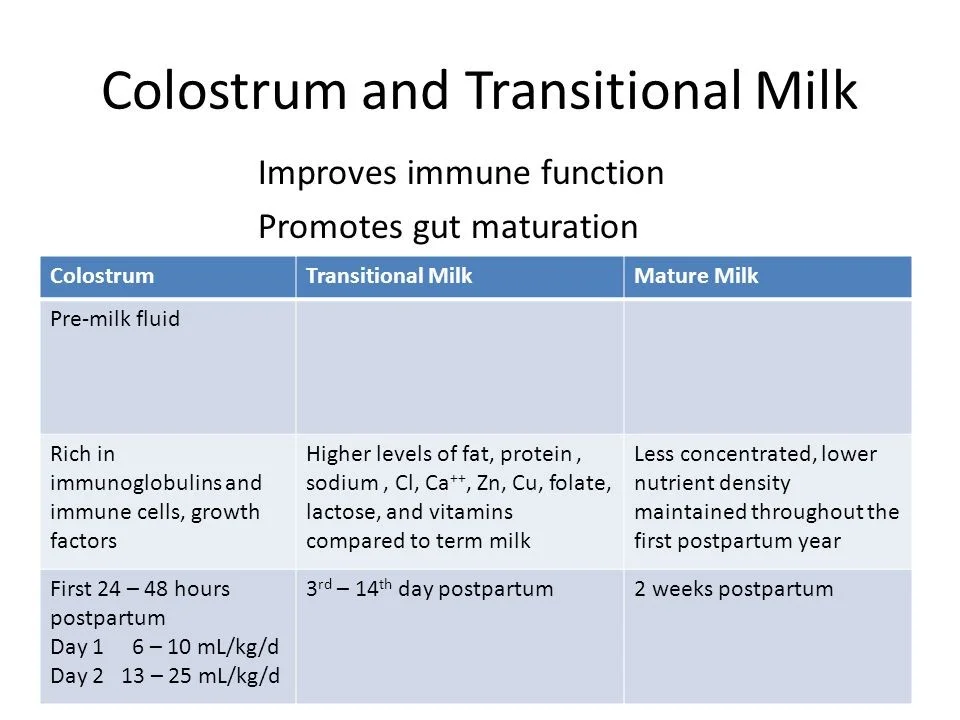
Colostrum and Transitional Milk
- Improves immune function.
- Promotes gut maturation.
| Colostrum | Transitional Milk | Mature Milk |
|---|---|---|
| Pre-milk fluid | ||
| Rich in immunoglobulins and immune cells, growth factors | Higher levels of fat, protein, sodium, Cl, Ca++, Zn, Cu, folate, lactose, and vitamins compared to term milk | Less concentrated, lower nutrient density maintained throughout the first postpartum year |
| First 24 – 48 hours postpartum Day 1 6 – 10 mL/kg/d Day 2 13 – 25 mL/kg/d | 3rd – 14th day postpartum | 2 weeks postpartum |
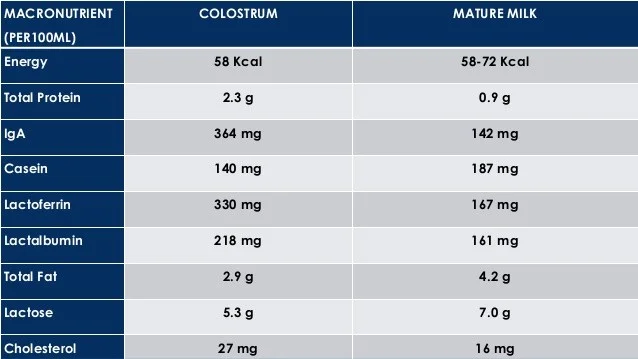
Comparison of Breast Milk ContentsZ
| MACRONUTRIENT (PER100ML) | COLOSTRUM | MATURE MILK |
|---|---|---|
| Energy | 58 Kcal | 58-72 Kcal |
| Total Protein | 2.3 g | 0.9 g |
| IgA | 364 mg | 142 mg |
| Casein | 140 mg | 187 mg |
| Lactoferrin | 330 mg | 167 mg |
| Lactalbumin | 218 mg | 161 mg |
| Total Fat | 2.9 g | 4.2 g |
| Lactose | 5.3 g | 7.0 g |
| Cholesterol | 27 mg | 16 mg |
Advantages of Breastfeeding
- There are many advantages to breastfeeding:
- Breast milk is the ideal food for the newborn, is inexpensive, and is usually in good supply.
- It provides the newborn with passive immunity (secretory immunoglobulin A and maternal lymphocytes).
- It accelerates the involution of the uterus because suckling stimulates the release of oxytocin.
- Emotional Bonding between the mom and the newborn.
Challenges of Initiation and Maintaining Breastfeeding
- No Milk is coming.
- Baby in NICU.
- Mother uses certain medications.
- Mother is working and not with the baby all the time.
- Breast pain.
- Cosmetic reasons.
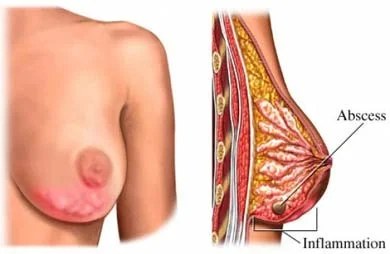
Common Postpartum Breast Complications & Management
- Engorgement & Pain (most common)
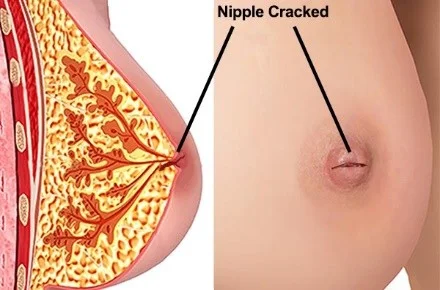
- Cracked nipples
- Mastitis
- Galactocele or Plugged ducts
- Breast abscess (0.5%)

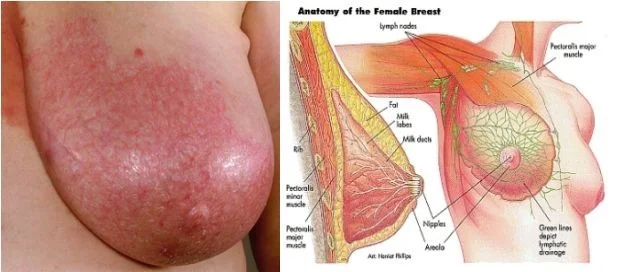
Cracked Nipple
Nipple Cracked

Anatomy of the Female Breast
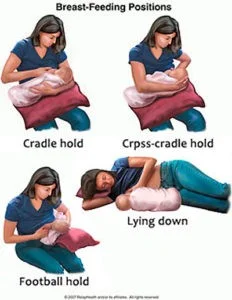
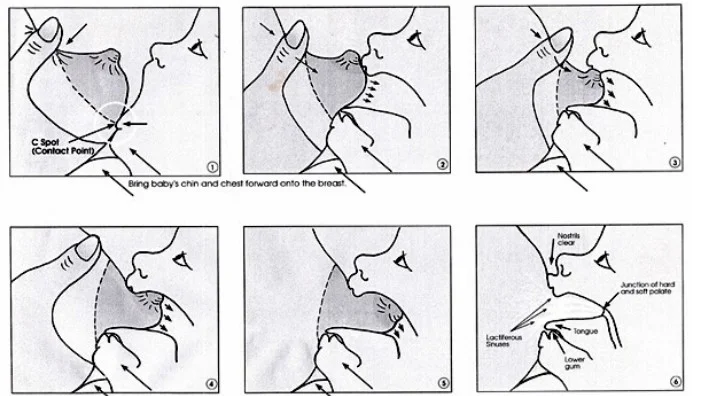
The Right Technique for BreastfeedingOSPE
Directory for Societies and Agencies Supporting Breastfeeding
