Examination of the Hip
Prof. Mamoun Kremli
Lina Serhan
Orthopedic Examination System
The systematic approach to orthopedic examination includes:
- Look - Visual inspection
- Feel - Palpation
- Move - Range of motion assessment
- Special tests - Specific diagnostic maneuvers
Look
General Assessment
- General patient observation: Patient’s overall condition and comfort level
- Local hip-thigh-lower limb assessment:
- Position and alignment
- Major deformities and swelling
- External devices: casts, splints, traction, dressings
Anatomical Local Assessment
- Skin: Swelling, scars, color, hair distribution, dryness
- Subcutaneous tissue: Lymph nodes, veins, nerves, tendons
- Muscles: Bulk, wasting, fasciculations (twitches)
- Bones: Landmarks, swelling, angulation, deformity
- Joints: Position, swelling, redness
Important: Always examine the posterior aspect - all patients have a posterior aspect!
General Patient Position Examples
Normal Positioning
- Patient lying comfortably in bed, not in pain

Abnormal Positioning Examples
Left hip pathology:
- Patient lying uncomfortably in bed, in pain
- Left hip abducted and externally rotated

Bilateral hip pathology:
- Patient lying uncomfortably in bed
- Right hip adducted and internally rotated
- Left hip abducted and externally rotated

Severe bilateral involvement:
- Patient sitting uncomfortably in wheelchair
- Both hips adducted (scissoring)
- Left hip extended

Local Hip-Thigh-Lower Limb Assessment
Position Assessment
- Abduction/Adduction
- Flexion/Extension
- External/Internal Rotation

Postural Changes
- Lumbar lordosis: Increased curvature may compensate for hip pathology

Major Deformities and Swelling
- Lateralized contour
- Asymmetrical skin folds
- Wide perineum
- Masses



External Devices
Immobilization:
- Casts
- Splints


Traction:
- Skin traction
- Skeletal traction



Orthotics and Dressings:
- Orthotics:
- AFO (Ankle-Foot Orthosis)
- KAFO (Knee-Ankle-Foot Orthosis)
- HKAFO (Hip-Knee-Ankle-Foot Orthosis)
- Dressings: Various types and applications


Anatomical Local Examination (Detailed)
- Skin: Swelling, scars, color, hair, dryness
- Subcutaneous: Lymph nodes, veins, nerves, tendons
- Muscles: Quadriceps/Gluteii - bulk, wasting, fasciculations
- Bones: Landmarks, swelling, angulation, deformity
- Joints: Position (hip joint too deep to visualize swelling)
Feel
Palpation Assessment
-
Tenderness:
- Generalized: Diffuse tenderness
- Localized: Specific points of tenderness
-
Temperature: Compare distal/proximal and right/left sides
-
Anatomical structures:
- Skin: Dryness, hypo/hyperesthesia, scars
- Subcutaneous: Lymph nodes, nerves, vessels, tendons, nodules
- Muscles: Tone, bulk, fasciculations, gaps, tenderness
- Bone: Landmarks (ASIS, Greater Trochanter, Ischial Tuberosity), tenderness, masses, crepitus
- Joint: Swelling, effusion, crepitation, synovial thickening, joint line tenderness (hip joint too deep to elicit)
Move
Movement Assessment Principles
- Active vs. Passive: Start with active movement to screen for pain
- Passive assessment: Used when needed to evaluate:
- Painless vs. painful range of motion
- Muscle power assessment
Critical Technical Considerations
- Differentiate true hip joint motion from pelvic motion
- Stabilize the pelvis in neutral position
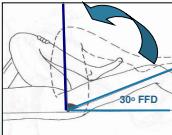
Important note: Patients with fixed hip flexion may appear to have full range when supine by tilting the pelvis forward, which creates increased lumbar lordosis.
Range of Motion Assessment
Flexion
- Initial position: Determined by Thomas Test
- Procedure:
- Check for lumbar lordosis
- Flex opposite hip fully
- Lumbar lordosis disappears
- Check hip position
- Flex hip to assess range
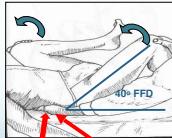
Range of motion: Flexion from 30° to 90°
- From 30° fixed flexion
- To 90° flexion

Extension
- Normal range: 30°
- Positions for assessment:
- Lateral position

- Prone position

Important: In presence of fixed flexion deformity, extension is already in “minus” range and doesn’t require assessment.
Abduction/Adduction
-
Normal ranges:
- Abduction: 45°
- Adduction: 15°
-
Pelvic stabilization techniques:
- Perform motion on both hips simultaneously
- Anchor knee of opposite side over examination table edge
- Palpate ASIS to assess pelvic motion
Both hips simultaneously:
- Stabilizes pelvis and compares both sides
- Can be performed in flexion or extension
Flexion

Extension

Alternative stabilization:
On both hips simultaneously
Stabilize pelvis and compare both sides

Edge of table technique:
Stabilizing the other hip at the edge of couch

ASIS palpation technique:
Holding ASIS to assess beginning of pelvic motion

Internal/External Rotation
- Must stabilize pelvis to prevent pelvic motion
- Best technique: Perform on both hips simultaneously
Assessment positions:
-
Supine with hips extended:
- Observe patella orientation

- Observe patella orientation
-
Supine with hips flexed:
- Use leg as pointer

- Prone with hips extended:

Special Tests
Thomas Test
Positive Thomas test in neonates and young children is normal
Purpose: Detect fixed flexion deformity of the hip
Procedure:
- Assess lumbar lordosis before testing
- Precaution: When knee has fixed flexion deformity, keep knee outside edge of couch
Precaution ⇒ when knee has fixed flexion deformity Solution ⇒ keep knee outside edge of couch


Trendelenburg Test
Purpose: Assess hip abductor strength and stability
Principle: Testing the hip the patient is standing on
- Normal: Pelvis tilts down on weight-bearing hip (performed by hip abductors)
- Positive: Pelvis on non-weight-bearing hip tilts down AND trunk tilts to weight-bearing side





Causes of Positive Trendelenburg
- Weak hip abductors:
- Paralyzed/wasted muscles
- Mechanically inefficient hip abductors:
- Reduced distance between origin and insertion (e.g., coxa vara)
- Unstable pivot of motion:
- Hip subluxation/dislocation
- Inhibited hip abductors:
- Painful to move (trauma, infection, irritation, tumor)
- Reduced range of motion:
- Hip incongruency, stiffness, osteoarthritis
Note: Almost any hip disease can cause a positive Trendelenburg test
Leg Length Assessment
Galleazzi Test
Purpose: Detect leg length discrepancy
Technique: Both heels must be at the same level


Leg Length Measurements
Apparent Length:
- Measurement: Midpoint to medial malleolus
- Affected by: Pelvic tilt
Both lower limbs - Should be Parallel

True Length:
- Measurement: ASIS to medial malleolus
- Not affected by Pelvic tilt
Position of both lower limbs - Should be identical

Additional measurement examples:


Neonatal Examination for Developmental Dysplasia of the Hip (DDH)
Ortolani Test
Purpose: Reduces a dislocated hip
- Expected finding: Feel a “clunk” (not a “click”)

Barlow Test
Purpose: Dislocates a reduced hip
- Expected finding: Feel a “clunk” (not a “click”)

Combined Ortolani/Barlow technique:


Gait Assessment
Normal Gait Cycle
- Stance phase: 60% of gait cycle
- Heel strike
- Foot flat - mid-stance
- Push off

- Swing phase: 40% of gait cycle
- Acceleration
- Mid-swing
- Deceleration
Abnormal Gait Patterns
| Gait Type | Explanation |
|---|---|
| Normal | Normal stance and swing phases |
| Antalgic | Painful to weight-bear - short stance phase |
| Lurch | Shortening - painless limping - normal stance period |
| Circumduction | Stiff hip - motion of pelvis compensates |
| High Step | Foot drop - more hip & knee flexion needed to free toes from ground |
| Tip-toe | Heel off the ground -l4/l5 |
Summary
Systematic approach to clinical examination in orthopedics:
- Look, Feel, Move, Special tests
- Sub-system helps ensure no steps are forgotten
Key considerations for hip examination:
- Important exposure considerations
- In “Move” assessment, must stabilize pelvis
- Special tests: Thomas, Trendelenburg, instability tests, length measurements
- Gait assessment is essential