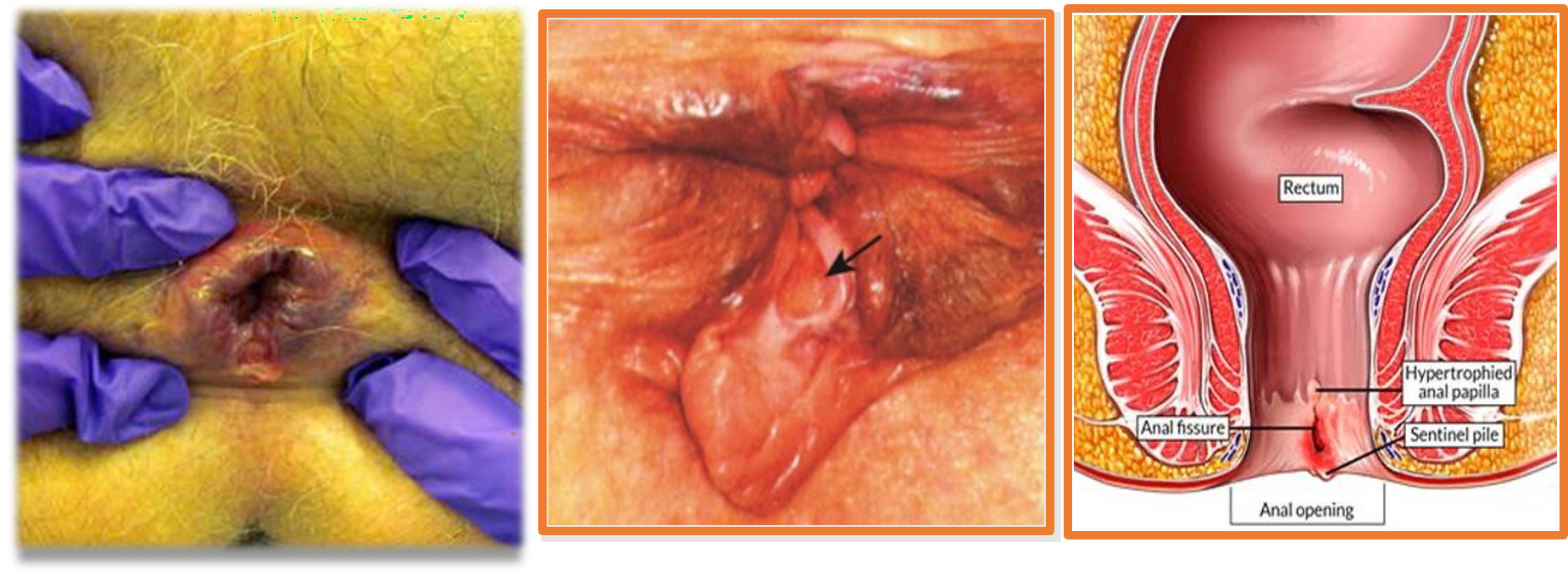
Anal Fissure
Painful linear tear or crack in the distal anal canal
- Acute vs chronic
- In short term: involves only the epithelium
- In long term: involves full thickness of the anal mucosa

The most commonly observed abnormalities:
- Hypertonicity, & hypertrophy of the internal anal sphincter
- Elevated anal canal
- Elevated internal sphincter resting pressures
- Relative ischemia, delayed healing, & healing by fibrosis
Pathophysiology and Etiology
Exact etiology is unknown
Risk factors are:
- Trauma from the passage of a particularly hard/ watery stool
- Low-fiber diets (lacking in fruits and vegetables)
- Prior anal surgery is a predisposing factor because scarring from the surgery may cause either stenosis or tethering of the anal canal, which makes it more susceptible to trauma from hard stool
Symptoms:
- Acute vs chronic
- Severe pain during defecation
- Lasts several minutes to hours afterward
- Recurrent
- Patient afraid or to have a bowel movement,
- Leading to a cycle of worsening constipation, harder stools, and more pain
- Bright blood on toilet paper, or stool
- Commonly, no significant bleeding.
Clinically:
-
Usually diagnostic
-
Location:
-
Midline ( Posterior- Anterior- Combined)
-
Off midline:
- Possibility of other bowel conditions (eg, Crohn disease),
- Infection (eg, sexually transmitted disease,or AIDS)
- Cancer.
-
Management:
Conservative:
- Modify life-style
- Food ( high fiber, low fat, avoid spicy)
- Sitz bath
- Avoid constipation/ diarrhea
Medical tharapy:
- Local analgesia (Lidocaine)
- Sphincter relaxation:
- Nitroglycerin 0.4% (NTG; also called glycerol trinitrate)
- Diltiazem 2%
- Botulinum toxin (eg, onabotulinumtoxina [BOTOX®]
Surgery:
- Lateral internal sphincterotomy
Indications:
- Failure of conservative therapy
- Symptomatic chronic fissure
Complications from surgery for anal fissure include the following:
- Infection
- Bleeding
- Fistula development
- Incontinence (the most feared complication)
- Recurrence/ nonhealing