Pharmacological Effects
- on carbohydrate :decreases blood glucose
- On fat : decreased fat breakdown - results in increased obesity with non-optimal diet for DM2 & Obesity
- On protein metabolism :decreased breakdown (anabolic effect): Long-term actions: Stimulation of cell proliferation - for normal growth
- On electrolytes: decrease potassium ,PO4, Ca++, magnesium blood concentration due to uptake into cells with glucose.
- Antiketogenic: decrease ketone bodies (acetone, AAA, BHBA) in the liver and help ketolysis
MOA of insulin:
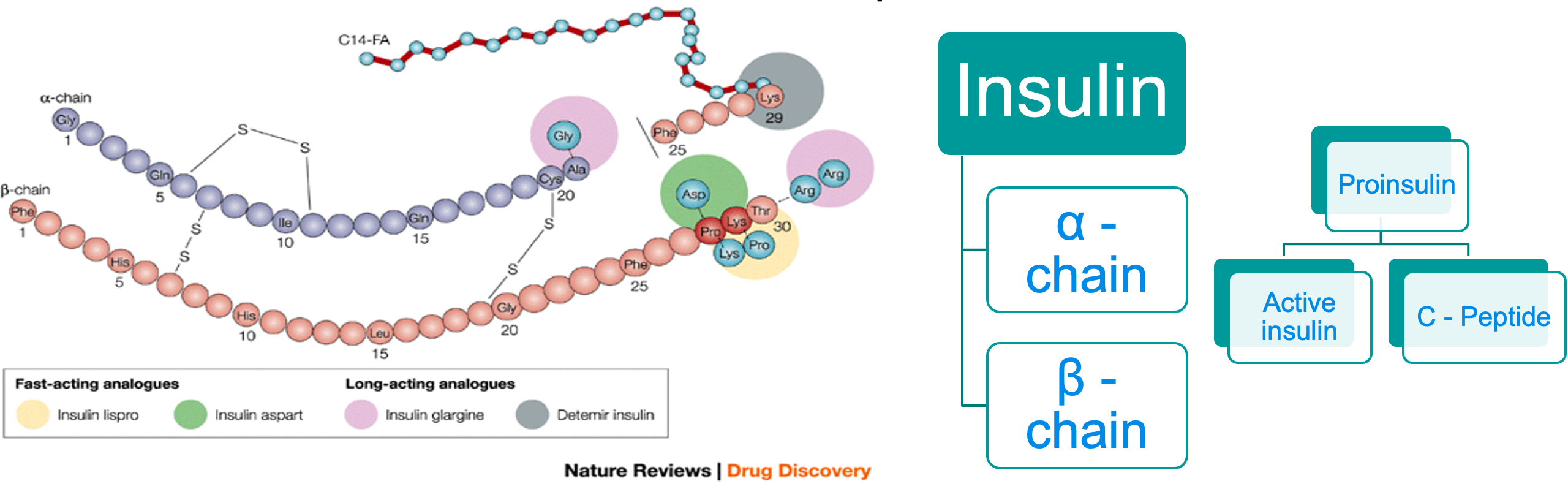
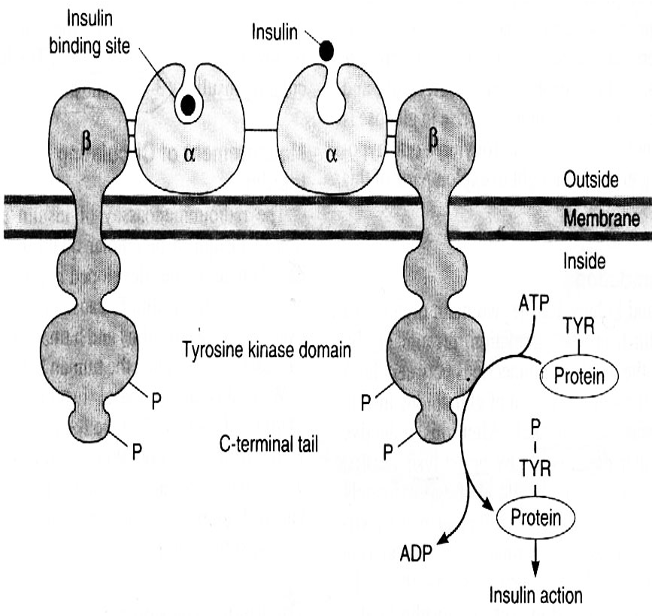
Insulin receptors: Structure: 2 extra-cellular α-subunits & 2 trans-membrane β-subunits.
Mechanism of action: Binding of insulin to α-subunits → ++ of β-subunits → ++ of tyrosine kinase enzyme → trigger series of IC effects → ↑ number of glucose transporters (especially GLUT4) on cell membrane → ↑ transport of glucose into the cell.
After doing its action, insulin-receptor complex is internalized by endocytosis.
 Cell membranes are impermeable to glucose, they require a special carrier, called a glucose transporter, to move glucose from the blood into the cell.
Cell membranes are impermeable to glucose, they require a special carrier, called a glucose transporter, to move glucose from the blood into the cell.
GLUT-4 is the insulin-dependent glucose transporter for skeletal muscle and adipose tissue Z
GLUT-2 is the major transporter of glucose into beta cells and liver cells. It has a low affinity for glucose and acts as a transporter only when plasma glucose levels are relatively high, such as after a meal.
GLUT-1 is present in all tissues. It does not require the actions of insulin and is important in transport of glucose into cells of the nervous system.
Factors that ↑ affinity of insulin receptors (up-regulation):
Insulin deficiency (e.g. starvation) → ↑ number of receptor. Drugs:
- Thiazolidinediones: e.g pioglitazone, rosiglitazone.
- Sulphonylureas: e.g gliclazide.
- Biguanides e.g
- Trace elements: e.g selenium and chromium.
Factors that ↓ affinity of insulin receptors (down-regulation)
- Obesity - DM2
- Drugs: e.g. Corticosteroids…….
Sources of insulin: Y
- Traditional (animal) insulin: prepared from: animals (beef and pork).
- Pork insulin differs from human insulin in 1 aa (alanine in pork and threonine in human) while beef insulin differs from human in 3 aa.
- Human insulin:
Human insulin: prepared by 2 methods:
- From pork insulin by chemical replacement of alanine by threonine.
- Recombinant DNA technology (genetic engineering).
Advantages of human insulin:
- Highly purified
- least antigenic.
- Rare resistance.
- Used in insulin resistance and gestational DM.
Administration
- Insulin is administered either IV, IM or SC. Oral, inhaled ………………
Insulin Therapy
The duration of action of insulin can be varied by:
-
Modification of the insulin molecule (by recombinant technology)
-
Conjugation of insulin with protamine in a low soluble complex. After injection proteolytic enzymes degrade protamine so allowing absorption of insulin.
-
Combination of insulin with zinc, to form zinc salts. After injection the salt precipitates and insulin is slowly released.
Different PREPARATIONS of insulin:
Onset & Duration Z
- Ultrashort -ACTING INSULIN: Insulin Lispro & Aspart
- SHORT-ACTING INSULIN:
- Intermediate-ACTING INSULIN
- Long-Acting Insulin
- Mixture of Insulin
- Pre-mixed formulations (Biphasic) of 30% regular (short) and 70% NPH (intermediate): provide rapid onset and prolonged duration.

Insulin administration
Side effects of insulin: Local side effects:
-
Allergy: at the site of injection (due to formation of IgGE). Treatment:
- Change the type of insulin to more purified preparation. change site injection regularly
- Local corticosteroids or antihistamines.
-
Lipodystrophy: atrophy or hypertrophy of s.c tissue after repeated injections. Treatment:
- Change the site of injection regularly.
- In lipoatrophy, give cone purified regular insulin in the center and periphery of the atrophic area to stimulate lipogenesis.
-
Local infection.
Systemic side effects:
- Hypoglycemia: the most common and dangerous side effect.
- Hypokalemia: insulin causes shift of K+ from extracellular to intracellular fluid.
- Hypersensitivity reactions: urticaria, angioedema or anaphylactic shock.
- Weight gain
Other Effects:
- Insulin resistance (IR)
- Pseudo-insulin resistance (Somogyi phenomenon):
- Dawn phenomenon
Events Requiring an Increase in Dosage of Insulin in Diabetic Patients
- Infections
- High fever
- Trauma, surgical operations
- Myocardial infarction
- Pregnancy
- Hyperthyroidism
- Diabetic ketoacidosis