IM
Hashimoto’s thyroiditis (chr. autoimmune thyroiditis)
- a) Autoimmune disease
- b) “Anti TPO antibodies” present
- c) Most cases are females
- d) Goiter present ( nodular)
- e) Patient may have other autoimmune diseases (vitiligo, DM, pernicious anemia, Addison’s)
SURGERY
Thyroiditis: Hashimoto’s disease
- Chronic autoimmune, destructive lymphocyte infiltration
- Commonest cause of hypothyroidism
- Females- >10 times
- 90 % - circulating anti-TPO (thyroid peroxidase)
- Initially euothyroid, later hypo- wt. gain, cold intolerance, constipation, dry skin, weakness
- Diffuse goitre/ may be nodular
- May change to lymphoma
Diagnosis: Low T4, increased TSH, anti TPO, FNA
Treatment: Thyroxine replacement Surgery- compressive symptoms, ? malignancy
ENT
Etiology
Due to auto Ab to thyroglobulin & microsome Ag-Ab reaction destruction of thyroid follicle.
Clinical Picture
- Manifestations of thyrotoxicosis in 5% of cases (in early stage)
- Manifestations of myxedema.
- Autoimmune manifestations e.g. erythema nodosum.
- Other autoimmune diseases e.g. vitiligo.
- The gland is asymmetrically large, firm, and nodular.
Complication
- Myxedema
- Pressure effects
- Lymphoma
Treatment
- Medical: Cortisone + L-thyroxin.
- Surgery: if large with pressure manifestations or suspicious of malignancy.
Imaging
is a common form of autoimmune thyroiditis and the leading cause of hypothyroidism.
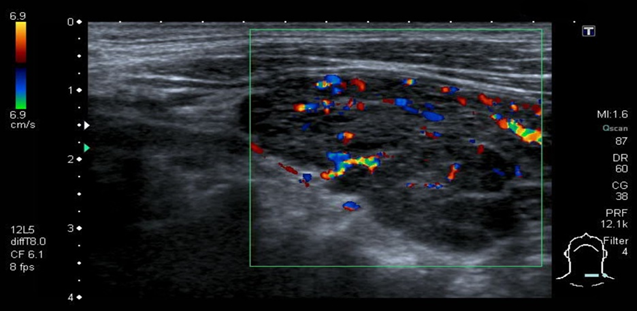
Ultrasound:
to assess thyroid size, echotexture, and to exclude thyroid nodules
Results depend on the form of Hashimoto thyroiditis.
- Atrophic phenotype: Reduction in thyroid size.
- Goitrous phenotype: Heterogeneous enlargement
Color-coded duplex sonography of the thyroid
There are hypoechoic and heterogeneous thyroid parenchyma and an enlarged thyroid.
There is no increased vascularization or perfusion in the color-coded duplex ultrasound. - These findings are consistent with the
Acute stage of Hashimoto thyroiditis.
Hashimoto thyroiditis
Thyroid ultrasound (transverse view): marked reduction in size and a heterogenous, flaky echoic structure suggesting inflammatory infiltration.
The thyroid is significantly hypoechoic and its appears lumpy compared to the surrounding muscles
