Growth and Short Stature
Dr Faten Zaidan
Definitions
- Length: stature of supine child (< 2 years old)
- Height: stature of standing child (>2 years old)
- Short stature: length or height below 3rd percentile
- Tall stature: length or height above 97th percentile
- Underweight: weight below 3rd percentile
- Overweight: weight between 110-120% of expected median percentile of the reference population
- Obesity: weight more than 120% of expected median percentile of reference population. Expressed as BMI
- Growth velocity: annual linear growth rate
- Bone age: Reflects bone maturation: the time at which long and short bone ossificates (chondrocyte in the cartilaginous growth plate proliferate -linear bone growth- and transforms to osteoblasts to form a bone -ossification)
Head Circumference
Brain growth is most rapid during the first two years of life.
-
HC increase 10 cm in first year:
- 1-3 months: 2cm/month
- 4-6 months: 1cm/month
- 6-12 months: 0.5cm/month
-
2-3 cm in the 2nd year
-
5-6 cm throughout the remainder of childhood
Length <2yrs / Height >2 yrs or standing
- Birth length increases 50% by 1 year
- Birth Length doubles by 4 years of age
- Birth length triples by 13 years of age
- After 2 years of age, average height increases 5 cm/year until adolescent
Weight
- Birth weight is regained by 10-14 days of life
- Birth weight doubles by 4 months of age
- Triples by 12 months of age
- Quadruples by 2 years of age
- After 2 years of age, normal weight gain is 2.5 kg per year until adolescent
Presentations
History
- Onset
- Previous measurements of both weight and height, calculate growth velocity
- Evidence of chronic disease
- Evidence of endocrinopathies
- Birth weight and mode of delivery
- Family history of:
- Short stature
- Family disease
- Social deprivation
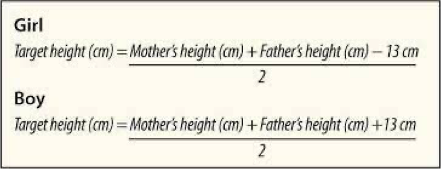
- Parents’ height (to calculate midparental height)
- Midparental height is used to determine the expected height the child must reach
Physical Examination
Examination:
-
Accurate measurements (do it yourself, 2 persons are needed to measure length).
-
Evidence of chronic illness e.g, joint deformity, dysmorphism, etc.
-
Endocrinopathy: e.g, goiter, midline defects, etc.
-
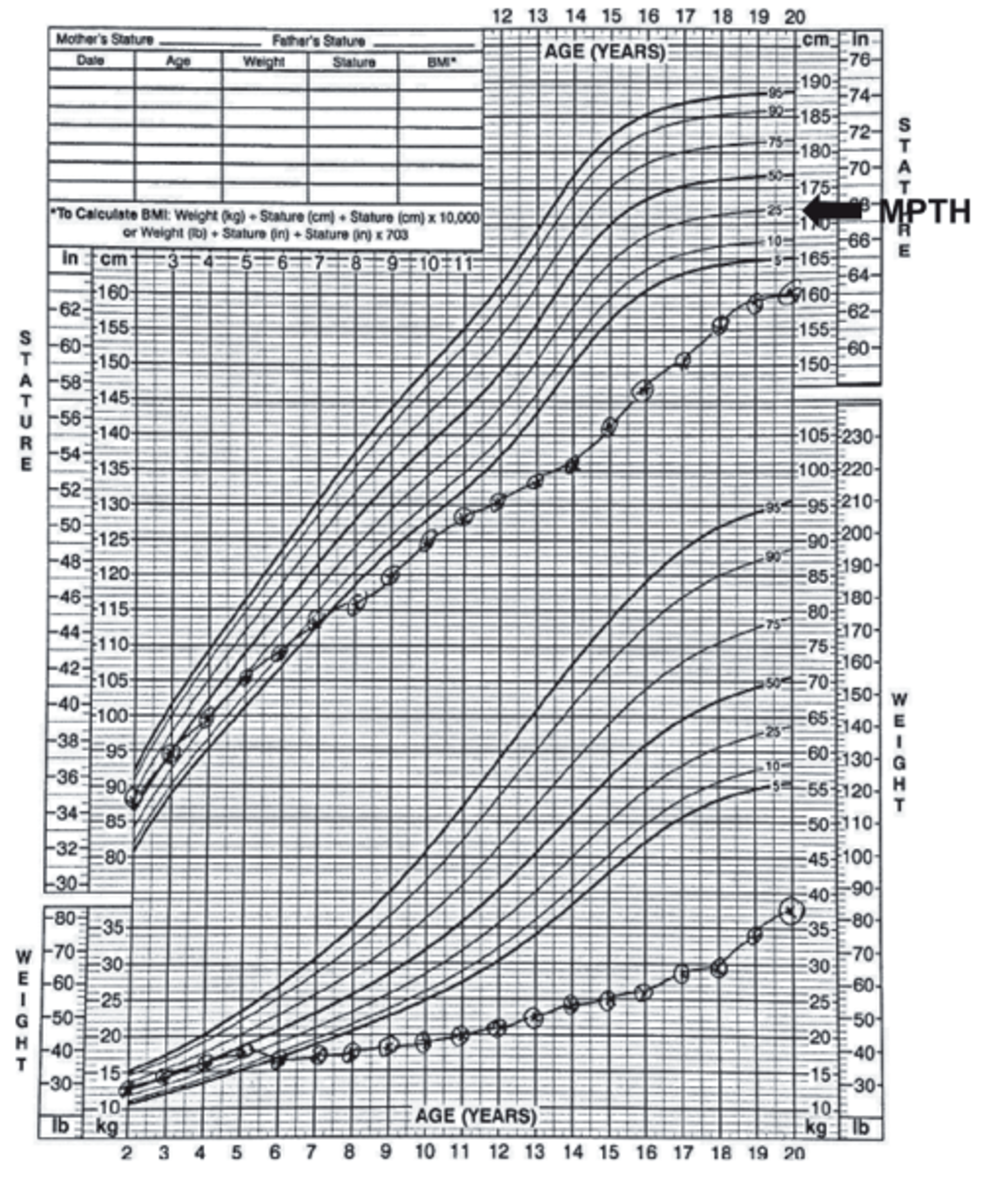
Correct plotting: Be familiar with growth charts and know how to use them.
-
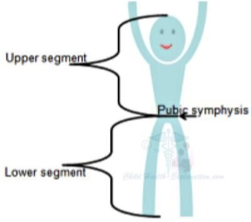
Assess proportionism by:
- Measuring upper to lower segment (1.7:1 in newborns and almost 1:1 in adults).
- Arm span: This is usually equal to the height ± 5 cm.
-
Fundoscopy: for optic atrophy.
-
Goiter.
-
Teeth.
-
ENT: look for midline defect.
-
Systems: look for evidence of chronic illness.
-
Assess puberty as per Tanner staging.
Upper/Lower Ratio
- Upper to lower segment ratio is measured for short stature cases to see if the upper segment of the body is proportionate or disproportionate to the lower segment of the body.
- At birth, Ratio is 1.7:1
- Trunk is longer than legs
- At 1 year old, Ratio is 1.4:1
- At 10 years old, Ratio is 1:1
- Trunk is equal to legs
- When do we see the upper segment is larger than the lower segment:
- Rickets, Turner, Achondroplasia
- When do we see the upper segment is smaller than the lower segment:
- Marfan Syndrome
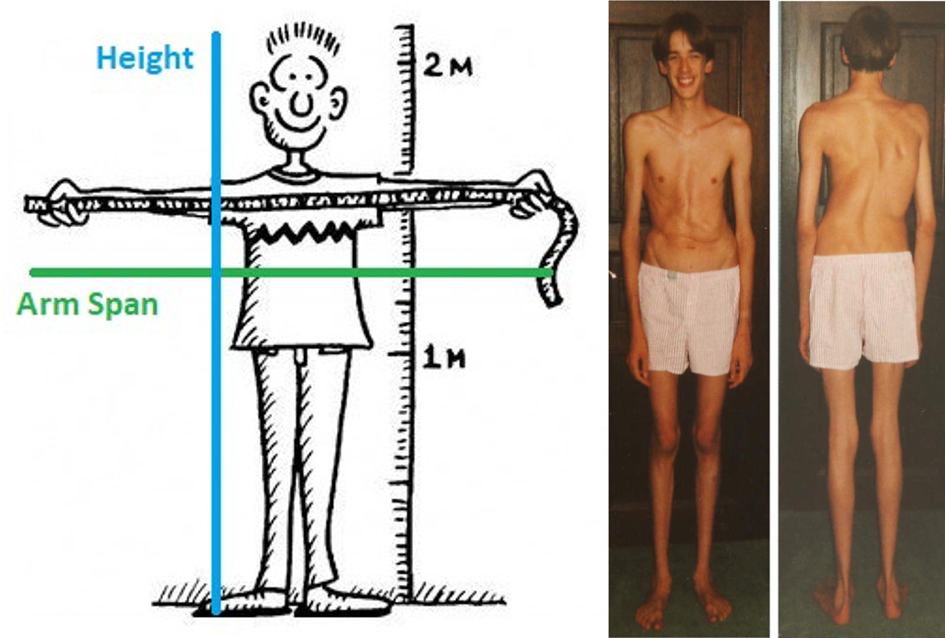
Arm Span
- Arm Span (AS): distance between the tips of the fingers when the patient holds both arms outstretched horizontally while standing against a solid surface
- At birth, AS is less than length by about 2.5 cm.
- By 10 years of age, AS is equal to height
- After 10 years in boys and 12 years in girls, AS exceeds height by up to 5 cm.
- If AS is exceeding height by more than 5 cm, consider pathologic causes of tall stature such as Marfan Syndrome
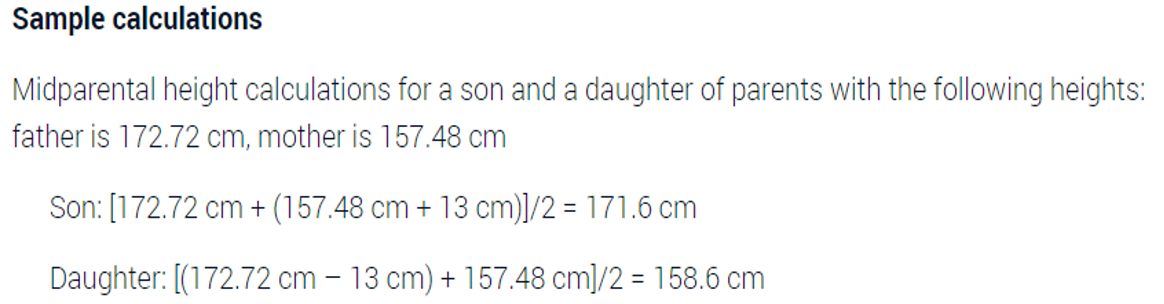
Mid-Parental Height
- Normally should be +/- 10 cm
Investigations
| TEST | RATIONALE |
|---|---|
| CBC | Anemia: nutritional, chronic disease, malignancy |
| Leukopenia: bone marrow failure syndromes | |
| Thrombocytopenia: malignancy, infection | |
| ESR, CRP | Inflammation of infection, inflammatory diseases, malignancy |
| Metabolic panel (electrolytes, liver enzymes, BUN) | Signs of acute or chronic hepatic, renal, adrenal dysfunction; hydration and acid-base status |
| Carotene, folate, and prothrombin time; celiac antibody panel | Assess malabsorption; detect celiac disease |
| Urinalysis with pH | Signs of renal dysfunction, hydration, water and salt homeostasis; renal tubular acidosis |
| Karyotype | Determines Turner (XO) or other syndromes |
| Cranial imaging (MRI) | Assesses hypothalamic-pituitary tumors (craniopharyngioma, glioma, germinoma) or congenital midline defects |
| Bone age | Compare with height age and evaluate height potential |
| IGF-1, IGF-BP3 | Reflects growth hormone status or nutrition |
| Free thyroxine | Detects MPHD or isolated hypothyroidism |
| Prolactin | Elevated in hypothalamic dysfunction or destruction, suppressed in pituitary disease |
Growth Hormone Therapy
-
Eight indications for Growth hormone therapy as per FDA:
- Noonan Syndrome
- GH deficiency
- Turner syndrome
- Chronic renal failure
- Idiopathic short stature
- SGA
- Prader Willi Syndrome
- SHOX gene abnormality
-
Criteria for discontinuing GH treatment:
- Decision by the patient/parent to discontinue.
- Growth rate less than 2 cm/year.
- Bone age of 14 years in girls and 16 years in boys.
-
Adverse effects of GH: Z
Special Growth Chart of Turner Syndrome
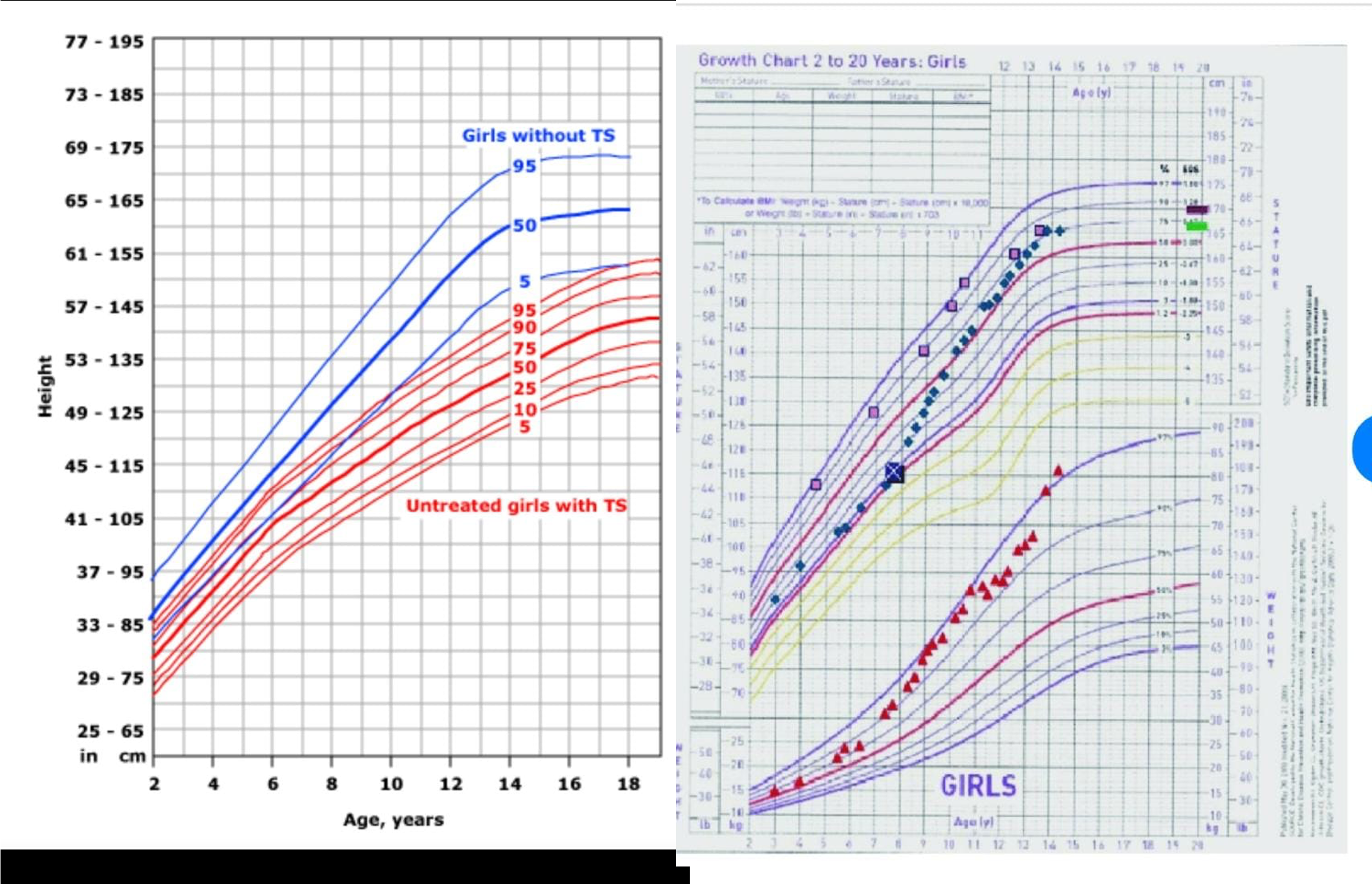
Turner growth chart with missed growth deceleration for several years prior to diagnosis and then post-treatment with growth hormone and then with estradiol added resulting in final height near mid-parental expectations.
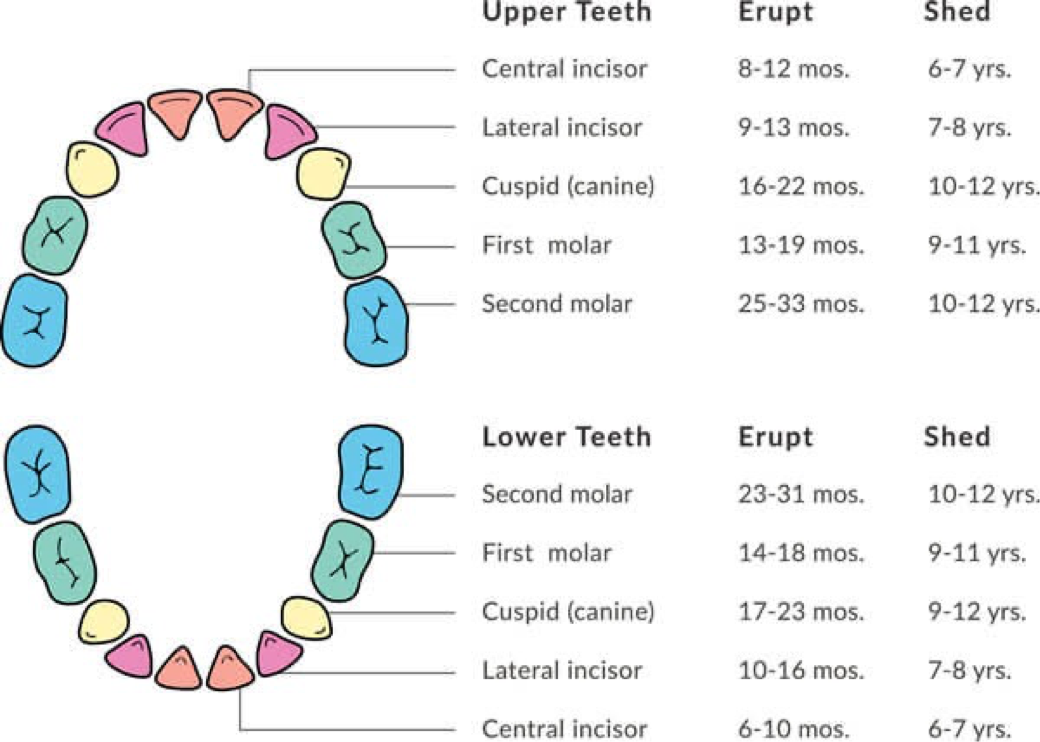
Teething
- Eruption of Deciduous dentition primary/Baby Teeth starts at age of 6-8 months
- By age of three years, all teeth should be erupted
- Total number of primary teeth is 20 teeth
- Permanent (Secondary teeth) starts at age of 6 years.
-
Total number of permanent teeth is 32 teeth
-
Symptoms:
-
LOW GRADE fever
-
Irritability
-
Drooling
-
Gum rubbing and increased biting
-
Ear rubbing
-
Decreased appetite MILDLY
-
- Myths:
- Diarrhea, Sleep disturbance, vomiting, cough, fever above 38 C are symptoms of teeth eruption. These symptoms are abnormal and need doctor’s evaluation.
Teeth Brushing
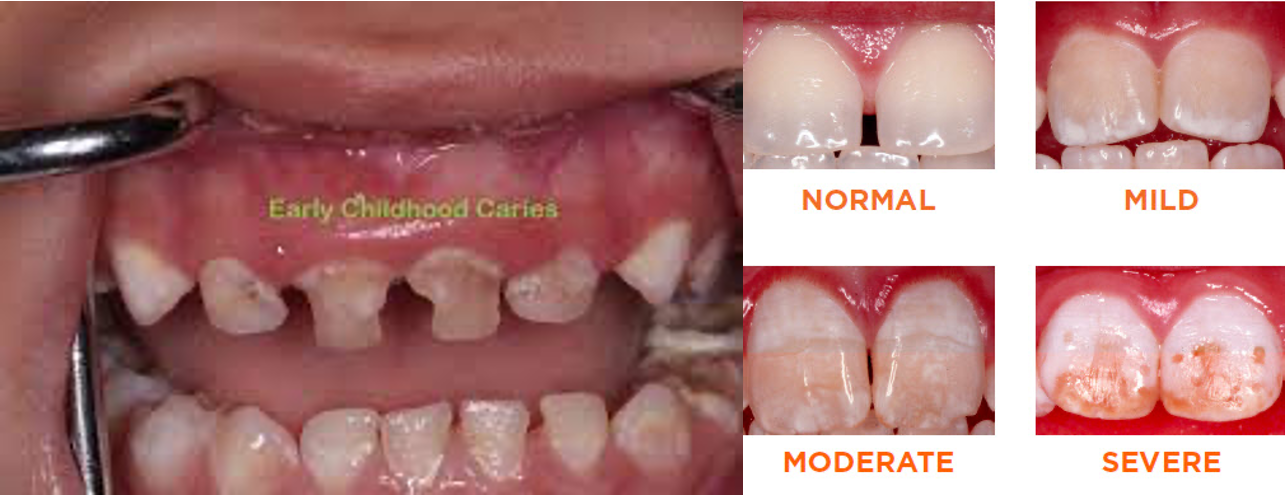
Brushing should start when the first tooth starts to erupt TO PREVENT EARLY DENTAL CARIES. Children with morbidities, intellectual disabilities, and special needs are the most prone to poor oral hygiene and dental caries.
- Toothpaste should contain fluoride because it strengthens dental enamel, protects dental enamel due to its resistance to chemical and physical damage, and protects against osteoporosis later in life.
Excess fluoride will result in fluorosis: Brown and white spots on teeth. Therefore:
- Infants should not receive fluoride supplements before 6 months of age.
- Toothpastes should be chosen based on the amount of fluoride it contains (most companies produce toothpaste with little fluoride).
- The fluoride content of human milk is low and is not influenced significantly by maternal intake.
What is the Amount of Toothpaste Allowed?

Delayed Teething
Delayed teething is defined as eruption after age of 15-18 months Causes:
-
Exclusively breastfed baby who is not supplemented with Vitamin D - Poor infant’s sun exposure
-
Endocrinopathies (Hypothyroidism, Hypopituitarism)
-
Genetic (Down Syndrome, PERT Syndrome, Achondroplasia)
-
Poor socioeconomic status
-
Poor maternal sun exposure during pregnancy
appears first lower incisors then upper
down up up down