Table of Contents
Postpartum Hemorrhage
By Dr. Mona Ahmed
Importance of PPH
Obstetric haemorrhage remains one of the major causes of maternal death in both developed and developing countries
Major causes of MM
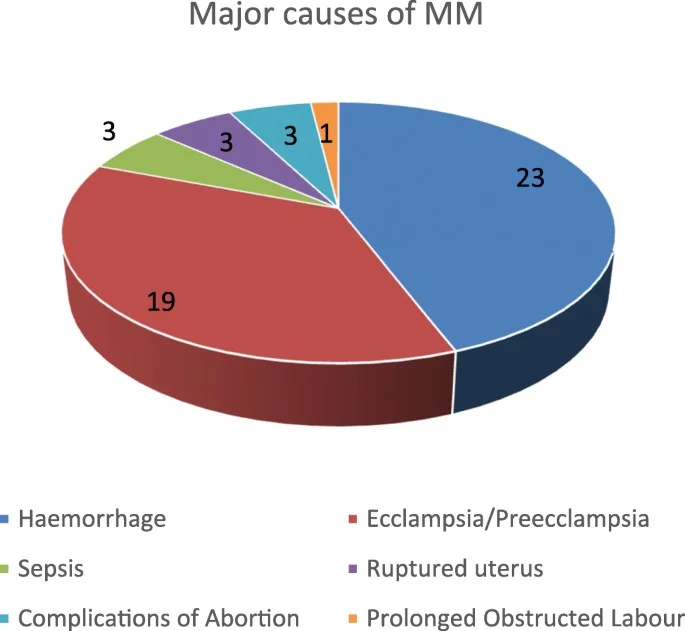
Postpartum Haemorrhage
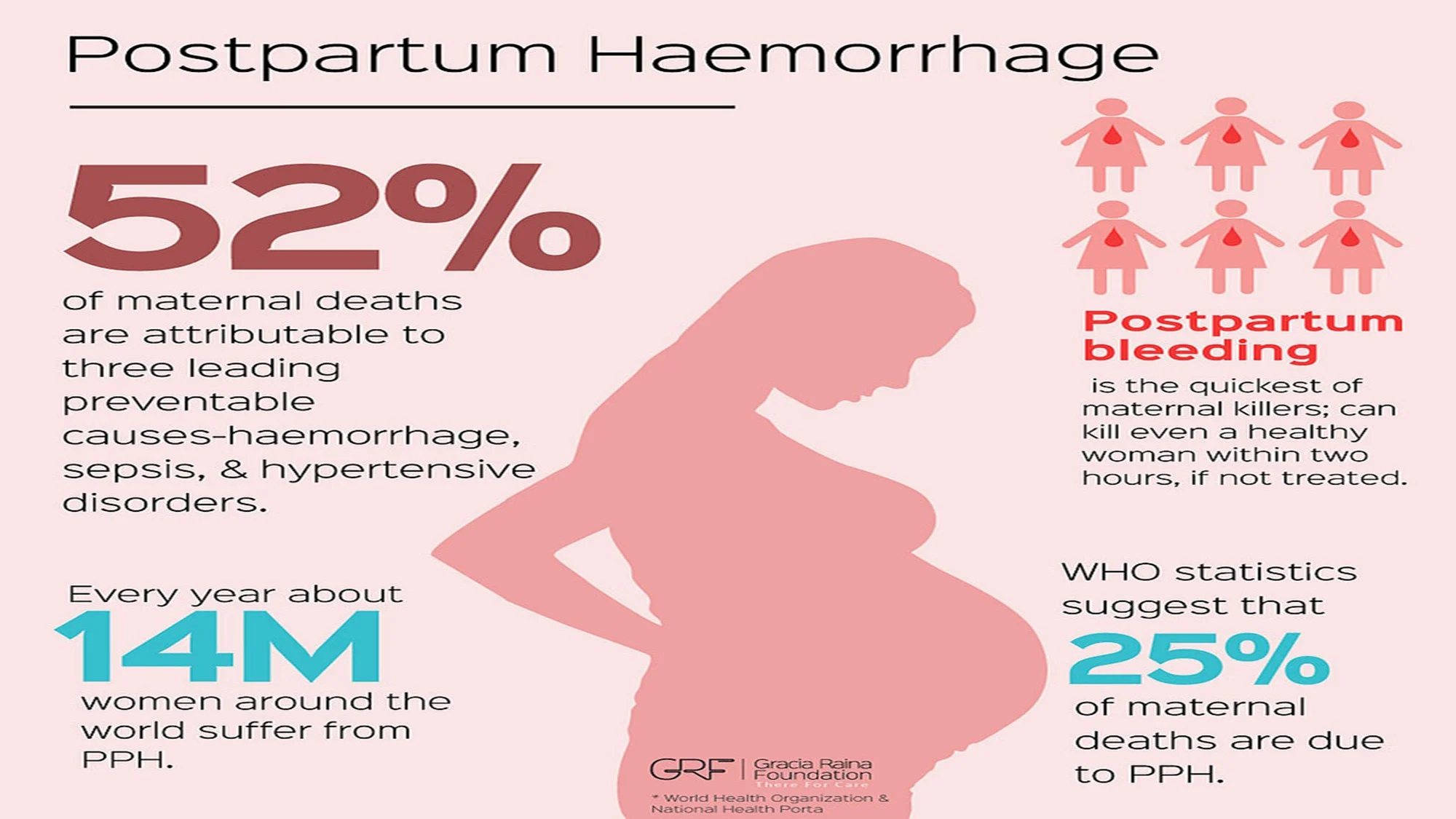
Global Impact

MMR due to PPH
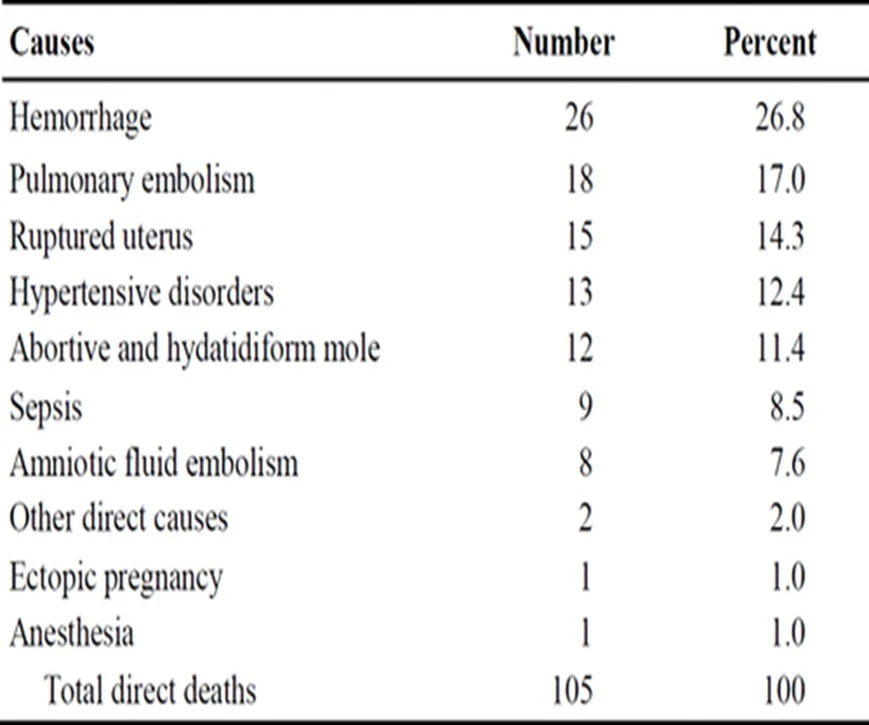
| Causes | Number | Percent |
|---|---|---|
| Hemorrhage | 26 | 26.8 |
| Pulmonary embolism | 18 | 17.0 |
| Ruptured uterus | 15 | 14.3 |
| Hypertensive disorders | 13 | 12.4 |
| Abortive and hydatidiform mole | 12 | 11.4 |
| Sepsis | 9 | 8.5 |
| Amniotic fluid embolism | 8 | 7.6 |
| Other direct causes | 2 | 2.0 |
| Ectopic pregnancy | 1 | 1.0 |
| Anesthesia | 1 | 1.0 |
| Total direct deaths | 105 | 100 |
US Pregnancy-Related Mortality
Definition of PPH
Primary post partum haemorrhage
500 ml blood loss from genital tract in the first 24 hours after birth.
Secondary post partum haemorrhage
Excessive or abnormal bleeding from genital tract between 24 hours & 6 weeks.
Causes of Postpartum Hemorrhage
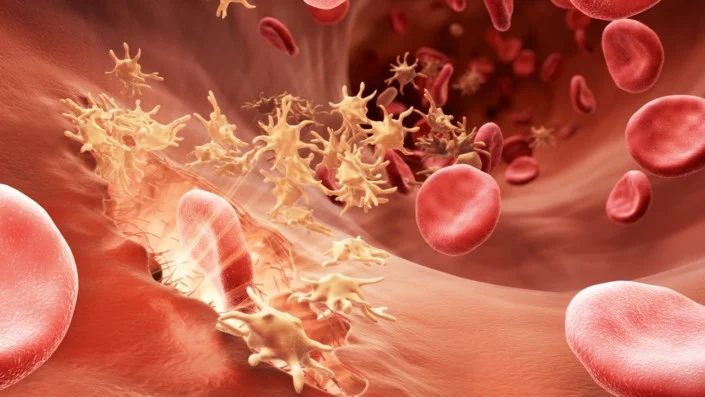
4T’s
- Tissue (retained placenta)
- Tone (uterine atony)
- Traumatic delivery
- Thrombin (coagulation disorders)
![]()
Four T’s Mnemonic for the Specific Causes of Postpartum Haemorrhage
| PATHOLOGY | SPECIFIC CAUSE | APPROXIMATE INCIDENCE (%) |
|---|---|---|
| Tone | Atonic uterus | 70 |
| Trauma | Lacerations Hematomas. Inversion. Rupture | 20 |
| Tissue | Retained tissue. Invasive placenta | 10 |
| Thrombin | Coagulopathies | 1 |
Prevention
Optimize haemoglobin levels below normal should be investigated & optimize prior to delivery. Management of 3rd stage of labour:
- prophylactic uterotonic(Oxytocin).
- Early cord clamping.
- Controlled cord traction to the placenta.

How to prevent lacerations?
- Routine episiotomy should be avoided to decrease blood loss and the risk of anal laceration
Causes of Uterine Atony
commonest causes of haemorrhage:
- uterine rupture.
- Uterine inversion
- Macrosomia.
- Multiple pregnancy.
- oxytocin use.
- grand multiparity.
- Polyhydramnios.
- Antepartum haemorrhage(Placental Abruption).
- Full bladder.
- Anaesthesia.
overdistention
TONE - UTERINE ATONY
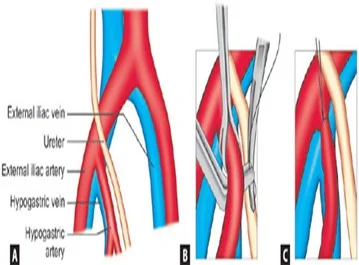
TISSUE - RETAINED PLACENTA
TRAUMA - LACERATIONS
TTHROMBIN - COAGULATION
Diagnosis of PPH
-
Detailed history including
- Parity.
- Mode of delivery.
- Third stage and puerperal complications.
-
Examination:
- Check pulse.
- Blood pressure.
- Temperature.
- Assess uterine size & cervical excitation and uterine tenderness Assessment.
- Exclude other sources of infection (e.g. mastitis, UTI or DVT).
- Assess clinical signs of blood loss.
- Speculum examination : Cervical dilatation, tears, infection, blood or remnant of tissues


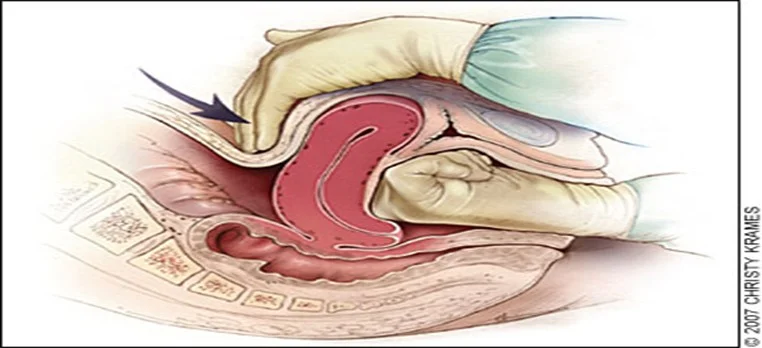
Diagnosis of Uterine Atony
- The main signs of uterine atony are:
- Bleeding.
- Enlarged and soft uterus in (bimanual examination)
- commonly referred to as “boggy.”
Management of Postpartum Haemorrhage
Resuscitate women. Stop bleeding.
Steps:
- Call for help
- Iv line(fluids , oxytocin).
- Obtain blood sample for:
- FBC.
- Clotting factors.
- U & E.
- Crossmatching of 6 unites.
- Insert urinary catheter :empty the bladder allow monitoring of UOP.
- Monitor(HR Pulse O2 saturation ).
- If any evidence of coagulopathy. Involve the haematologist.

Treatment of Atony
- Call for help
- ABC
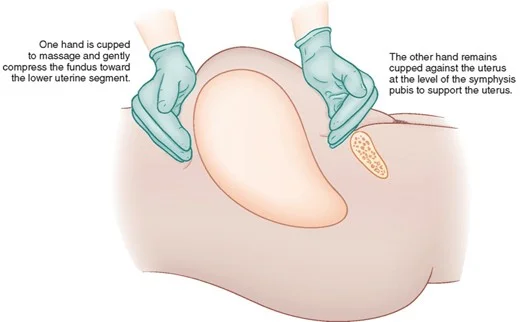
- Uterine massageZ
- Bimanual compression(Increase oxytocin infusion)Z
- Uterotonics()Z
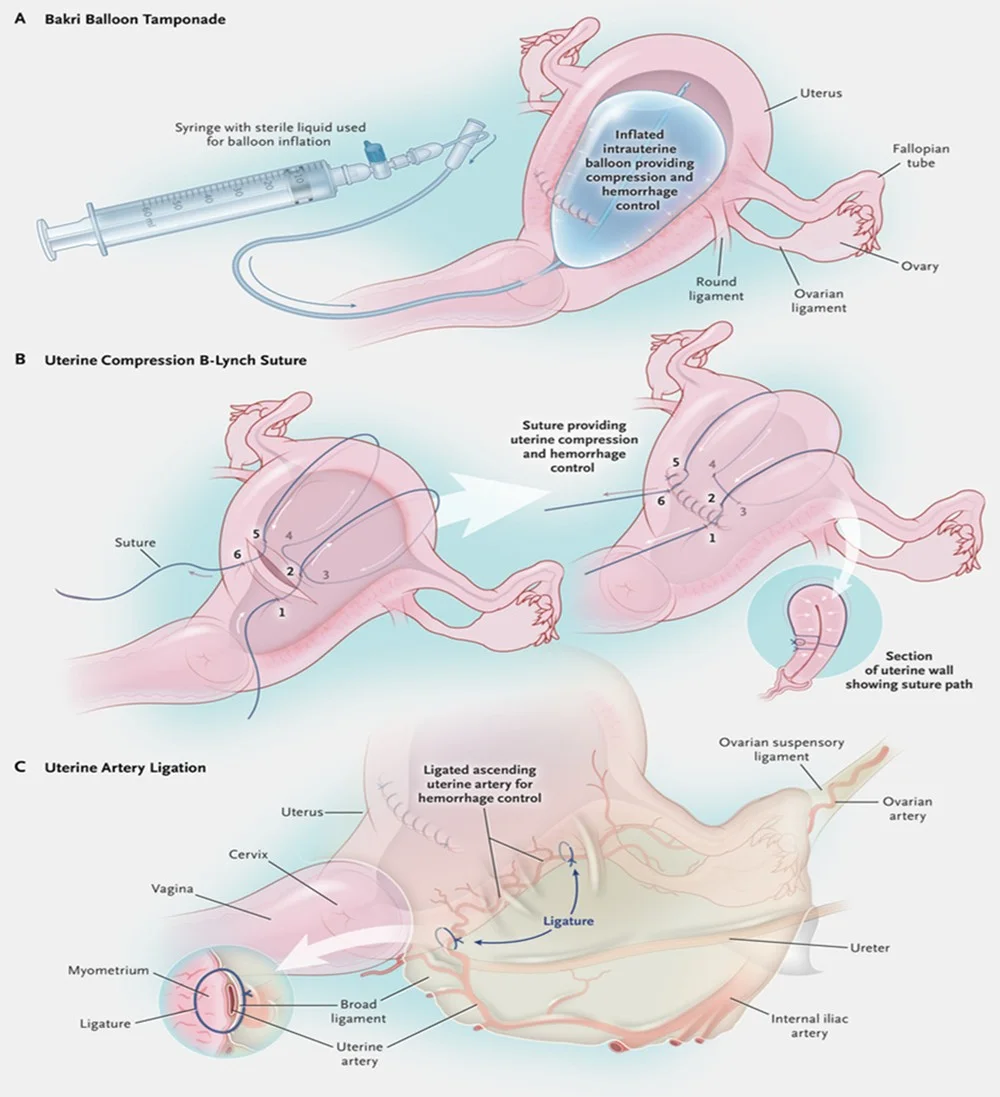
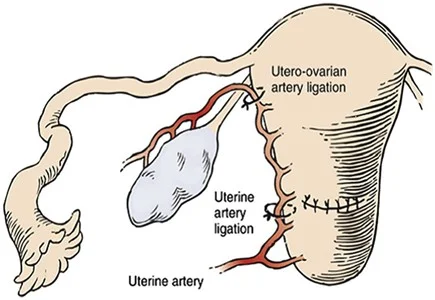
- Take the pt to the theatre
Management Techniques for PPH


Treatment of uterine inversion
Uterine Rupture - Hysterectomy

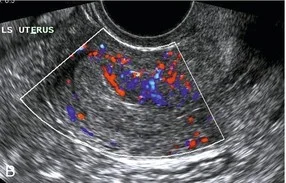
Tissue
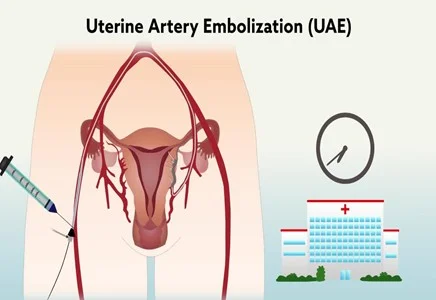
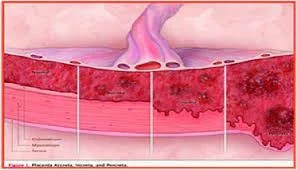
- Placenta accreta.
- Retained placenta.
- Retained products of conception.
Trauma
- Previous caesarean sections.
- Perineal tears.
- Episiotomy.
- Cervical laceration.
- Macrosomic baby.
- Instrumental delivery.
Thrombin
- Disseminated intravascular coagulation.
- Pyrexia in labour.
- Placental Abruption.
- Preeclampsia.
- Bleeding disorders.
- Use of Anticoagulants.
- Chorioamnionitis.

Others
- Asian ethnicity.
- Induction of labour.
- Anaemia.
- Obesity.
- Age >40 years.
- Prolonged labour.
Risk Factors for Secondary Postpartum Haemorrhage
- A history of primary PPH.
- Past history of PPH.
- Infections…C/S wound …Endometritis(uterine tenderness, fever or foul smelling lochia). …Mastitis. …UTI. …Others.
- Manual removal of placenta.
- PROM.
- Cancers.

Investigations
- U/S and Doppler study.
- CBC, C-RP and β-Hcg.
- Low vaginal, high vaginal, endocervical and rectal swabs.
- Coagulation profile.
- Midstream urine specimen.
- Blood cultures if temperature ≥ 38°C

Signs and Symptoms of Uterine Rupture
- Abdominal tenderness.
- Circulatory collapse.
- Elevation of presenting fetal part.
- Fetal bradycardia.
- Increasing abdominal girth.
- Loss of uterine contractions.
- Maternal tachycardia.
- Vaginal bleeding
Complications of Postpartum Haemorrhage
- Anaemia
- Anterior pituitary ischemia with delay or failure of lactation (i.e., Sheehan syndrome or postpartum pituitary necrosis)
- Blood transfusion
- Death
- Dilutional coagulopathy
- Fatigue
- Myocardial ischemia
- Postpartum depression.
- Orthostatic hypotension