Clinical Case Scenarios
Knee Pain and Degenerative Disease
Dr. Tarif Alakhras
Case 1: Lady with Chronic Knee Pain
Patient Presentation
- 54 year old lady, presented to the clinic with pain in both knees for 3 years
- No clear history of trauma
Comprehensive History
Pain Assessment
- Characteristics: Site, onset, character, radiation, associated symptoms, time course
- Severity: Exacerbating and relieving factors
- Impact: Activity and pain relationship, sleep disturbance
Medical Background
- Occupational status and physical activity level
- Current medications
- Comorbidities and previous surgical history
- Menopausal status
- Dietary habits
Clinical Examination
General Assessment
- Pain level and patient comfort
- Weight status (overweight evaluation)
- General appearance (ill-looking, anemic signs)
Local Examination
Position and Attitude
- Patient positioning and attitude
- Extra-articular findings
Systematic Examination: Look, Feel, Move
 Figure: Clinical examination approach for knee assessment
Figure: Clinical examination approach for knee assessment
Diagnostic Investigations
Laboratory Studies
- General: Complete blood count, inflammatory markers
- Specific: Metabolic panel, rheumatoid factor if indicated
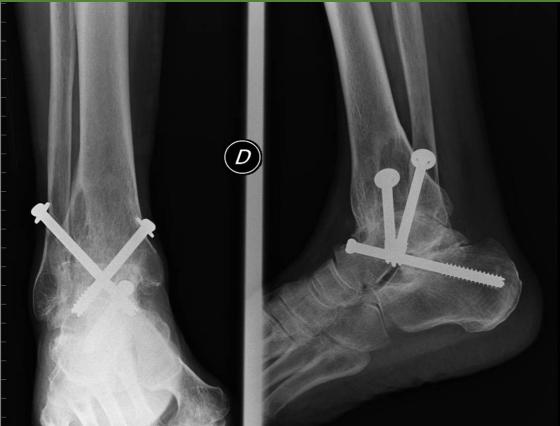
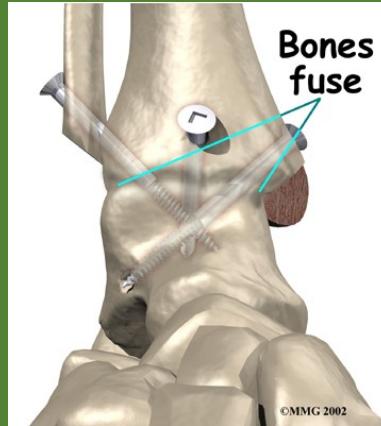
Imaging Studies
- Standard Radiographs:
- Both knees AP standing views (weight-bearing)
- Lateral views of both knees
- Skyline view (patellofemoral assessment)






Management Strategy
Conservative Management
- Lifestyle Modifications:
- Weight reduction program
- Walking aid prescription
- Physical therapy regimen
Medical Management
- Pain management: NSAIDs, analgesics
- Disease-modifying agents when appropriate
- Intra-articular injections (steroids, hyaluronic acid)
Surgical Considerations
- Timing: When conservative measures fail
- Options:
- Arthroscopy (selective cases)
- Osteotomy (young patients with unicompartmental disease)
- Total knee arthroplasty (end-stage disease)




Case 2: Young Patient with Acute Knee Injury
Patient Presentation
- 25 years old patient came to the clinic complaining of right knee pain
- History of acute sports injury
Injury Mechanism
Acute Phase
- Immediate acute pain following injury
- Mechanism of injury:
- Violent rotation with flexion (classic ACL injury pattern)
- Swelling characteristics:
- Immediate swelling (indicates hemarthrosis - intra-articular bleeding)
- Delayed swelling (suggests reactive effusion)
Subacute and Chronic Phase
- History of giving way episodes (sudden knee instability)
- Repeated attacks of swelling and pain
- Progressive functional limitation
Clinical Examination Findings
Physical Signs
- Swelling pattern:
- Initially: Hemarthrosis (blood in joint)
- Later: Chronic effusion
- Muscle changes: Wasting of quadriceps muscle
- Functional instability
Special Ligament Tests
- Anterior drawer test (ACL integrity)
- Lachman’s test (gold standard for ACL)
- Pivot shift test (functional instability assessment)

Diagnostic Imaging
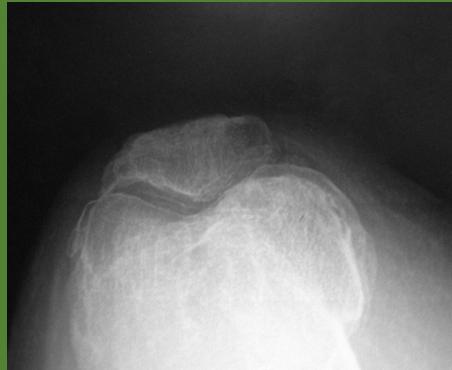
Hip osteoarthritis comparison images: * Hip without Osteoarthritis (for comparison)

Treatment Approach
Non-Surgical Management
- Physical therapy:
- Quadriceps strengthening
- Proprioceptive training
- Range of motion exercises
- Activity modification
- Bracing (for selected cases)
Surgical Indications
- Active individuals with instability
- Recurrent instability episodes
- Failed conservative management
- Early arthritic changes





Post-Operative Rehabilitation
- Phase 1: Protected motion, early controlled motion
- Phase 2: Strengthening and proprioception
- Phase 3: Return to specific activities
- Phase 4: Return to sports (typically 6-9 months)