Medical Disorders in Pregnancy
Sickle Cell Anemia
Definition and Pathophysiology
Sickle cell anemia is an autosomal recessive disorder characterized by abnormal hemoglobin S (HbS). The mutation leads to the destruction of red blood cells.


Prepregnancy Counselling
- Multidisciplinary team involvement (obstetrician and hematologist)
- Partner screening
- Stop iron-chelating agents before pregnancy
- Folic acid supplementation (5mg/day) and penicillin prophylaxis for hyposplenism
- Monitoring of Hb and HbS percentage, with transfusion if necessary
Clinical Features
- Hemolytic anemia
- Painful crises
- Hyposplenism
- Increased risk of infections (UTI, pyelonephritis, pneumonia, puerperal sepsis)
- Avascular necrosis of bone
- Increased risk of thromboembolic disease (pulmonary embolism, stroke)
- ACUTE CHEST SYNDROME (FEVER, CHEST PAIN, TACHYPNEA, INCREASE)
- WCC, pulmonary infiltrates
- iron overload leads to cardiomyopathy
Antenatal Care
- Screening for urine infection at each visit
- Treatment of crisis (analgesia, oxygen, rehydration, antibiotics if infection suspected)
- Regular assessment of fetal growth (ultrasound, Doppler)
- Aim for vaginal delivery with adequate hydration, avoiding hypoxia, and continuous fetal monitoringZ - UNLESS CS is indicated
- Consider antenatal and postnatal thromboprophylaxis
- the use of prophylactic antibiotics
Fetal Complications
- Miscarriage
- IUGR
- Prematurity
- Stillbirth
Thyroid Disease and Pregnancy
Thyrotoxicosis:
- 95% of women have graves disease.
- For first time in pregnancy occur in the late first or early second trimester.Z
Clinical features:
- Palpitation.
- Vomiting.
- Goitre.
- Palmer erythema.
- Emotional liabilities.
- Tremors.
- Lid lag.
- Lid retraction.
Diagnosis:
- TFT


Complications
- Maternal complications: hypertension, preeclampsia, heart failure
- Fetal risks:
- Miscarriage.
- IUGR.
- Preterm birth.
- Fetal hypothyroidism(drug induced).Z
- Thyrotoxicosis (in autoimmune cases due to transplacental TSI)
- IUFD.

Management
- Propylthiouracil is better than carbimazole (less teratogenisity).
- Do serial US to monitor the baby.
- Do TFT in each semester.
- Close monitoring during labour”+ continuous CTG”.
- Do cord blood sampling for TFT.
- Delivery is by VD unless CS is indicated

Asthma in Pregnancy
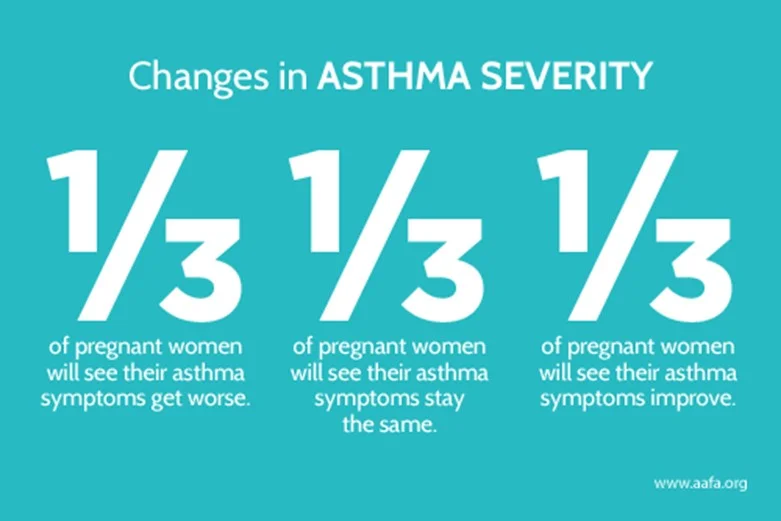
Course of disease
- Approximately one-third of patients worsen during pregnancy, one-third improve, and one-third remain unchanged (pregnancy has no effect).Z
- Most exacerbations occur in the third trimester, but most pregnancies pass uneventfully.
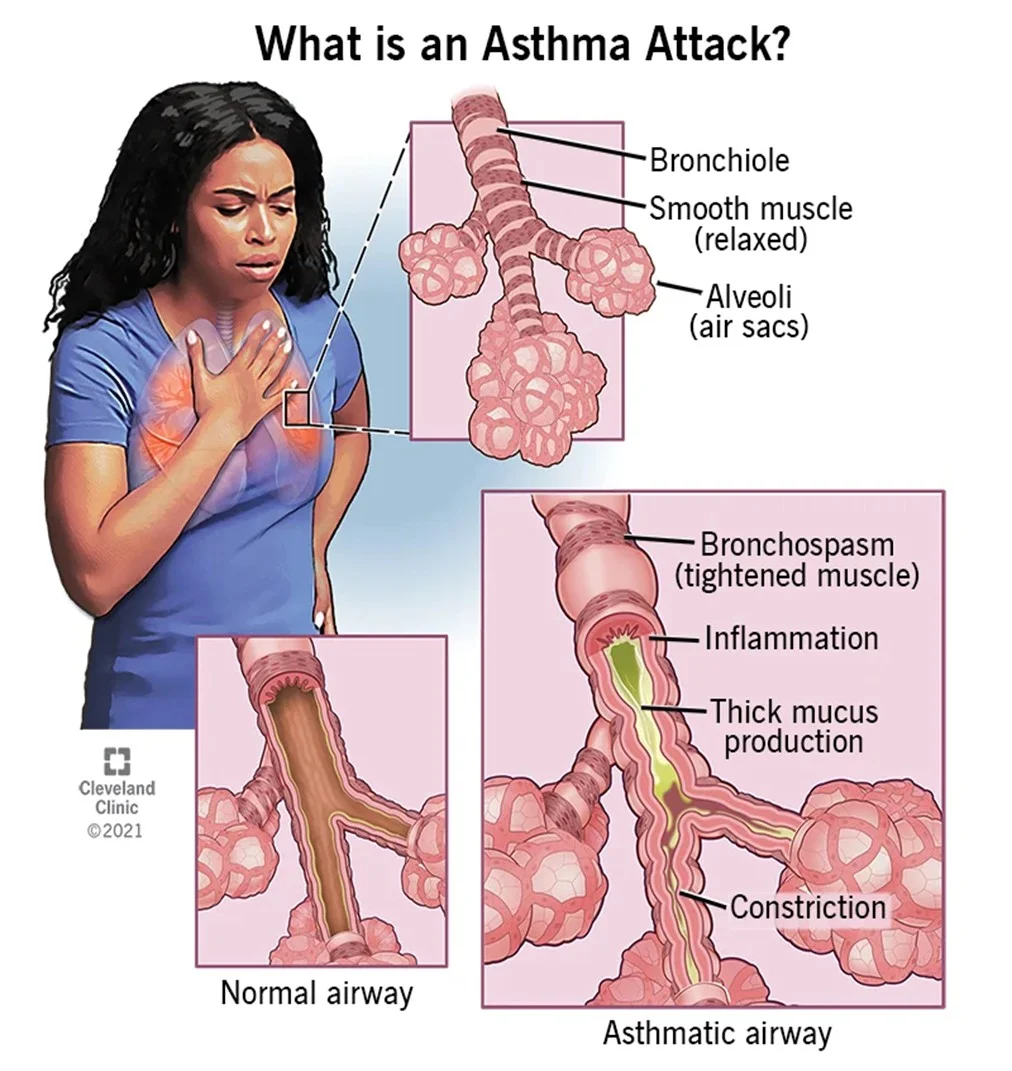
Symptoms
- Cough, wheeze, dyspnoea, chest tightness.
- Avoid known trigger factors.
Common trigger factors
- Pollen, animal dander, dust
- Chest infection, cold weather, emotional stress
Signs of exacerbation
- Tachycardia, increased respiratory rate, audible wheeze, use of accessory respiratory muscles.
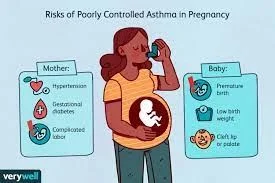
Maternal risks
- Increased risk of preeclampsia, higher maternal mortality, and greater need for hospitalization.
Fetal/neonatal risks
- Low birth weight, preterm delivery, and risk of neonatal asphyxia.
 #Z
#Z

Management
- O2.
- Bronchodilator(Salbutamol).(inhaler or oral ).
- Steroids.(oral , inhaler).
- Antibiotics if there is infection.
- Avoid PGs in induction(exacerbate asthma).
- Delivery
VD Unless C/S is indicated.

Iron Deficiency Anemia
Definition
- Anaemia in pregnancy: haemoglobin or haematocrit below trimester-specific cut-offs
- 1st trimester: Hb < 11 g/dL, Hct < 33%
- 2nd trimester: Hb < 10.5 g/dL, Hct < 32%
- 3rd trimester: Hb < 11 g/dL, Hct < 33%
Classification (by MCV / mechanism)
- By size (MCV):
- Microcytic (< 80 fL): iron deficiency, thalassaemia (commonly)
- Normocytic (80–100 fL): anaemia of chronic disease, acute blood loss
- Macrocytic (> 100 fL): folate or vitamin B12 deficiency
- By mechanism (often overlapping):
- ↓ Production: iron, folate, B12 deficiency, bone marrow disease
- ↑ Destruction: haemolysis (sickle cell, thalassaemia)
- Blood loss: acute or chronic (menstrual, obstetric, GI)
Risk factors
- Poor dietary intake (low iron/protein/folate)
- Short interpregnancy interval, teenage pregnancy, multiparity
- Heavy menses or prior delivery blood loss
- GI malabsorption, chronic illness
- Hemoglobinopathies (suspect with relevant family history or ethnicity)
Diagnosis
- CBC with indices: Hb, Hct, MCV
- Ferritin: < 30 µg/L confirms iron deficiency
- Peripheral blood smear
- Hemoglobin electrophoresis if hemoglobinopathy suspected
Management
- Lifestyle / nutrition:
- Eat iron-rich foods (red meat, poultry, legumes, leafy greens)
- Vitamin C enhances iron absorption; avoid tea/coffee with meals
- Pharmacological:
- Routine supplementation in pregnancy: ~27 mg/day elemental iron (prenatal vitamins)
- Treatment (oral): ferrous sulfate / ferrous fumarate / ferrous gluconate (dosing depends on elemental iron goal)
- Parenteral iron: for severe anaemia, oral intolerance, or poor response
- Transfusion: reserved for severe cases (e.g., Hb < 6 g/dL with maternal or fetal compromise)
- Practical choices and considerations:
- Ferrous sulfate — first-line: effective, widely available, affordable
- Ferrous gluconate — lower elemental iron, better tolerated (less GI upset) but requires more tablets
- Ferrous fumarate — highest elemental iron per tablet → fewer tablets needed, but may cause more GI side effects
Elemental iron content (approximate per tablet)
- Ferrous fumarate (325 mg): ~106 mg elemental iron
- Ferrous sulfate (325 mg): ~65 mg elemental iron
- Ferrous gluconate (300 mg): ~34 mg elemental iron
Treatment approach (summary)
- Start with ferrous sulfate unless not tolerated.
- If intolerance → switch to ferrous gluconate (gentler).
- If higher elemental dose with fewer pills needed and tolerated → consider ferrous fumarate.
- Use parenteral iron or transfusion for severe / refractory cases or urgent maternal/fetal compromise.
Prevention & screening
- Universal low‑dose iron supplementation from 1st trimester (prenatal vitamins with folate)
- Early screening: CBC at booking and again at 24–28 weeks
Maternal and fetal complications (with emphasis on severe anaemia)
- Maternal: fatigue, reduced work capacity, increased infection risk, higher likelihood of transfusion in obstetric haemorrhage
- Severe anaemia (Hb < 6 g/dL) associated with: abnormal fetal oxygenation, non‑reassuring fetal heart patterns, fetal cerebral vasodilatation, fetal death — may prompt maternal transfusion for fetal indications
- Postpartum: increased risk of postpartum depression, poorer maternal–infant interaction and potential negative effects on infant development


Urinary Tract Infections (UTI)Z
-
Asymptomatic bacteriuria: ~4–8% prevalence; if untreated, ~40% may progress to symptomatic infection.
-
Acute cystitis: ~1% (incidence).
-
Acute pyelonephritis: ~1–2% (incidence).
-
Risk factors
- Female sex, especially with diabetes mellitus
- Sickle cell trait or disease
- Immunosuppression
- Urinary tract stones
- Polycystic kidney disease
- Congenital renal anomalies
-
Typical symptoms
- Pyelonephritis: nausea, vomiting, loin (flank) pain, fever
- Cystitis: suprapubic pain, dysuria
-
Investigations
- Positive urine dipstick should always be followed by a midstream urine (MSU) culture.
-
Management
- All bacteriuria should be treated to prevent pyelonephritis and reduce risk of preterm labor — typically with 3–7 days of a broad-spectrum antibiotic.
- Acute cystitis: treat for 7 days with an appropriate antibiotic.
- Pyelonephritis: treat for 10–14 days with an appropriate antibiotic.
Epilepsy in pregnancy — key points
- Common causes of seizures in pregnancy: epilepsy, eclampsia, encephalitis/meningitis, space‑occupying lesions (tumour, tuberculoma), cerebrovascular accident, cerebral malaria or toxoplasmosis, thrombotic thrombocytopenic purpura, drug/alcohol withdrawal, toxic overdose, metabolic abnormalities (e.g. hypoglycaemia).
- Most mothers have healthy babies. Risk of congenital abnormalities depends on the type, number and dose of antiepileptic drugs (AEDs). Sodium valproate should be avoided in pregnancy because it has a high risk of congenital malformations and adverse neurodevelopmental effects in the child.
Definition, diagnosis and seizure types
- Definition: Epilepsy = recurrent unprovoked seizures, normally diagnosed by a neurologist.
- Common seizure types: tonic–clonic, absence, focal.
- Pregnancy differential diagnosis: eclampsia, metabolic causes, cardiac syncope, psychogenic non‑epileptic seizures, and epilepsy.

Cardiovascular diseases pre-pregnancy counselling
- Lifestyle
- Multidisciplinary with cardiologist 5 mg
- IUGR
- Small for gestational age
- Preterm
Labor
- 1 stage (Cervical diltation + pain) - we give pain killer
- 2 stage (Delivery of baby) - Prophylactic Forceps
- 3 stage (Placental delivery) - Avoid angometr…?
Pre‑pregnancy counselling
- Folic acid: 5 mg/day before conception to reduce neural tube defects.
- AED choice: use the lowest effective dose and avoid valproate and polytherapy where possible.
- Counselling topics: risks of congenital malformations and long‑term neurodevelopmental effects (particularly with valproate). Women who have been seizure‑free for ≥1 year have the best prognosis in pregnancy.
Antenatal management
- Joint obstetrics–neurology care is recommended.
- Screening: detailed anomaly scan at 18–20 weeks; consider serial growth scans if on AEDs.
- AED monitoring: routine serum levels usually not required (exceptions such as lamotrigine in selected cases).
- Obstetric risks: increased risk of miscarriage, hypertensive disorders, haemorrhage and preterm birth.
- Maternal mental health: screen for depression, anxiety and cognitive effects.
- Manage pregnant women with significant heart disease in a joint obstetric/cardiac clinic.
- Continuity of care makes the detection of subtle changes in maternal wellbeing more likely.
- Routine physical examination should include:
- pulse rate.
- blood pressure.
- jugular venous pressure.
- heart sounds.
- ankle and sacral oedema
- and presence of basal crepitations.
- Most women will remain well during the antenatal period.
- Echocardiography is useful in assess function and valves,
- and an echocardiogram at the booking visit and at around 28
- weeks’ gestation is usual.
- Any signs of deteriorating cardiac status should be carefully investigated and treated.
- Anticoagulation is essential in patients with:
- congenital heart disease with pulmonary hypertension (PH).
- or artificial valve replacements.
- and in those at risk of atrial fibrillation.
- Low molecular-weight heparin is often used as an alternative to
- warfarin, especially in the first and third trimester.
Intrapartum care
- Seizure risk in labour is low (~1–2%). Continue AEDs (oral or parenteral as needed).
- Seizure treatment: benzodiazepines are first‑line — treat promptly.
- Analgesia: epidural, Entonox and TENS are safe. Avoid pethidine (can be epileptogenic).
- Delivery: epilepsy alone is not an indication for caesarean section unless there is poor seizure control. Continuous fetal monitoring if seizures occur.
Postpartum management
- Seizure risk ↑ in the first 72 hours postpartum (stress, sleep deprivation, missed doses).
- Review AED dose within ~10 days postpartum to avoid toxicity (physiological changes can alter levels).
- Breastfeeding: encouraged — most AED exposure via milk is compatible with breastfeeding. Lamotrigine and levetiracetam transfer more into milk, but definitive adverse outcomes have not been proven.
- Safety advice: take practical precautions (e.g. baby baths on the floor, don’t bathe alone, general seizure‑safety measures).
- Postpartum depression: more common in women with epilepsy (≈29% vs 11%) — screen all.
Contraception & future pregnancy
-
With enzyme‑inducing AEDs, effective options include copper IUD, levonorgestrel IUS and depot injection; enzyme inducers reduce the efficacy of combined pills, patches, rings and implants.
-
Note: lamotrigine levels can be affected by estrogen contraceptives (dose interactions may increase seizure risk).
-
Emergency contraception: copper IUD preferred when on enzyme‑inducing AEDs.
Management of labour and delivery
- In most cases the aim of management is to await the onset of spontaneous labour.
- Anaesthesia is often recommended to reduces the pain related stress.
- Prophylactic antibiotics should be given to any woman with a structural
- heart defect to reduce the risk of bacterial endocarditis.
- VD is the mode of delivery unless C-section is indicated.
- Caesarean delivery is associated with:
- Risk of haemorrhage, thrombosis and infection, conditions that are likely to be much less
- well tolerated in women with cardiac disease
- the maternal condition is considered too unstable to tolerate the physiological
- demands of labour.. Postpartum haemorrhage in
- particular can lead to major cardiovascular instability. Ergometrine may be
- associated with intense vasoconstriction, hypertension and heart failure, and
- therefore active management of the third stage is usually with Syntocinon™
- (synthetic oxytocin) alone. Syntocinon is a vasodilator and therefore should be
- given slowly to patients with significant heart disease, with low-dose infusions
- preferable. High-level maternal surveillance is required until the main
- haemodynamic changes following delivery have passed
Prepregnancy counselling
- Women with heart disease: will be aware of their condition prior pregnancy
- They should be fully assessed by an obstetrician and cardiologist.
- fetal risks carefully explained.
- A plan to optimize medication & health state.
Issues in pre-pregnancy counselling of women with heart disease
- Risk of maternal death.
- Possible reduction of maternal life expectancy.
- Effects of pregnancy on cardiac disease.
- Mortality associated with high-risk conditions.
- Risk of fetus developing congenital heart disease.
- Risk of preterm labour and FGR.
- Need for frequent hospital attendance and possible admission.
- Intensive maternal and fetal monitoring during labour.
- Other options – contraception, adoption, surrogacy.
- Timing of pregnancy
Fetal risk of maternal cardiac disease
- Recurrence (congenital heart disease).
- Maternal cyanosis (fetal hypoxia).
- Iatrogenic prematurity.
- FGR.
- Effects of maternal drugs (teratogenesis, growth restriction, fetal loss).
Risk factors for development of heart failure in pregnancy
- Respiratory or urinary infections.
- Anaemia.
- Obesity.
- Corticosteroids.
- Tocolytics.
- Multiple gestation.
- Hypertension.
- Arrhythmias.
- Pain-related stress.
- Fluid overload
- Management of labour in women with heart disease
- Avoid induction of labour if possible.
- Use prophylactic antibiotics.
- Ensure fluid balance.
- Avoid the supine position.
- Discuss regional/epidural anaesthesia/analgesia with senior anaesthetist.
- Keep the second stage short.
- Use Syntocinon judiciously.