Pediatric
Dr. Mansour Alqurashi
Learning Objectives
- Understand common definitions in neurology: seizures, epilepsy, status epilepticus, aura, ictal and postictal phases.
- Discuss and categorize the various etiologies of seizures in infancy and childhood.
- Describe the different types of seizure disorders in children.
- Discuss the clinical presentation of various epileptic syndromes in pediatrics.
- List the diagnostic criteria for the establishment of febrile seizure.
- Describe the general management and prognosis of febrile seizures.
Other Presentations
Epilepsy
Definitions
Seizure
A sudden, involuntary, time-limited alteration in behavior, motor activity, autonomic function, consciousness, or sensation, accompanied by an abnormal electrical discharge in the brain due to abnormal neuronal activity and sudden biochemical imbalance at the cell membrane.
Acute Symptomatic (Provoked) Seizure
A seizure occurring in the setting of some systemic provoking factor (normal brain).
Unprovoked Seizure
Occurs in the absence of a potentially responsible clinical condition or occurs in relation to a preexisting brain lesion or progressive nervous system disorder beyond the time interval recognized for acute symptomatic seizure.
Provoked Seizures
Common Causes
- Febrile seizures
- Metabolic events (e.g., hypoglycemia)
- Acute CNS infections
- Drug intoxication
- Head trauma
Other Causes
- Post-infectious or post-vaccinal encephalopathy
- Inborn errors of metabolism
Incidence/Prevalence
- 0.5-1%
Clinical Presentation
Motor Changes
Parents/caregivers may report seeing:
- Repetitive non-purposeful movements
- Staring
- Lip-smacking
- Falling down without cause
- Stiffening of any or all extremities
- Rhythmic shaking of any or all extremities
Seizure activity cannot be interrupted with verbal or physical stimulation.
Sensory and Autonomic
Parents/caregivers may report the child is:
- Feeling nauseated
- Feeling odd or peculiar
- Losing control of bowel or bladder
- Feeling numbness, tingling
- Experiencing odd smells or sounds
Consciousness
Consciousness is the usual alertness or responsiveness. Parents or you may observe the child to have:
- Baseline alertness
- Diminished level of consciousness
- Unresponsive and unconscious
Events That Mimic Seizures
- Apnea
- Breath Holding spells
- Dizziness
- Myoclonus
- Psychogenic Seizures/Pseudo seizures
- Benign neonatal sleep myoclonus
- Night terror (2–3 hours after a child falls asleep, non-REM)
- Rigors
- Shuddering attacks
- Jitteriness
- Syncope
- Tics
- Dystonia
- Transient Ischemic Attacks
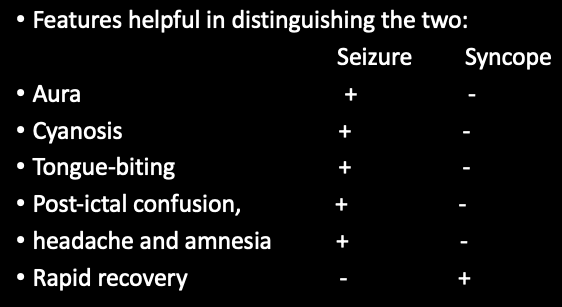
Epilepsy vs. Syncope
| Feature | Epilepsy | Syncope |
|---|---|---|
| Precipitating factors | Rare | Common |
| Occurrence | Awake, sleep | Awake |
| Onset | Abrupt | Gradual |
| Duration | 60-90 sec | 10-15 sec |
| Jerking limbs | Yes | Occasional |
| Facial colour | Flushed | Pale |
| Perspiration | Hot, sweaty | Cold, clammy |
| Postictal recovery | Slow | Rapid |
| Postictal confusion | Common | Uncommon |
| EEG & prolactin | Positive | Negative |
Helpful Tools for Diagnosis
- Accurate history and description of events
- Ask family member to “act out” event
- Ask family to videotape event
- Provoking factors (Medications, genetic factors, electrolyte abnormalities, sleep state, infections, brain inflammation, or injury).
- EEG/VEEG (photic stimulation & hyperventilation, sleep deprivation)
Seizure Classifications
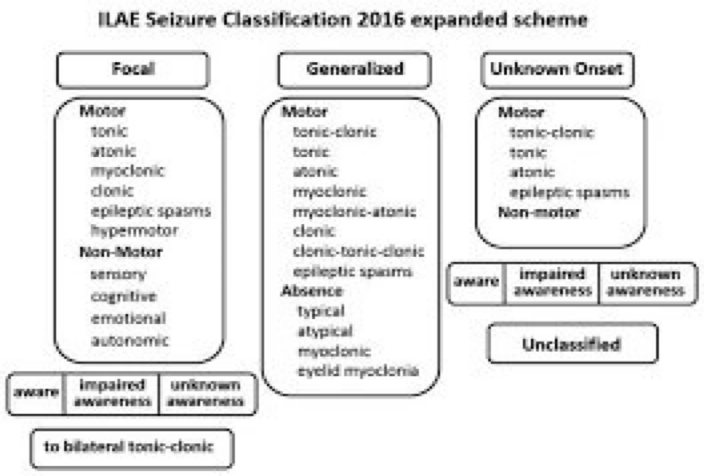
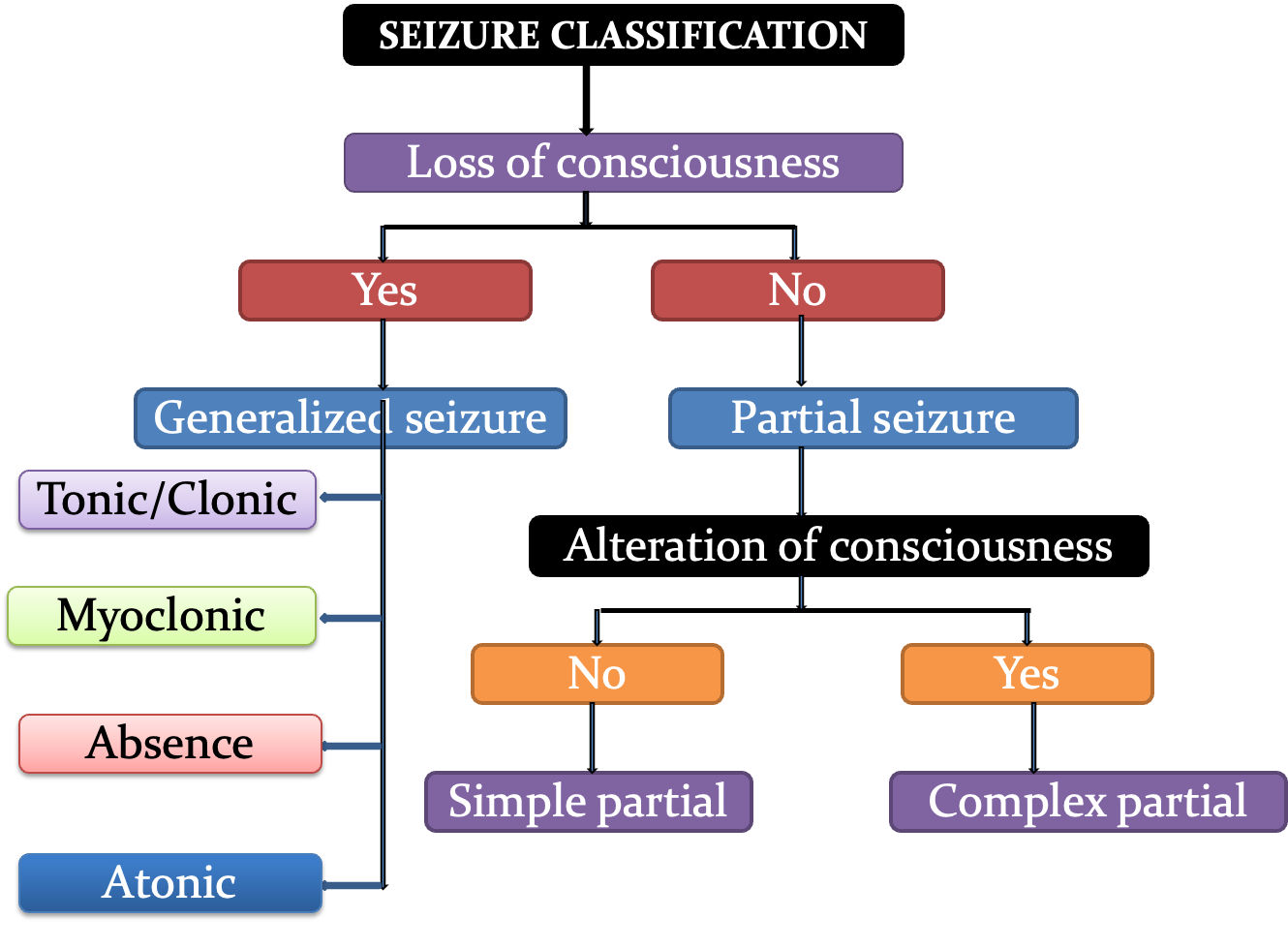
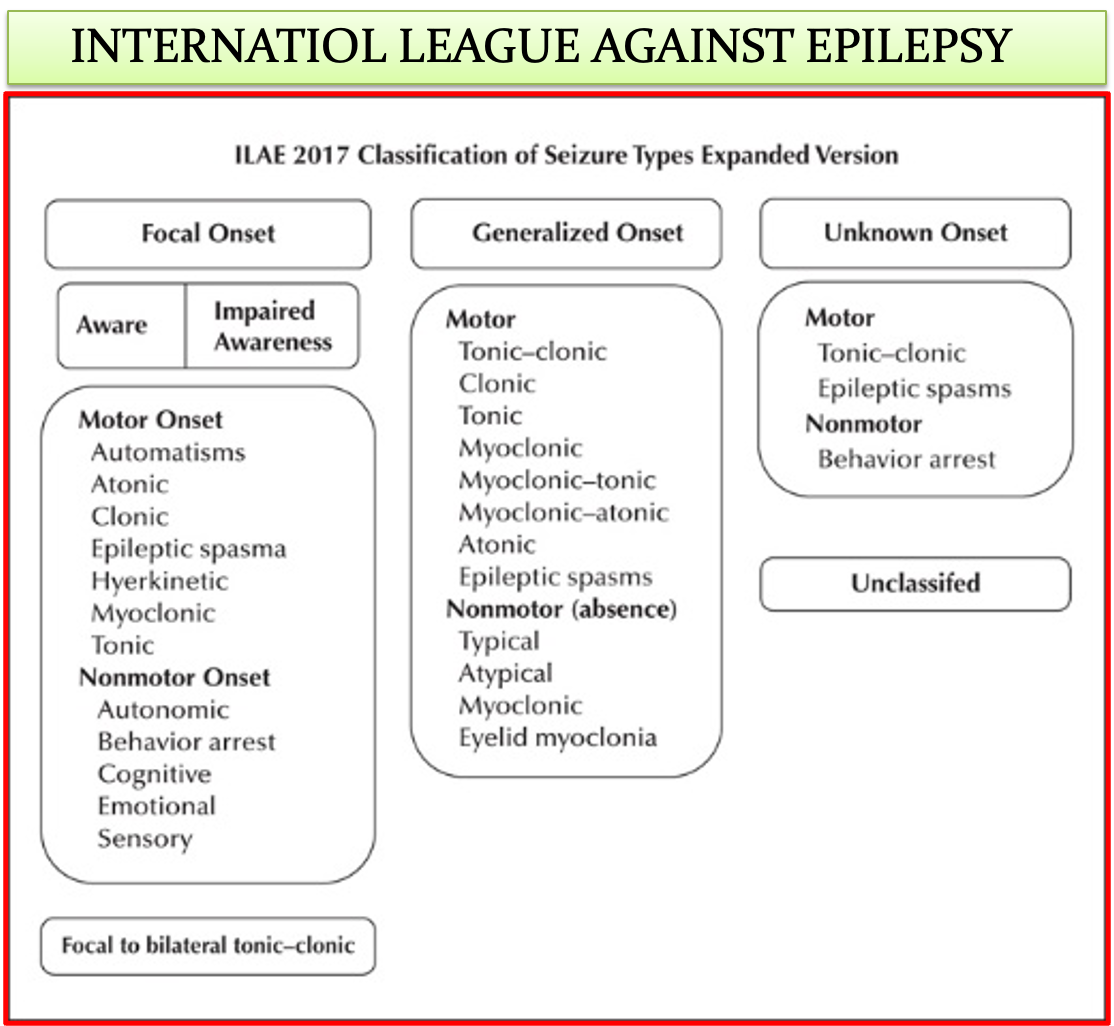
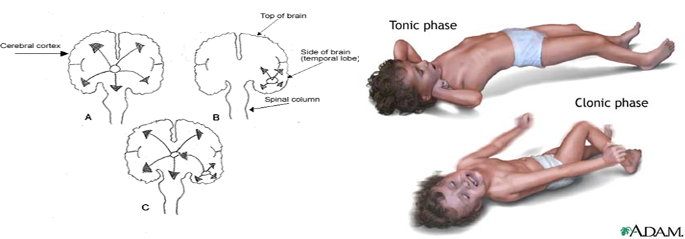
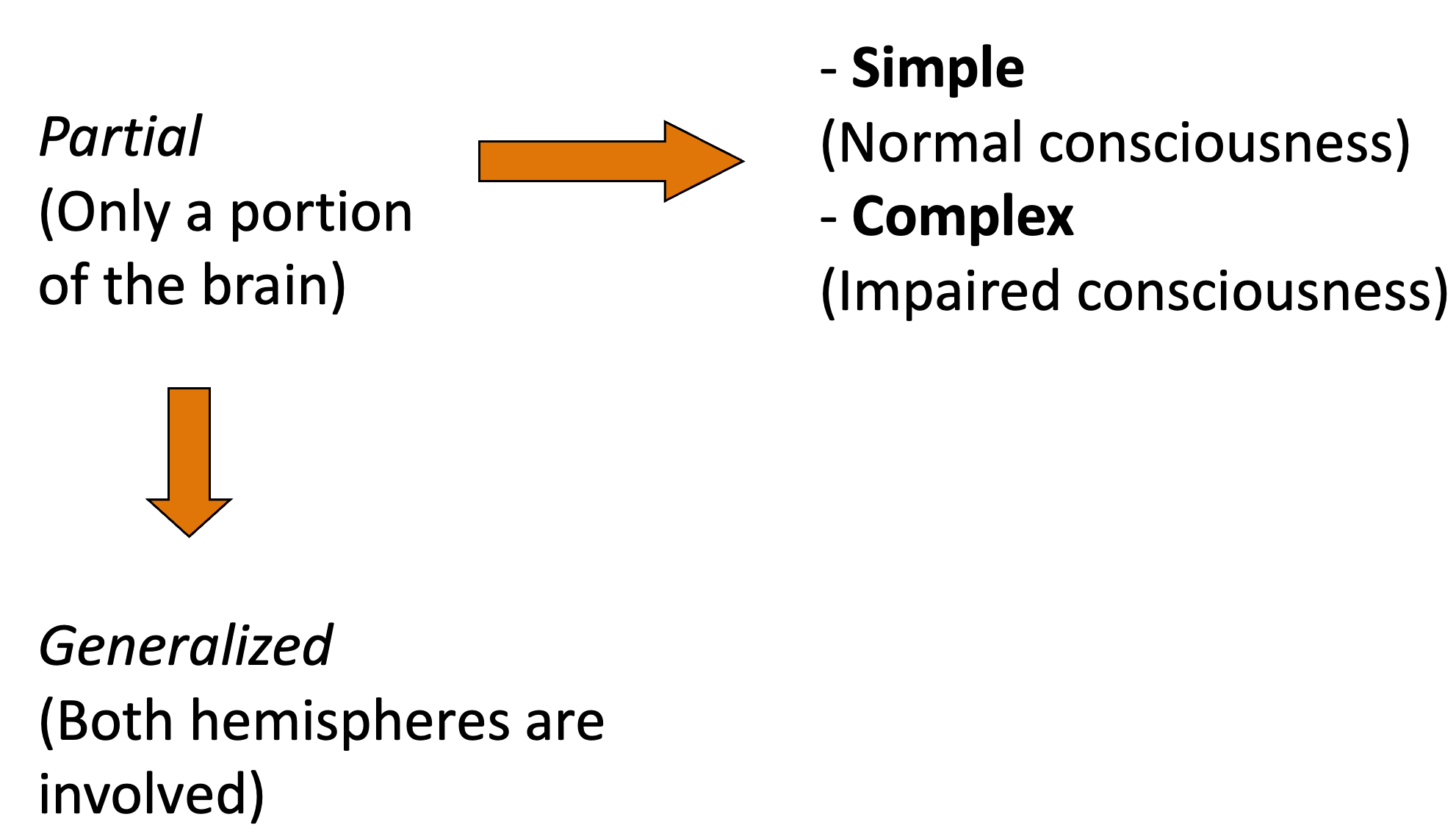 Seizures are classified with respect to where the abnormal neuronal activity occurs. With generalized seizures, both hemispheres of the brain are involved and there is loss of consciousness. Movements are tonic or clonic or a combination. Absence seizures are also generalized. Partial seizures may be simple or complex, and involve only one hemisphere of the brain. In complex partial seizures, there is altered level of consciousness, while in simple partial seizures there is NO loss of consciousness; however, there may be transient cognitive impairments. Movements begin with a single muscle group and then spread in both complex and simple partial seizures. The different types of symptoms that may occur include motor symptoms such as - head/eye deviation, jerking, stiffening; autonomic symptoms, such as - pupillary dilatation, drooling, pallor, change in heart rate or respiratory rate, as well as somatosensory symptoms, such as smells and/or alteration of perception (for example déjà vu).
Seizures are classified with respect to where the abnormal neuronal activity occurs. With generalized seizures, both hemispheres of the brain are involved and there is loss of consciousness. Movements are tonic or clonic or a combination. Absence seizures are also generalized. Partial seizures may be simple or complex, and involve only one hemisphere of the brain. In complex partial seizures, there is altered level of consciousness, while in simple partial seizures there is NO loss of consciousness; however, there may be transient cognitive impairments. Movements begin with a single muscle group and then spread in both complex and simple partial seizures. The different types of symptoms that may occur include motor symptoms such as - head/eye deviation, jerking, stiffening; autonomic symptoms, such as - pupillary dilatation, drooling, pallor, change in heart rate or respiratory rate, as well as somatosensory symptoms, such as smells and/or alteration of perception (for example déjà vu).
-
Epilepsy Auras
-
Absence Seizure
-
Status Epilepticus
-
Febrile Seizure
-
Rolandic Epilepsy
-
Infantile Epileptic Spasms Syndrome (IESS)
-
Juvenile Myoclonic Epilepsy (JME)
-
Lennox-Gastaut Syndrome
.
Treatment of a Newly Diagnosed Case of Epilepsy
- Seizure Therapy:
- 1st Monotherapy
- 2nd Monotherapy/Combination Therapy
- Ketogenic Diet
- Intractable Epilepsy:
- Combination Therapy, Vagus Nerve Stimulation (VNS)
- Surgery
CM
- Status epilepticus >15m
HISTORY OF SEIZURES
- Any clinical event caused by abnormal electrical discharge in the brain –
- Role of inhibitory neurotransmitter, gamma amino butyric acid (GABA) and various excitatory neurotransmitters (acetylcholine, amino acids such as glutamate and aspartate)
- Epilepsy is the tendency to have recurrent seizures (fits)
SEIZURE CLASSIFICATION
Depending on the source of the seizure within the brain:
Localized – Partial - seizures
- Simple partial - if consciousness not affected
- Complex partial - if consciousness is affected
Generalized seizures
- All involve loss of consciousness
- Further divided according to the effect on the body -include absence, myoclonic, clonic, tonic, tonic–clonic, and atonic seizures.
- Partial seizure may spread within the brain. This is known as secondary generalization
HISTORY OF SEIZURES
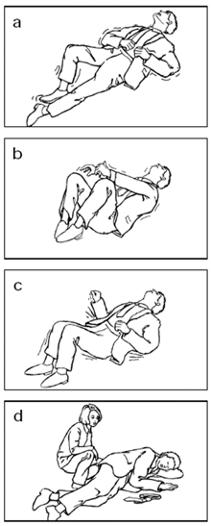
- Obtain a description of the seizure/s:
- From patient and witness (NB blackouts, faints, fits, loss of consciousness)
- What happens at the onset of the fit?
- What happens during the fit?
- Does the patient fall or remain standing or sitting?
- How does the fit end?
- Confusion or other post-ictal symptoms?
- Is there incontinence, any injury or tongue biting?
- Change in seizure pattern
- Frequency of seizures?
- When do the seizures occur?
- Head trauma or brain illness (especially in adult onset epilepsy)
- Birth history (especially in early onset seizures)
- Family history of seizures
- What medication is taken?
- History of past/ current medication, compliance and response to medication
SEIZURE AND SYNCOPE