Pediatrics
PNEUMONIA
DEFINITION AND EPIDEMIOLOGY
PNEUMONIA is a primary inflammation of lung parenchyma. Viruses are the most common cause in younger children, while bacteria are commoner in older children.
Mortality:
- The mortality rate in developed countries is low (<1 per 1000 per year). In developing countries, pneumonia is the number one killer of children in these societies.
Seasonality:
- Pneumonia is most common in winter and spring.
Medical conditions predispose to pneumonia and contribute to increasing severity:
- Congenital heart disease
- Bronchopulmonary dysplasia
- Cystic fibrosis
- Asthma
- Sickle cell disease
- Neuromuscular disorders, especially those associated with a depressed consciousness
- Some gastrointestinal disorders (e.g., gastroesophageal reflux, tracheoesophageal fistula)
- Congenital and acquired immunodeficiency disorders
AGE SPECIFIC ETIOLOGY OF PNEUMONIA
| AGE GROUP | FREQUENT PATHOGENS (IN ORDER OF FREQUENCY) |
|---|---|
| Neonates (<3wk) | Group B streptococcus, Escherichia coli, other gram-negative bacilli, Streptococcus pneumoniae, Haemophilus influenzae (type b,* nontypeable) |
| 3wk-3mo | Respiratory syncytial virus, other respiratory viruses (rhinoviruses, parainfluenza viruses, influenza viruses, human metapneumovirus, adenovirus), enterovirus D68, S. pneumoniae, H. influenzae (type b,* nontypeable); if patient is afebrile, consider Chlamydia trachomatis |
| 4mo-4yr | Respiratory syncytial virus, other respiratory viruses (rhinoviruses, parainfluenza viruses, influenza viruses, human metapneumovirus, adenovirus), enterovirus D68, S. pneumoniae, group A streptococcus |
| ≥5yr | M. pneumoniae*, S. pneumoniae, Chlamydophila pneumoniae, H. influenzae (type b,* nontypeable), influenza viruses, adenovirus, COVID-19, other respiratory viruses, Legionella pneumophila |
* H. influenzae type b is uncommon with routine immunization.
Adapted from Kliegman RM, Jenson HJ, et al., eds. Nelson Essentials of Pediatrics, 5th ed. Philadelphia: Elsevier; 2006: p. 507.
strep p. most common

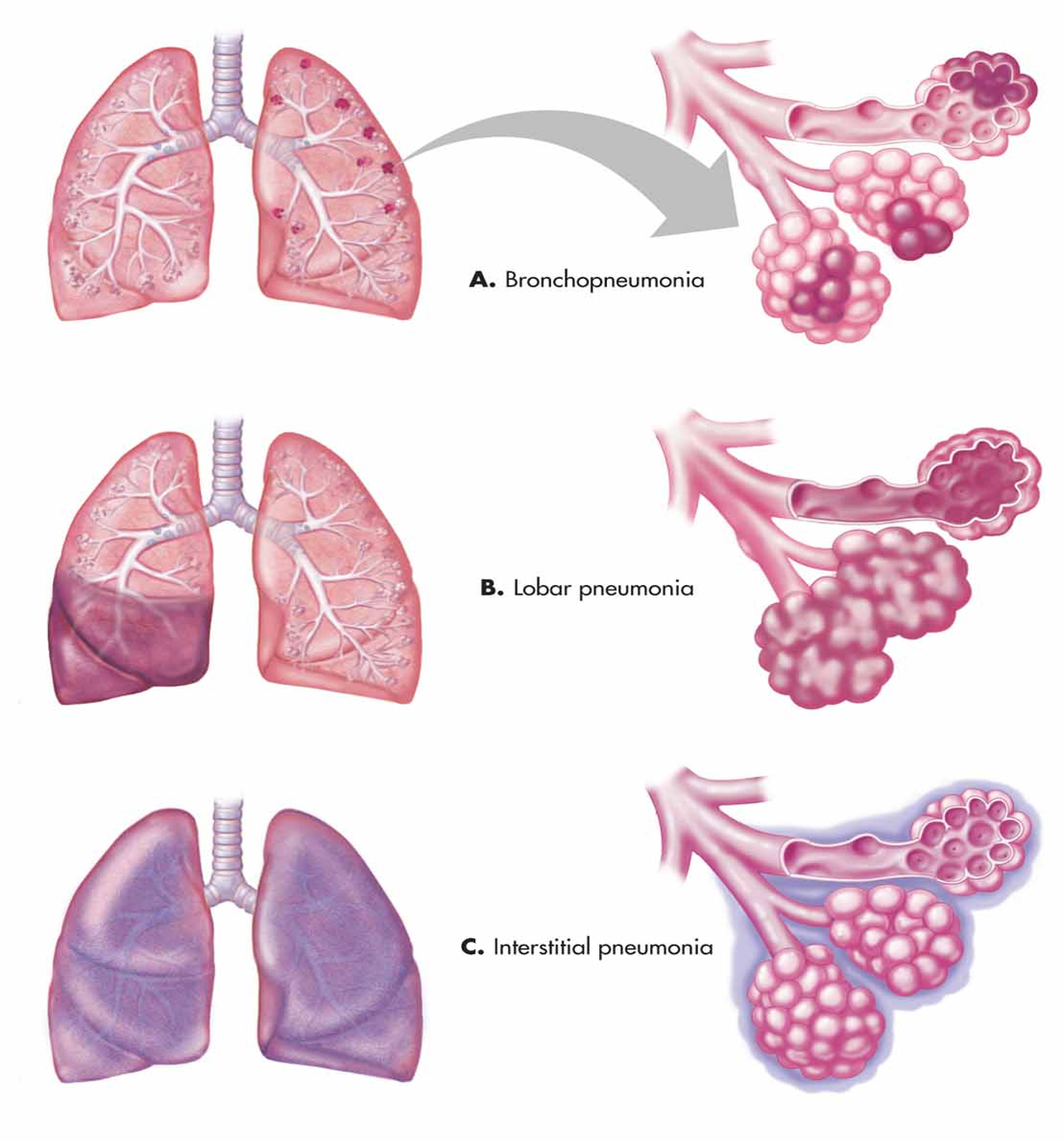
ANATOMICAL TYPES OF PNEUMONIA
-
Lobar pneumonia:
- Involvement of a single lobe or segment of a lobe; this is the classic pattern of S. pneumoniae pneumonia
-
Bronchopneumonia:
- Primary involvement of airways and surrounding interstitium; this pattern is sometimes seen in Streptococcus pyogenes and Staphylococcus aureus pneumonia
-
Necrotizing pneumonia:
- Associated with aspiration pneumonia and pneumonia resulting from S. pneumoniae, S. pyogenes, and S. aureus)
-
Caseating granuloma (as in tuberculosis pneumonia)
-
Interstitial and peribronchiolar with secondary parenchymal infiltration:
- This pattern typically occurs when a severe viral pneumonia is complicated by bacterial pneumonia
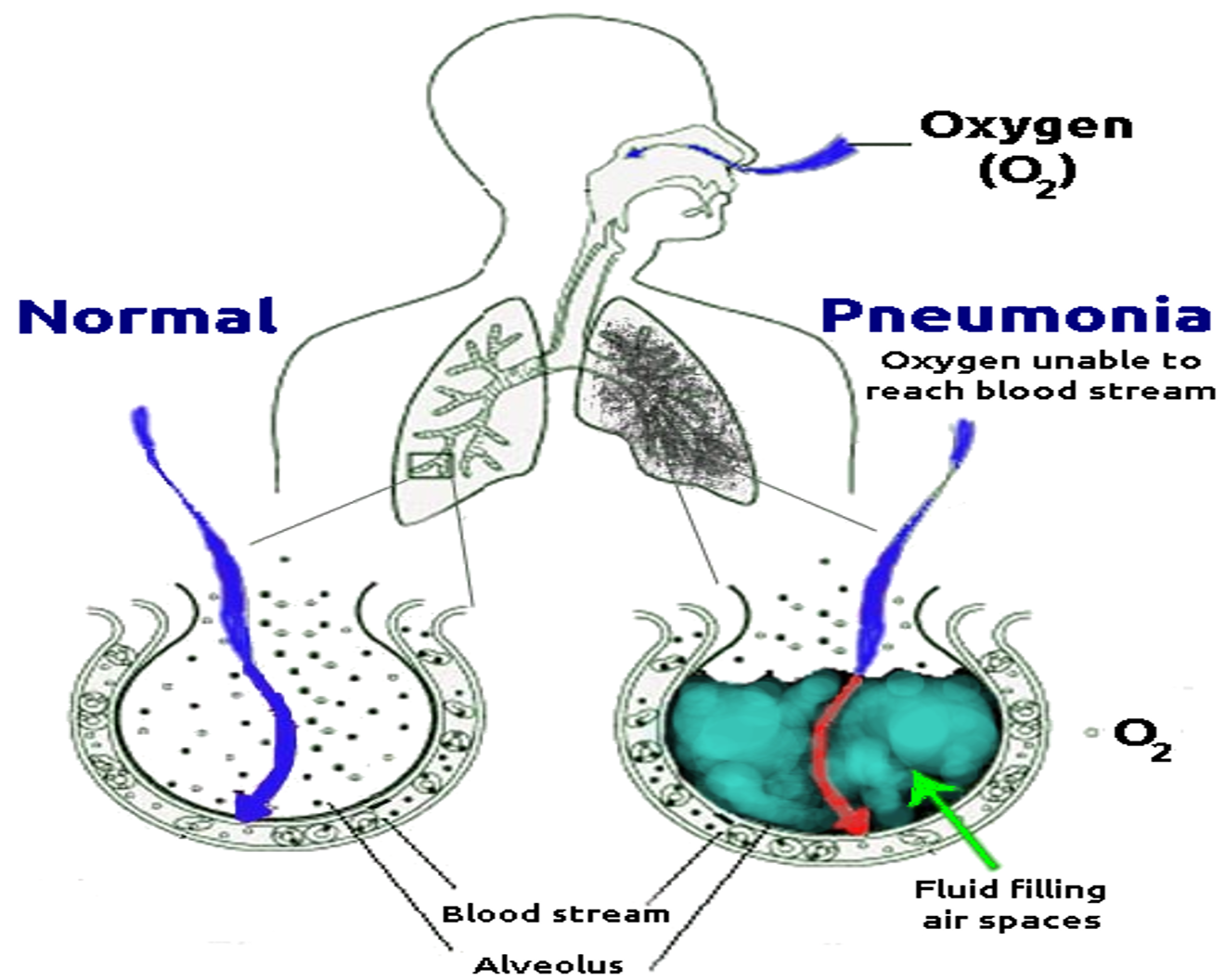
Pathophysiology
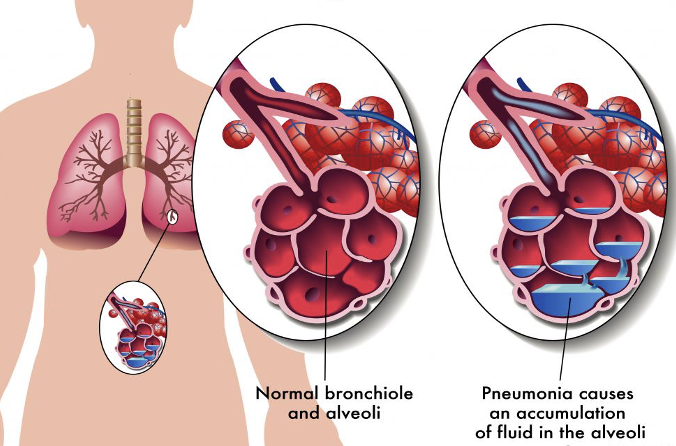
- Bacteria enter the lungs (from the throat or nose, airborne droplets, or blood).
- Bacteria may invade the spaces between cells and between alveoli.
- The macrophages and neutrophils inactivate the bacteria. The neutrophils also release cytokines.
- This causes general activation of the immune system.
- Leading to fever, chills, and fatigue.
- The neutrophils, bacteria, and fluid fill the alveoli.
- Resulting in the consolidation seen on chest X-ray.
CLINICAL PICTURE
Presenting features vary with age, infectious agent, and severity or stage of the illness.
- Fever, cough (productive or non-productive), and difficulty breathing are common presenting symptoms, often preceded by signs of a minor upper respiratory tract infection.
- Chest or stomach pain.
- Decrease in appetite.
- Chills.
- Breathing fast or hard.
- Vomiting.
- Headache.
- Not feeling well.
Examination This includes assessment for:
- Fever:
-
38.5°C is a feature of bacterial pneumonia
-
- Oxygenation:
- Cyanosis indicates severe illness.
- Pulse oximetry identifies significant hypoxemia (SaO2 <92% in air)
- Respiratory rate:
- Tachypnea is a useful indicator of pneumonia.
- Rates defined by the WHO provide a 74% sensitivity for radiologically defined pneumonia:
AGE RESPIRATORY RATE
<2 months >60 breaths/min
2–12 months >50 breaths/min
1-5 years >40 breaths/min
5-10 years >30 breaths/min
Work of breathing:
- Chest recession, nasal flaring, and grunting are most sensitive in children aged <3 years.
Examination feature
Percussion and auscultation: Examination findings consistent with radiographically confirmed pneumonia include:
Crackles, also called rales or crepitations; in a systematic review, crackles were 3.5 times more frequent in infants with radiographic pneumonia than without.
- Findings consistent with consolidated lung parenchyma, including: - Decreased breath sounds - Bronchial breath sounds. - Bronchophony (the distinct transmission of sounds such as the syllables of “ninety-nine”) - Whispered pectoriloquy (transmission of whispered syllables) - Tactile fremitus (e.g., when the patient says “ninety-nine”) is increased - Dullness to percussion
Wheezing
- is more common in pneumonia caused by atypical bacteria and viruses than bacteria.
- Findings suggestive of pleural effusion include chest pain with splinting, dullness to percussion, distant breath sounds, and a pleural friction rub.
| Examination feature | Possible significance |
|---|---|
| General appearance (state of awareness, cyanosis)* | Most children with radiographically confirmed pneumonia appear ill |
| Vital signs | |
| Temperature | Fever may be the only sign of pneumonia in highly febrile young children; however, it is variably present and nonspecific |
| Respiratory rate | Tachypnea correlates with radiographically confirmed pneumonia and hypoxemia. Absence of tachypnea helps to exclude pneumonia |
| Degree of respiratory distress | Respiratory distress is more specific than fever or cough for lower respiratory infection |
| Tachypneax Hypoxemia | Predictive of pneumonia |
| Increased work of breathing: | |
| Retractions | More common in children with pneumonia than without; absence does not exclude pneumonia |
| Nasal flaring | More common in children with pneumonia than without; absence does not exclude pneumonia |
| Grunting | Sign of severe disease and impending respiratory failure |
| Accessory muscle use | Sign of severe disease |
| Head bobbing | Sign of severe disease |
| Lung examination | |
| Cough | Nonspecific finding of pneumonia |
| Auscultation | Findings suggestive of pneumonia include: crackles (rales, crepitations), decreased breath sounds, bronchial breath sounds, egophany, bronchophony, and whispered pectoriloquy. Wheezing more common in viral and atypical pneumonias |
| Tactile fremitus | Suggestive of parenchymal consolidation |
| Dullness to percussion | Suggestive of parenchymal consolidation or pleural effusion |
| Mental status | Altered mental status may be a sign of hypoxia |
INVESTIGATIONS
-
Full blood count and acute phase reactants
- Total leukocyte and neutrophil count.
- C-reactive protein.
- ESR have poor sensitivity and specificity for distinguishing between viral and bacterial pneumonia.
-
Microbiological investigations
- Blood cultures:
- The yield is low and a positive result takes 48–72 h. Positive in 10–15% of patients with pneumococcal pneumonia.
- Respiratory tract samples:
- Sputum for culture is rarely available and samples are frequently contaminated.
- Nasopharyngeal aspirate (NPA) for viral immunofluorescence assay or PCR is useful in infants. Bronchoscopy or pleural fluid aspiration may provide samples.
- Serology:
- Paired serology 14 days apart is available for diagnosis of mycoplasma but treatment is usually given on empirical grounds.
- Blood cultures:
IMAGING
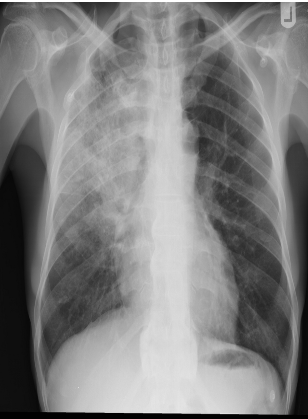
- CXR:
- The appearance of consolidation on CXR is reliable for the diagnosis of pneumonia, but CXR appearances are not reliable for distinguishing between viral and bacterial infection as there is considerable overlap.
- The CXR may appear normal early in the disease. However, as an approximate guide:
- Viral pneumonia:
- Patchy perihilar infiltration, hyperinflation, atelectasis
- Bacterial pneumonia:
- Lobar consolidation (air bronchogram) occasionally with parapneumonic effusion. Pneumatocoele and abscesses suggest staphylococcal pneumonia
- Mycoplasma pneumonia: most commonly school age
- Patchy, segmental consolidation with hilar lymphadenopathy.
- Viral pneumonia:
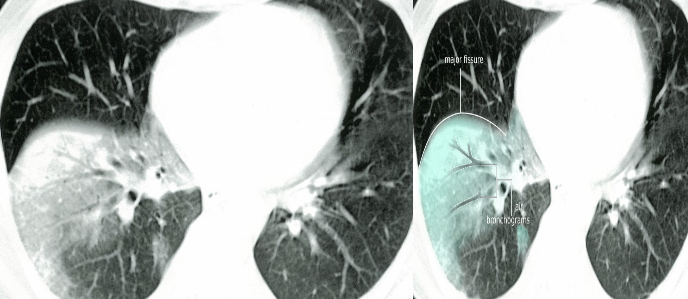
Chest X-Ray showing patch of pneumonia
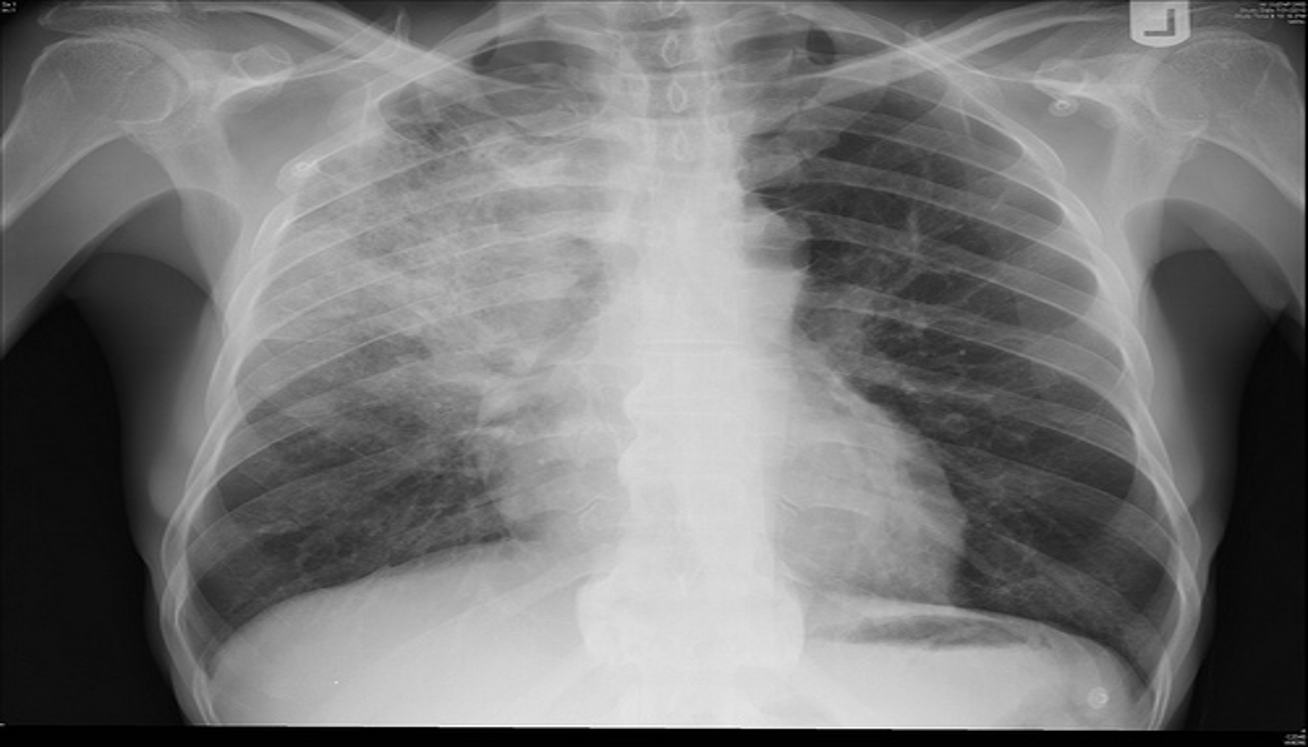
Image of chest x-ray displaying the interstitial pattern seen in viral pneumonia. The interstitial pattern shows fine lines radiating from the hila.

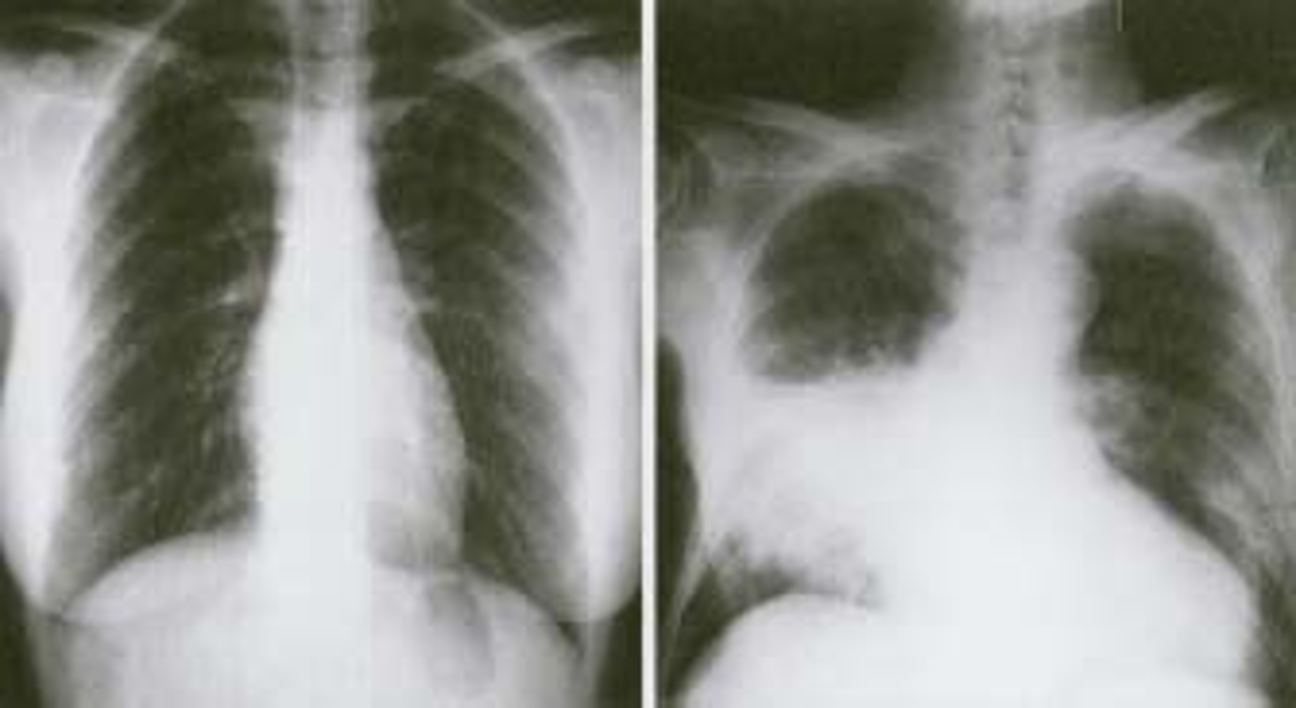
These chest X rays compare clear, healthy lungs with the cloudy, inflamed lung tissue of pneumonia.
Right lower lobe consolidation in a patient with bacterial pneumonia.

Anteroposterior radiograph from a child with a round pneumonia.

X-ray view of mycoplasma pneumonia
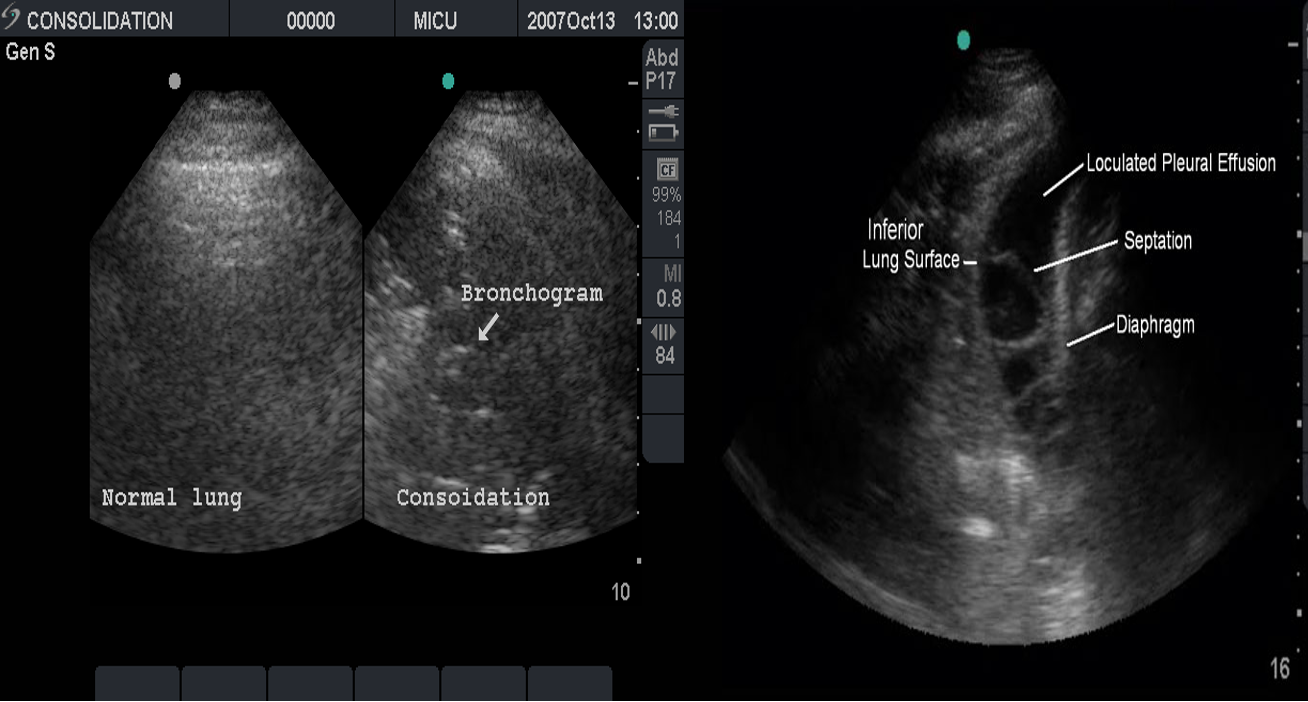
Ultrasound:
This is most useful if a pleural effusion is suspected on CXR. It can differentiate between clear fluid and fibrino-purulent effusions.
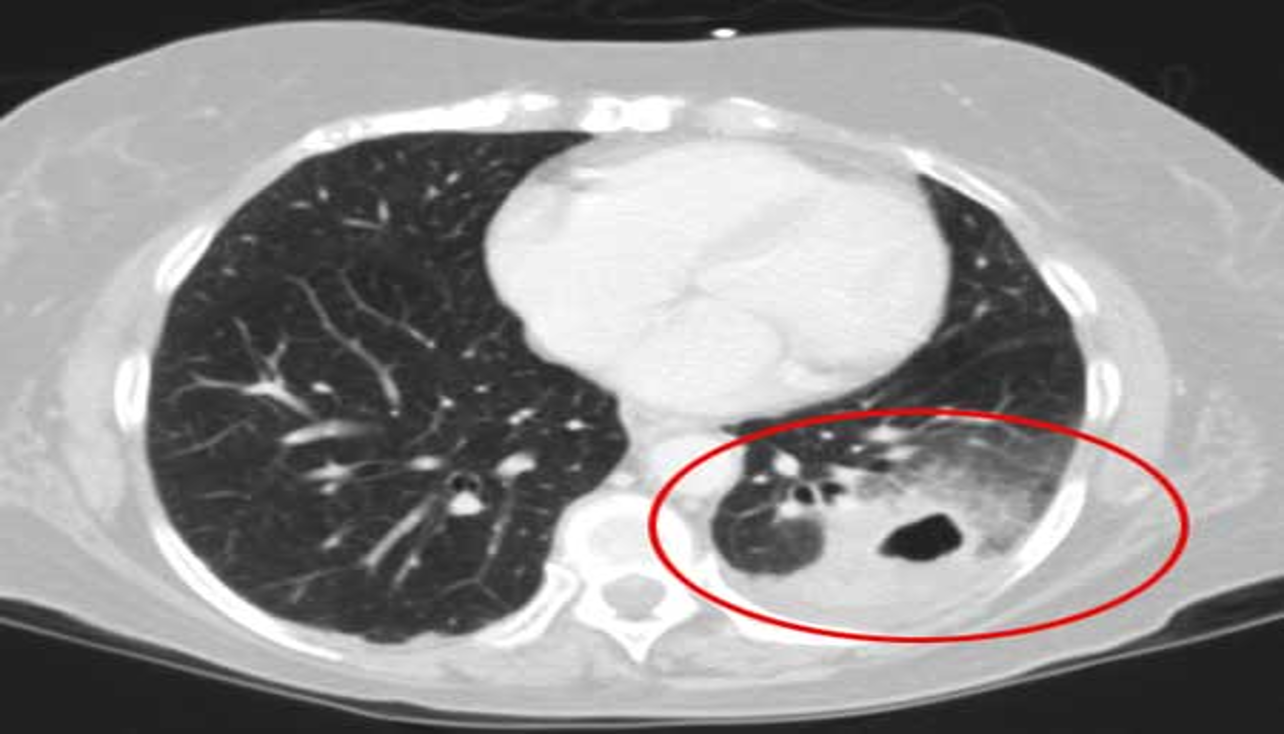
CT scan:
Provides more detailed imaging of suspected abscess or empyema.
DIFFERENTIAL DIAGNOSIS
Foreign body aspiration must be considered in young children. The aspiration event may not have been witnessed.
Other causes of tachypnea, with or without fever and cough, in infants and young children include:
- Bronchiolitis.
- Heart failure
- Sepsis
- Metabolic acidosis.
These conditions usually can be distinguished from pneumonia by history, examination, and laboratory tests or additional imaging may be necessary.
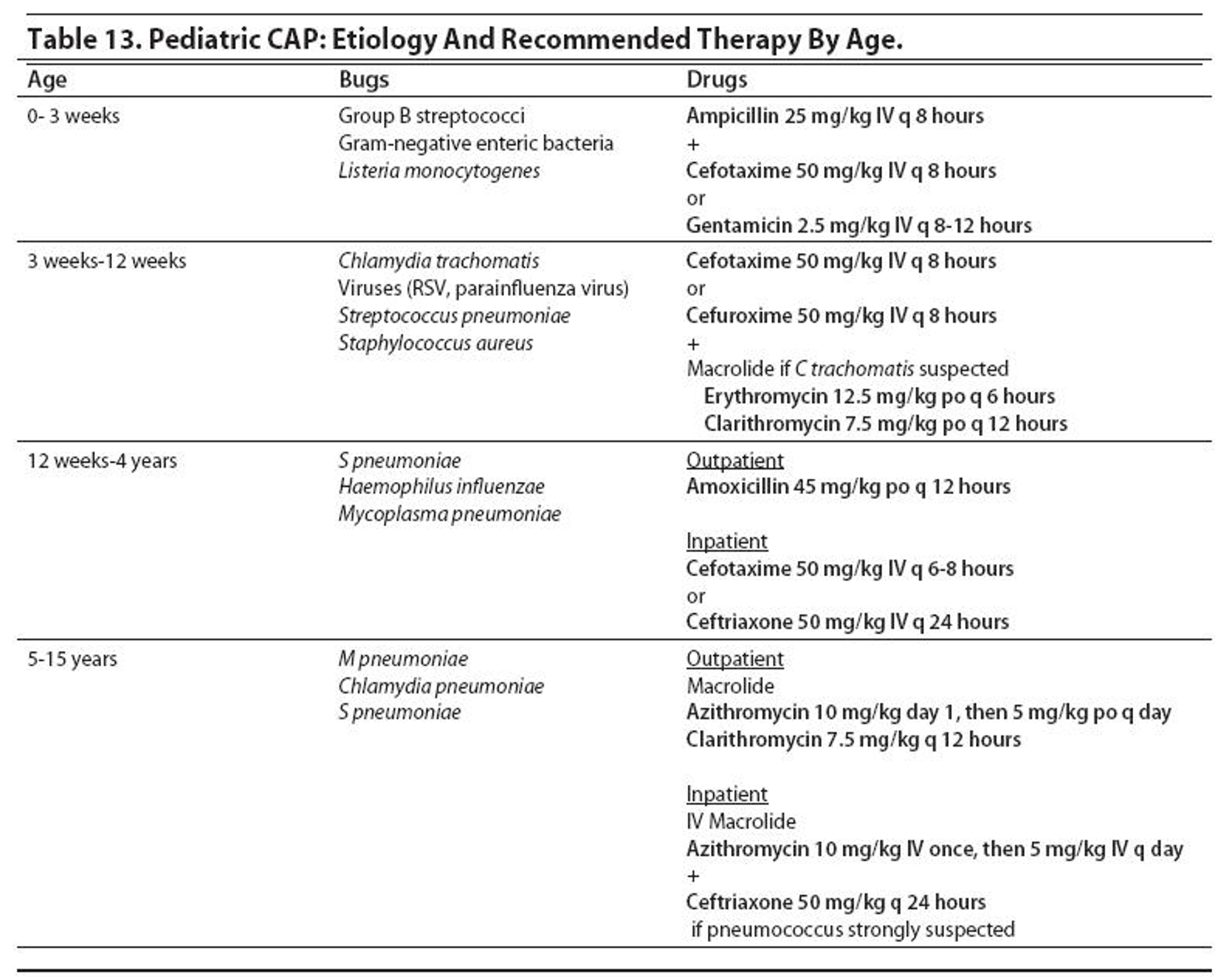
TREATMENT
As viral and bacterial pneumonia are often difficult to distinguish, treatment including the use of antibiotics is based on age and severity. Treatment may include:
- Oxygen: to maintain SaO2 >92%
- Fluids: restrict to 80% maintenance. (contrast to bronch)
- Antipyretics
- Antibiotics:
- Outpatient
- <5 years: amoxicillin is the first choice oral antibiotic, alternatives include co-amoxiclav and macrolides
-
5 years: a macrolide (erythromycin, clarithromycin, or azithromycin) is the first choice oral antibiotic as mycoplasma infection is more likely.
- Hospital
- Oral antibiotics are safe and effective for many children with CAP, but in severe cases with sepsis, consolidation with effusion, failed response, or intolerance to oral antibiotics, IV treatment is indicated with a third-generation cephalosporin (e.g., cefotaxime, ceftriaxone) or ampicillin.
- A change to oral antibiotics can then be made if there is clear improvement.
- Treatment duration is between 5 and 10 days depending on severity.
- Outpatient
if <3m or with high risk check oxygen saturation 92% indication.
COMPLICATION
Most children with CAP improve without complications, but an unexplained trend of increased complications of bacterial pneumonia has been seen worldwide.
- Treatment failure (antibiotic resistance)
- Lung Abscess.
- Metastatic infection.
- Pleural infection (Pleural Effusion or empyema).
- Pneumatoceles.
- Necrotizing pneumonia
- Hyponatremia secondary to inappropriate ADH secretion is common.
- Aspiration Pneumonia
Therapeutics Y
–It is acute inflammation of the lung parenchyma. –The cause may be infectious or non infectious.
Pneumonia affects 450 million/yr, 7% of population & result in 4 million deaths.
- Community Acquired Pneumonia (CAP)
Imaging
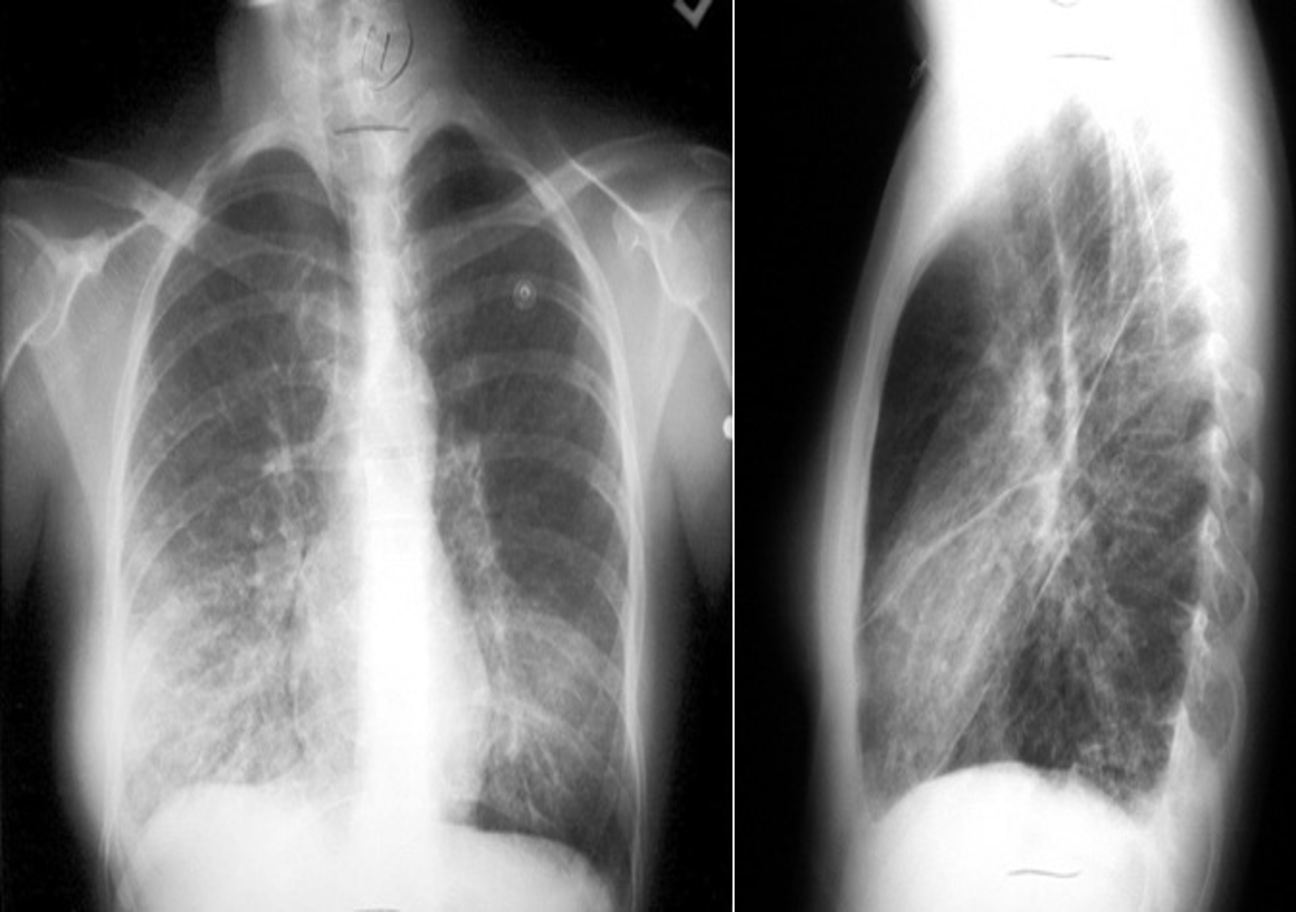
RT. lower lobe; Lobar pneumonia: Opacity of one or more pulmonary lobes & Presence of air bronchograms
- Right lower lobe is most commonly affected by pneumonia
- Spine blackness increased reversibly (Spine sign); lower part opaque

Bronchopneumonia:
- Poorly defined patchy infiltrates scattered throughout the lungs.
- Presence of air bronchograms
Air Bronchogram
Normally, it is not possible to identify air in bronchi within normally aerated lung, because the walls of the normal bronchi are too thin and air-filled bronchi are surrounded by air in the alveoli. However, if the alveoli are filled with fluid, the air in the bronchi contrasts with the fluid in the adjacent lung.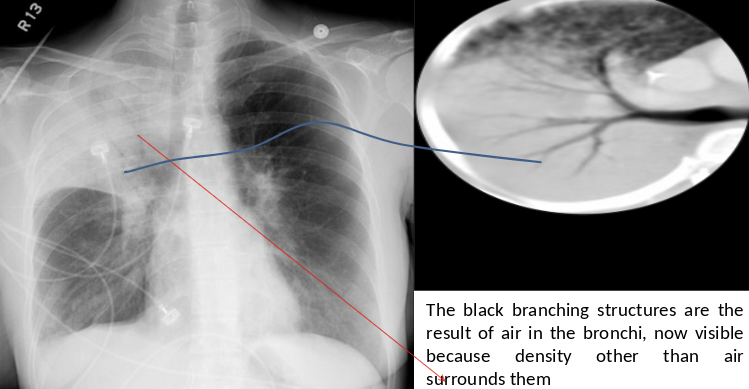
CT chest (axial plane; lung window) of a patient with a history of bacterial pneumonia
Opacification of much of the right lower lobe parenchyma is the result of air space consolidation. Pulmonary vessels are obscured and patent airways
(air bronchograms, white dashed line) are seen.