GYN
ECTOPIC PREGNANCY
DR Mona Ahmed

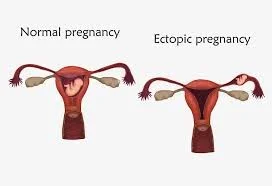
Ectopic pregnancy
Definition and Sites
Ectopic pregnancy is implantation of a pregnancy outside the normal uterine cavity.
Sites:
- Over 98% implant in the Fallopian tube.
- Rarely:
- ✓ in the interstitium of the tube.
- ✓ Ovary.
- ✓ Cervix.
- ✓ abdominal cavity.
- ✓ or in caesarean section scars.

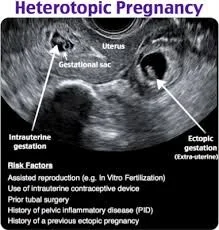
Heterotopic Pregnancy is the simultaneous development of two pregnancies: one within and one outside the uterine cavity.
Incidence : One in 80 pregnancies are ectopic.
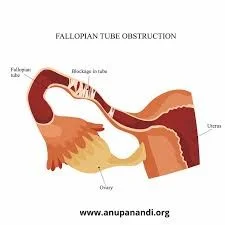
Aetiological factors for ectopic pregnancy:
- Damage of Fallopian tube due to :
- pelvic infection (e.g. Chlamydia/Gonorrhoea) previous ectopic pregnancy.
- Functional alterations in Fallopian tube due to smoking and increased maternal age.
Additional risk factors include :
- previous abdominal surgery (e.g. appendicectomy, caesarean section).
- Subfertility.
- IVF.
- Intrauterine contraceptive devices.
- Endometriosis
- Conception on oral contraceptive/morning after pill.
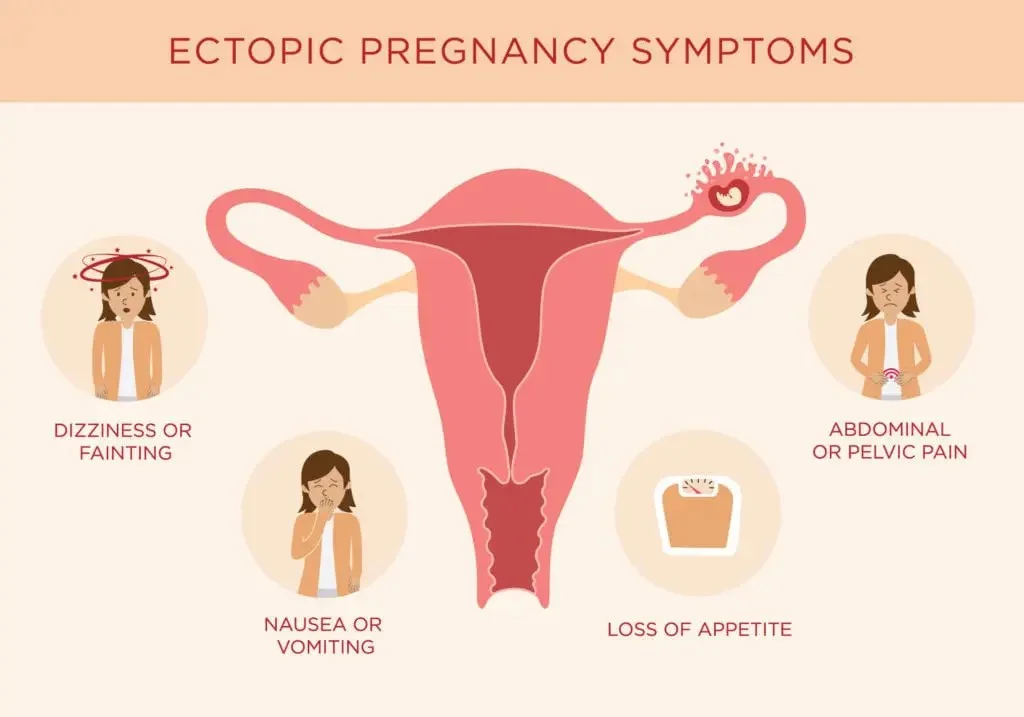
ECTOPIC PREGNANCY SYMPTOMS
- Symptoms of pregnancy.
- Abdominal pain.
- and/or vaginal bleeding in early pregnancy. very acutely with rupture of the EP and massive intraperitoneal bleeding.
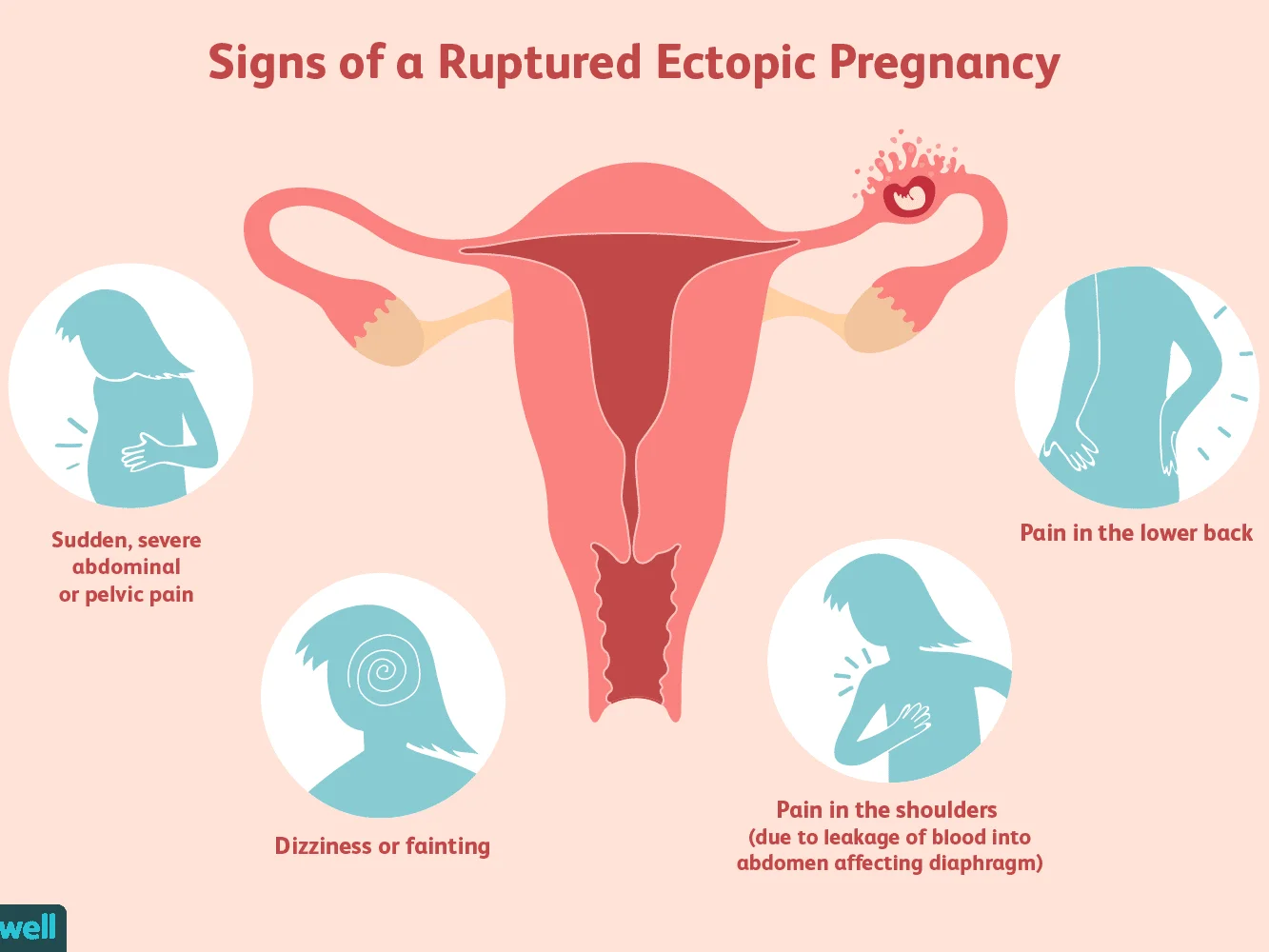
- The free blood in the peritoneal cavity can cause diaphragmatic irritation and shoulder tip pain.
Symptoms associated with ectopic pregnancy include:
- DIZZINESS OR FAINTING
- ABDOMINAL OR PELVIC PAIN
- NAUSEA OR VOMITING
- LOSS OF APPETITE
Diagnosis of ruptured EP:
- Acute abdomen.
- hypovolaemic shock with positive PT.
- Bleeding.
- Abdominal pain.
Without viable intrauterine pregnancy.(US)
Signs of a Ruptured Ectopic Pregnancy
- Sudden, severe abdominal or pelvic pain
- Pain in the lower back
- Dizziness or fainting
- Pain in the shoulders (due to leakage of blood into abdomen affecting diaphragm)
Investigations
- important to assess clinically : (abdominopelvic examination).
- TVUSS:
- A TVUSS showing :
- Empty uterus.
- Adnexal mass.
- Moderate to significant free fluid during TVUSS is suggestive Of a ruptured EP.
- A TVUSS showing :
Serum hCG: the serum hCG level in EP the rise of hCG is often suboptimal Doubling .ie. less than double every two days of quantitive hcg test
-
Haemoglobin and ‘Group and Save’Z
- (or cross-match if pt is severely compromised)
-
measure to assess degree of intra-abdominal bleeding and rhesus status.





Pregnancy of unknown location
- In up to 40% of women with an EP.
- Diagnosis is not made on first attendance and they are labelled as having a ‘pregnancy of unknown location’ (PUL).
Diagnosis :
- Empty uterus + adnexal mass on TVUSS(+positive pregnancy test)
- The mainstay of investigation is consecutive measurement of serum hCG concentrations.
- Endometrial biopsy (occasionally when hCG levels are static).
All PUL must be investigated to determine the location of the pregnancy.

Management
can be managed using (expectant, medical or a surgical ) …depending on clinical presentation and patient choice.
Expectant management is suitable for patients who are … haemodynamically stable. … and asymptomatic.
The patient requires serial hCG measurements until levels are undetectable
Medical management
Intramuscular methotrexate is a treatment option for patients with
- minimal symptoms.
- adnexal mass <40 mm in diameter.
- serum hCG concentration under 3,000 IU/l. until negative -
Methotrexate is a folic acid antagonist that inhibits trophoblastic cells.
- The dose is calculated based on the patient’s body surface area and is 50 mg/m2
- After methotrexate treatment serum hCG is usually routinely measured on days 4, 7 and 11. every 4 days, if increased, double or triple dose
- then weekly thereafter until undetectable.
Medical treatment should therefore only be offered if facilities are present for regular follow-up visits

Contraindications to medical treatment include:
- chronic liver, renal or haematological disorder.
- active infection.
- immunodeficiency.
- breastfeeding.
side-effects
stomatitis, conjunctivitis, gastrointestinal upset and photosensitive skin reaction, and causing abdominal pain.
It is important to avoid
- conceiving for 3 months after, coz of teratogenicity risk.
- Alcohol
- prolonged exposure to sunlight during treatment
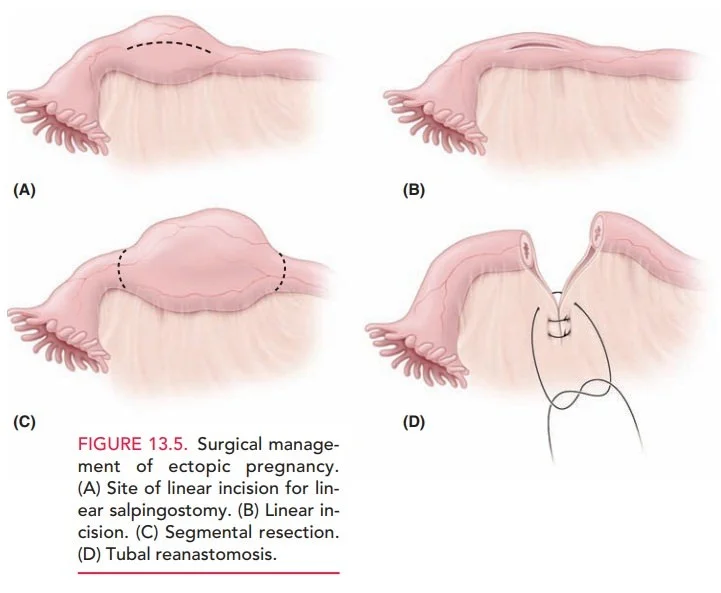
Surgical management
- The standard & definite surgical treatment approach is
- laparoscopy (for stable patient),
- or
- Laparotomy (for severely compromised patients or where there are no endoscopic facilities).
![]()

The operation of choice is:
- salpingectomy (if contralateral tube is healthy)
- or
- salpingostomy.
RR Micrope - novel approaches to operative ectopic pregnancy?
Salpingostomy
- Recommended only if the contralateral tube is absent or damaged.
- It is associated with a higher rate of subsequent EP.
Pregnancy rates subsequently remain high if the contralateral tube is normal
Anti-D administration
-
All rhesus-negative women who have a surgical procedure to manage an EP or miscarriage should be offered anti-D immunoglobulin.
-
Anti-D is not required for:
- Threatened miscarriage.
- Incomplete miscarriage.
- complete miscarriage.
medical management of miscarriage or EP but guidelines differ, and prophylaxis is often given

Summary of other early pregnancy disorders
| Disorder | Definition | Risk factors | Clinical presentation | |
|---|---|---|---|---|
| Gestational trophoblastic disease (GTD) (abnormal trophoblast proliferation) | Spectrum of conditions that includes complete and partial hydatidiform mole, invasive mole and choriocarcinoma | Previous molar pregnancy High or low maternal age Asian origin | Ultrasound features of intrauterine vesicles (‘cluster of grapes’) Persistently raised hCG levels after miscarriage | Registration Uterine evacuation by suction curettage (without misoprostol) Serial hCG measurements Avoid oestrogens |
| Hyperemesis gravidarum | Multiple pregnancies GTD | Excessive nausea and vomiting, often accompanied by dehydration | Antiemetics Fluid and electrolyte replacement Multivitamins Thromboprophylaxis | |
| Ectopic Pregnancy Q&A Discussion |