Table of Contents
- Placenta
- Overview of the Placenta
- Development of Placenta
- Formation and Components
- Detailed Development Process
- The Placenta at Term
- Placental Circulation
- Types of Circulation
- Types of Placenta
- Umbilical Cord
- Fetal Membrane
- Function of Placenta
- Amniotic Fluid
- Function of Amniotic Fluid
- During Pregnancy
- During Labor
- Abnormality of Amniotic Fluid
- Oligohydramnios
- Causes of Oligohydramnios
- Complications of Oligohydramnios
- Fetal Complications
- Maternal Complications
- Polyhydramnios
- Grades of Polyhydramnios
- Causes of Polyhydramnios
- Oligohydramnios
Placenta
Overview of the Placenta
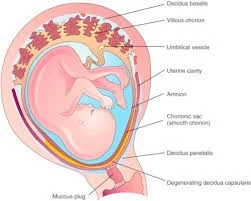
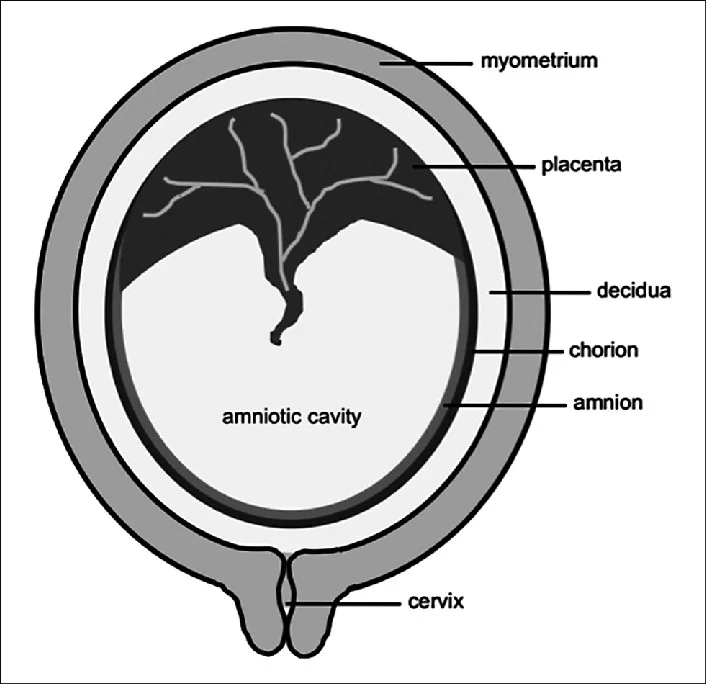
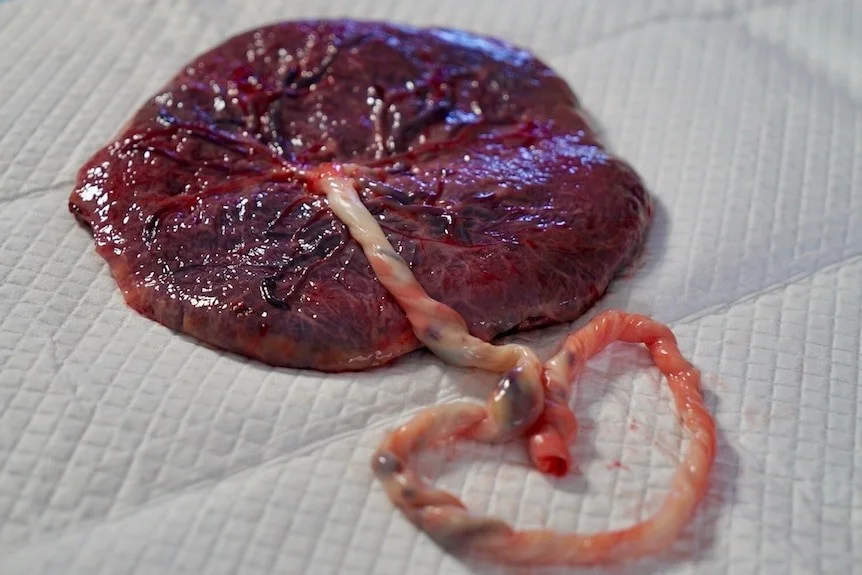
The human placenta is discoid, because of its shape; hemochorial, because of direct contact of the chorion with the maternal blood and deciduate, because some maternal tissue is shed at parturition.
The placenta attached to the uterine wall and establishes a connection between the mother and the fetus through the umbilical cord.
Development of Placenta
Formation and Components
The placenta is developed from two sources:
- Fetal component which develops from the Trophoblast.
- Maternal component consists of decidua basalis.
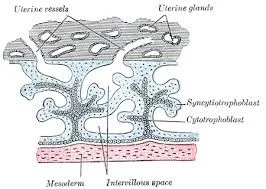
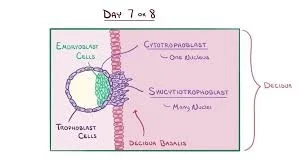
As fertilization of the ovum occurs and a zygote is formed, this cleavage continues till it is 16 cell staged and is called as Morula. The cells of the outer layer give rise to a structure called as the trophoblast. The trophoblast differentiates 7-9 days after fertilization into cytotrophoblast and syncytiotrophoblast. The trophoblast gives rise to the Amnion, Chorion, and the fetal side of the placenta.
The syncytiotrophoblast grows into the endometrium (Decidua). The maternal blood vessels are opened up and blood from them fills the lacunar space. So, lacunae have maternal blood. Each trabecula is, initially made up entirely of syncytiotrophoblast. Later, cells of cytotrophoblast begin to multiply and grow into each trabecula.
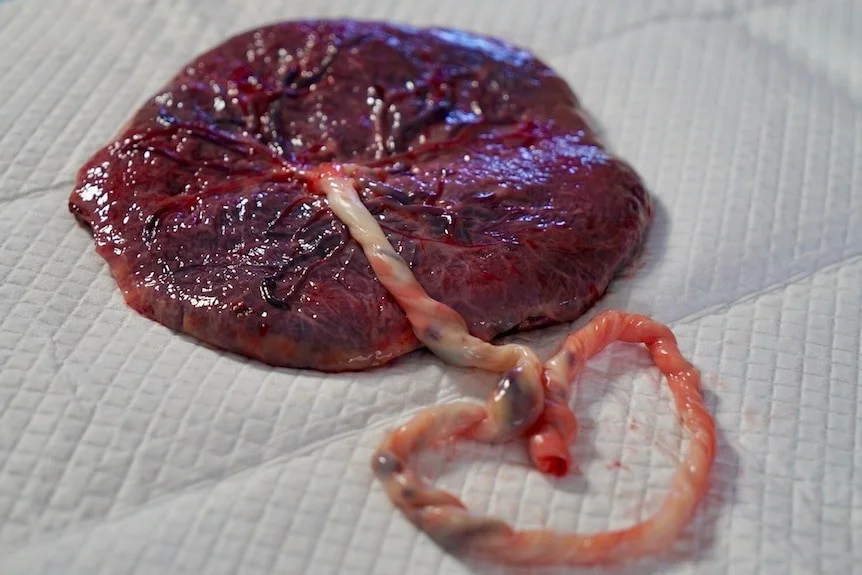
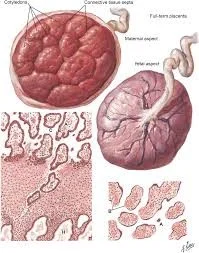
The Placenta at Term
The placenta, at term, is almost a circular disk with a diameter of 15–20 cm and a thickness of 3 cm at its center.
It weighs 500 gm.
It has two surfaces:
- Maternal surface: is rough and spongy.
- Fetal surface: is covered by the smooth and glistening amnion with the umbilical cord attached at or near its center. At term, about four-fifths of the placenta is of fetal origin.
- A cotyledon or lobule is the functional unit of the placenta.
- Only the decidua basalis and the blood in the intervillous space are of maternal origin.
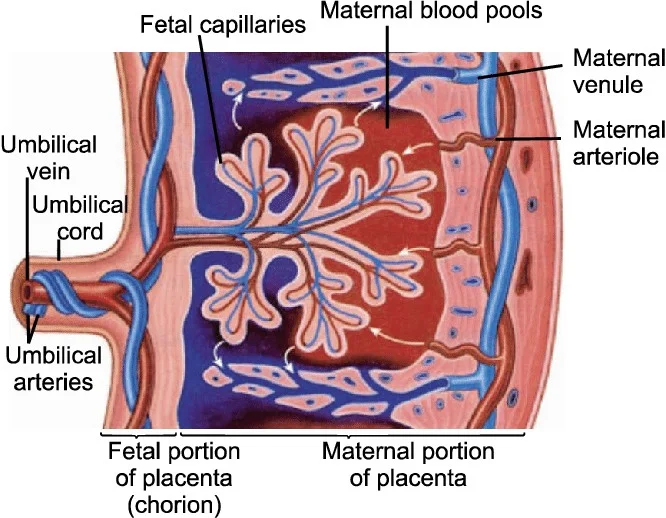
Placental Circulation
Types of Circulation
- Uteroplacental circulation: It is concerned with the circulation of the maternal blood through the intervillous space.
- Fetoplacental circulation: The two umbilical arteries carry the blood from the fetus to the placenta. Fetal blood circulation is around 400ml per min.
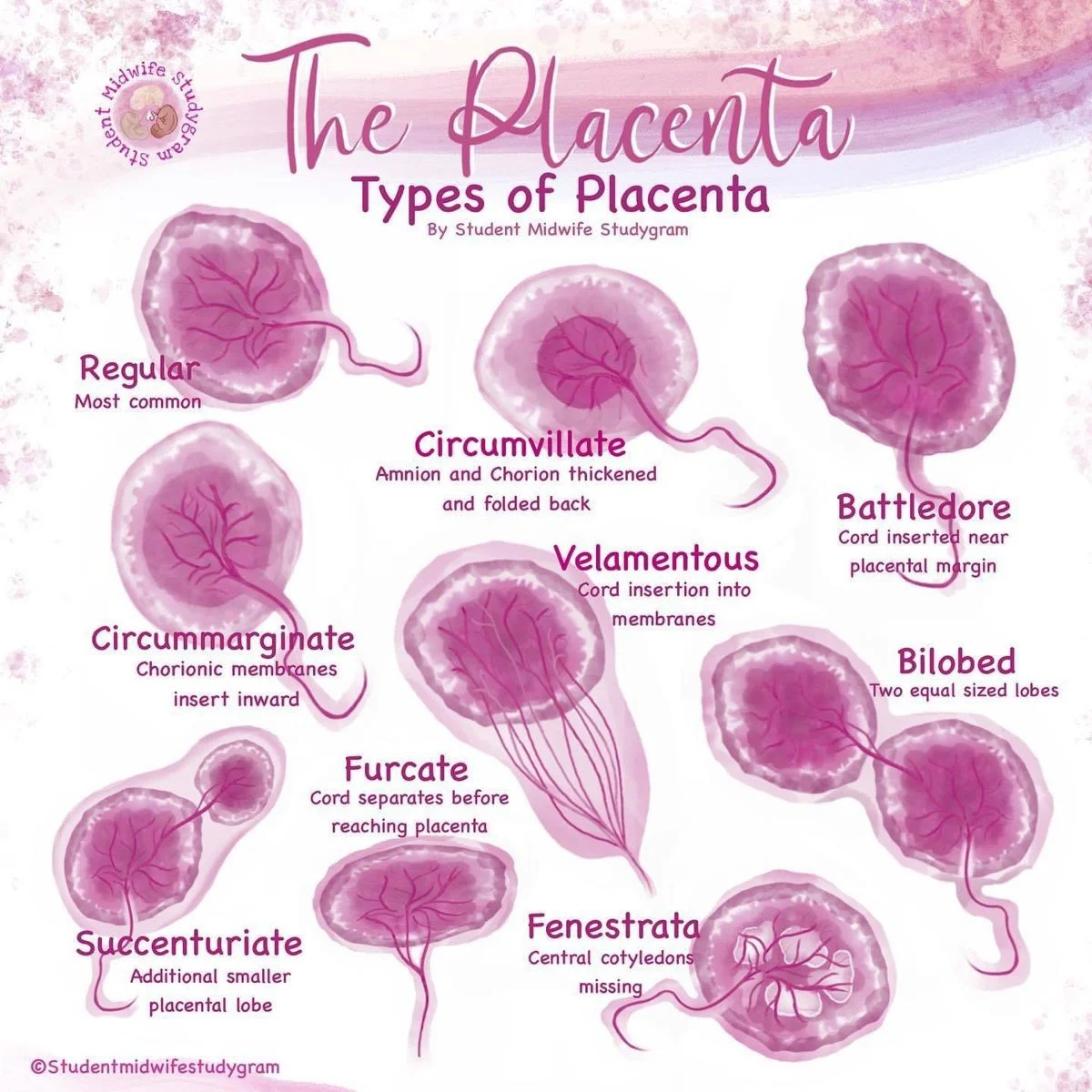
Types of Placenta
Umbilical Cord
The range is between 30-100 cm.
It has 2 arteries and one vein. The two arteries are smaller in diameter than the veins.
The extracellular matrix, which is specialized connective tissue, consists of Wharton’s Jelly.

Fetal Membrane
- Chorion (outer layer)
- Amnion (inner layer)
Function of Placenta
- Transfer of nutrient and waste products.
- Enzymatic function.
- Barrier function.
- Immunological function.
- Storage.
- Endocrine function.
Amniotic Fluid
The rate of amniotic fluid turnover is 500 cc/hr. The volume of Amniotic fluid is maximum between 36-38 weeks (1l) and then decreases such that at term it is roughly 800-900 ml.
Amniotic fluid originates both from maternal and fetal sources:
- In early pregnancy – As an ultrafiltrate of maternal plasma. By the beginning of the second trimester – It consists of extracellular fluid which diffuses through the fetal skin.
- After 20 weeks – Cornification of skin prevents this diffusion and amniotic fluid is composed of fetal urine.
Function of Amniotic Fluid
During Pregnancy
- It acts as a shock absorber, protecting the fetus from possible extraneous injury.
- Maintains an even temperature.
- The fluid distends the amniotic sac and thereby allows for growth and free movement of the fetus and prevents adhesion between the fetal parts and amniotic sac.
- It has some nutritive value.
During Labor
- The amnion and chorion are combined to form a hydrostatic wedge which helps in dilatation of the cervix.
Abnormality of Amniotic Fluid
OligohydramniosZ
Oligohydramnios is a condition where liquor amnii is deficient (< 200 ml at term).
Sonographically it is defined as:
- Absence of amniotic fluid pocket.
- Maximum vertical diameter of amniotic fluid pocket less than 2 cm.
- Amniotic fluid index less than 5 cm.
Causes of Oligohydramnios
- Drug (Prostaglandin Synthetase inhibitors and ACE inhibitors).
- IUGR.
- Leaking of fluid following amniocentesis or chorionic villus sampling.
- Maternal conditions like hypertension and preeclampsia.
- Post-term pregnancy.
- Premature rupture of membrane.
- Abruptiochronic.
- Chromosomal anomaly like triploidy.
- Renal anomalies of fetus.
Complications of Oligohydramnios
Fetal Complications
- Abortion.
- Deformity due to intra-amniotic adhesions or due to compression.
- Fetal pulmonary hypoplasia (may be the cause or effect).
- Cord compression.
- Fetal growth restriction.
Maternal Complications
- Prolonged labor.
- Increased operative interference due to malpresentation.
- The sum effect may lead to increased maternal morbidity.
Polyhydramnios
Defined when amniotic fluid index (AFI) is > 25 cm or finding of a pocket of fluid measuring 8 cm.
Grades of Polyhydramnios
- Mild: defined as pockets measuring 8-11 cm in vertical dimension.Z
- Moderate: defined as pocket measuring 12-15 cm in vertical dimension.
- Severe: defined as free-floating fetus found in pockets of fluid of 16 cm or more.
Causes of Polyhydramnios
- Fetus produces more urine, e.g.:
- Multifetal pregnancy (number of fetus is more: more urine).
- Maternal hyperglycemia/diabetes: Maternal hyperglycemia → Fetal hyperglycemia → Fetal polyuria → increased amniotic fluid.
- Twin to Twin transfusion syndrome.
- The amount of amniotic fluid will increase if fetal swallowing is impaired as in cases of:
- Cleft lip and cleft palate.
- Esophageal atresia or stenosis.
- Duodenal atresia or stenosis.
- Bowel obstruction.
- Anencephaly.
- Other Causes:
- Placental Causes: Chorangioma of placenta and circumvallate placenta.
- Fetal Causes: Hydrops fetalis, Rubella, syphilis, Toxoplasma infection of fetus, Trisomy (note – Triploidy leads to oligohydramnios), Sacrococcygeal teratoma, Thalassemia of fetus.
