Surgery
Shock
Septic Shock
Bacteremia: - It is the presence of bacteria within the bloodstream.
Sepsis: - - is the systemic response to infection and - It is defined as the presence of SIRS in addition to a documented or presumed infection i.e., infection-induced syndrome involving 2 or more manifestations of SIRS.
Severe sepsis meets the a forementioned criteria and is associated with organ dysfunction, hypoperfusion, or hypotension.
Septic Shock
Severe Sepsis induced hypotension (systolic < 90 mmHg). Disturbance in O₂ delivery and O₂ consumption. Gram positive (52%), Gram negative (38%) infections.
Common sites of infection:
- Lung (50-70%), (respiratory)
- abdomen (20-25%) ,
- urinary tract (5-7%),
- skin.
Risk groups:
- Immunocompromised
-
65 years or older
- Infants under 1 year

Pathophysiology
-
Infection- triggers cytokines (TNF-α, IL 1-β) mediated pro-inflammatory response.
-
Peripheral vasodilatation due to NO release
-
Fall in systemic vascular resistance
-
Reflex tachycardia, increased cardiac output (CO)- High output state.
-
Clinically: warm well perfused periphery
-
Low diastolic BP, wide pulse pressure.
Septic Shock- pathophysiology
If septic state persists: Endothelium dysfunction leads to: - Extravasation of fluid - Loss of intravascular volume - Ventricular dysfunction → impairs CO. - Peripheral perfusion falls
Clinically indistinguishable from low output state
Features of warm and cold shock
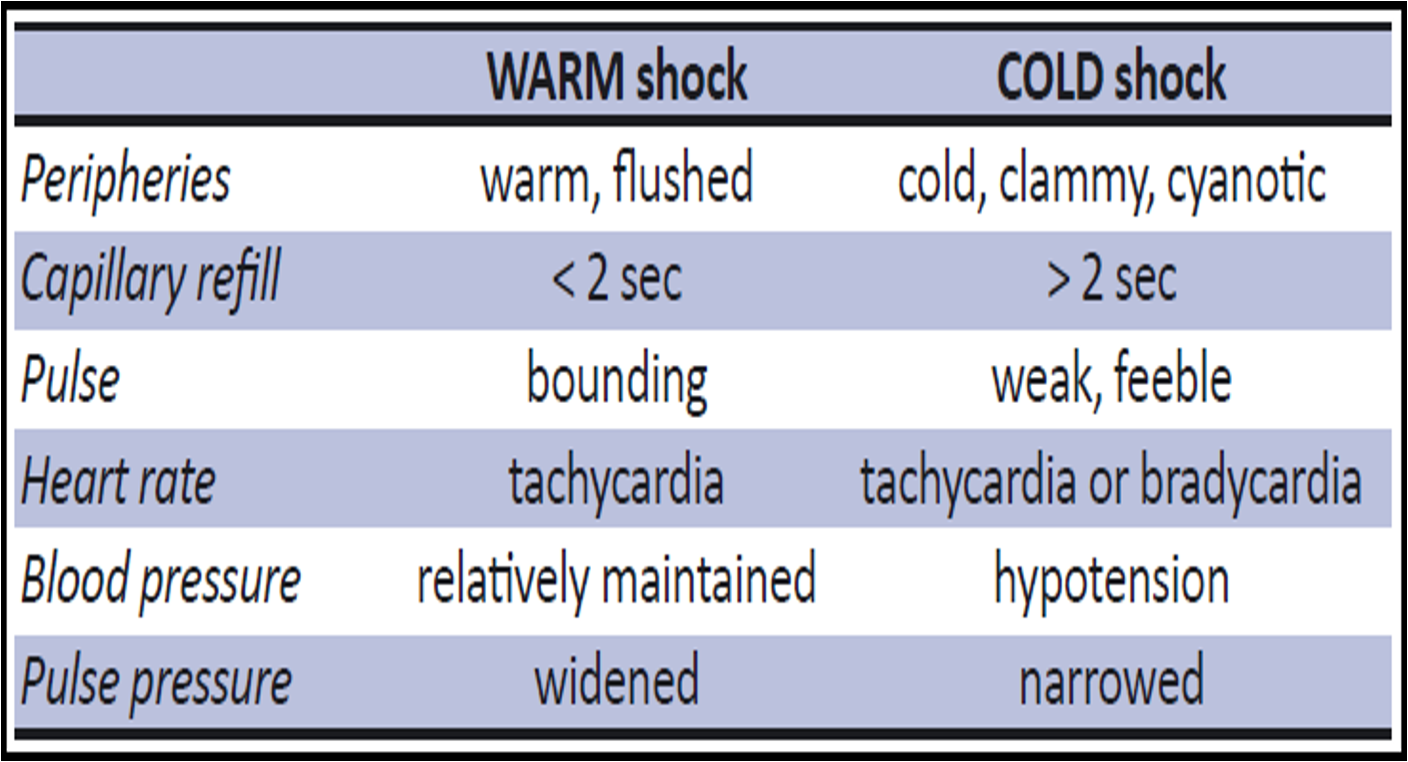
EARLY WARM SHOCK (WARM shock)
-
Compensated warm phase of shock.
-
Prompt response to fluids and pharmacologic treatment.
-
Toxins increase the body temperature.
-
Arterial blood pressure falls but the cardiac output increases because the left ventricle has minimal resistance to pump against.
-
Adrenergic discharge further Increases the cardiac output. The skin remains pink, warm & well perfused (Cutaneous vasodilatation).
LATE COLD SHOCK (Refractory septic shock)
-
Late decompensated phase.
-
There is hypovolemia with decrease in right heart filling & decreases cardiac output.
-
The knowledge of existence of a septic focus is the only factor that differentiates septic shock from traumatic & hypovolemic shock.
Treatment:
1) Aim of treatment is to:
- a- control infection and
- b- improve the hypovolemic state, caused by endotoxin induced peripheral vasodilatation.
2) Blood culture should be done before antibiotic administration.
3) Debridement & drainage of the infection.
4) Antibiotics: combination of 3rd generation cephalosporin, aminoglycoside and metronidazole should be effective against most organisms.
5) Inotrope (Cardiogenic + Septic) use is indicated in severely ill patients to maintain cardiac output.
Truama
Septic shock
- Delayed arrival
- Penetrating abdominal injuries
- Early septic shock- normal circulating volume
- Tachycardia
- Warm skin
- Systolic BP is near to normal
- Wide pulse pressure