IM
DR WAQAR
DEFINITION
Accumulation of more than 25 cc of fluid in the peritoneal cavity is called ascites.
( normally, only about 25 cc fluid in the cavity)
GRADES OF ASCITES
- Grade 1: Mild ascites, only detected by ultrasound. Physical exam normal.
- Grade 2: Moderate ascites, causing moderate abdominal & flank distension
- Grade 3: Large ascites, causing huge abdominal distension ( Grade 2 & 3 can be detected by physical exam)
At least 1.5 L fluid should be present in the abdomen so as to be detected by examination
S/S
Patient’s complaints:
- No complaints ( if very little fluid)
- Abdominal distension
- Respiratory distress
On Examination :
- Normal ( if very little fluid)
- Abdominal distension if significant fluid is present
- Shifting dullness if significant fluid is present
- Fluid thrill if significant fluid is present
- Umbilicus may be bulging if significant fluid is present
CLASSIFICATION
Ascites can be divided into 2 main types according to the protein concentration of the fluid
- TRANSUDATE: Protein less than 30g/L in the ascitic fluid.
- EXUDATE: Protein more than 30 g/L
A better way of classification is the SAAG ratio
( Serum to Ascites Albumin Gradient)
SAAG
- Serum albumin minus ascitic fluid albumin ( albumin difference)
- This difference can be more than 1.1g/100cc or less than 1.1g/100cc
So, ASCITES WITH SAAG > 1.1 OR SAAG < 1.1
CAUSES OF ASCITES
SAAG > 1.1
- Cirrhosis wth/portal HTN
- Portal HTN due to any other cause
- Heart failure
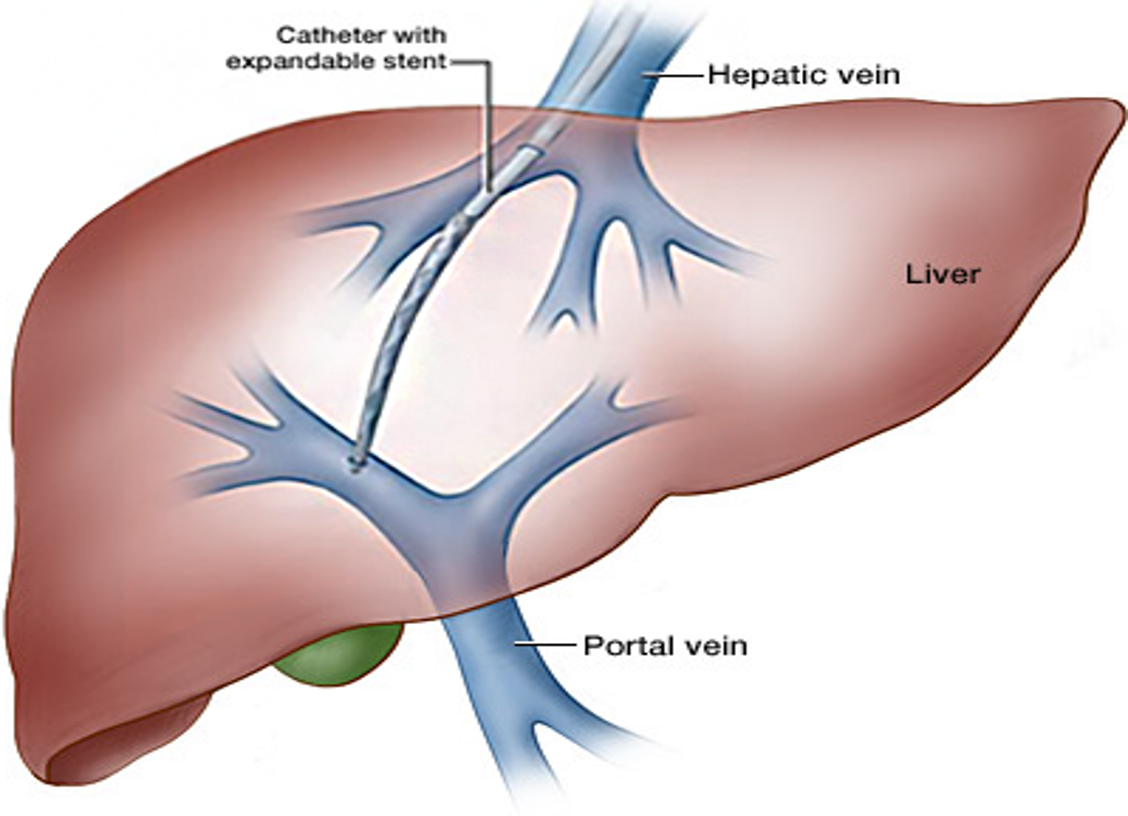
- Budd-Chiari syndrome (hepatic vein obstruction)
- Spontaneous bacterial peritonitis
SAAG < 1.1
- Bacterial & fungal peritonitis
- Tuberculous peritonitis
- Nephrotic syndrome
- Pancreatitis
- Low serum albumin
Some other types of Ascites
-
Hemorrhagic ascites: due to malignancy
-
Chylous ascites:
- Collection of white “milky” fluid
- Rich in fats/Triglycerides
- Occurs in lymphomas, TB peritonitis
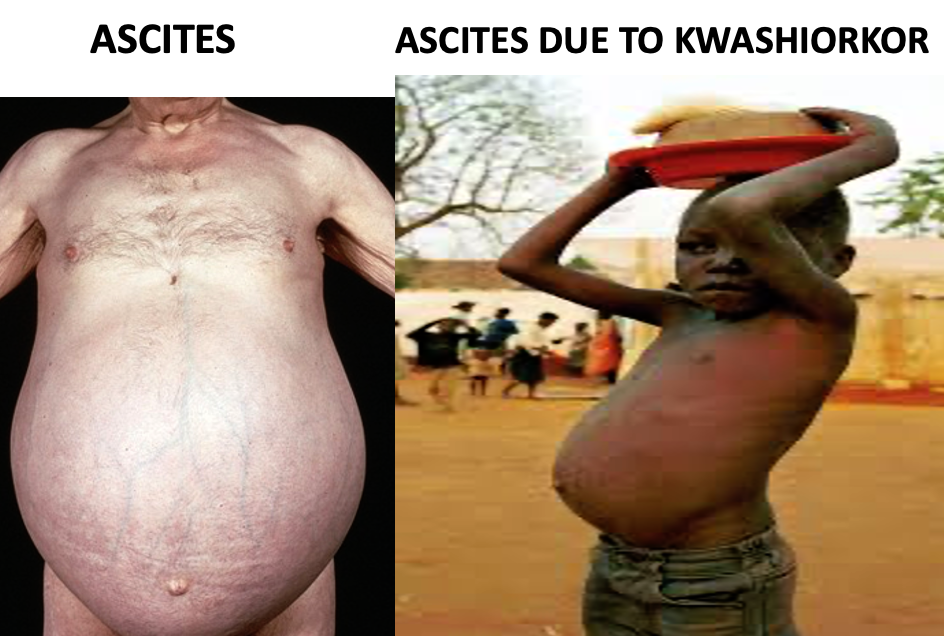
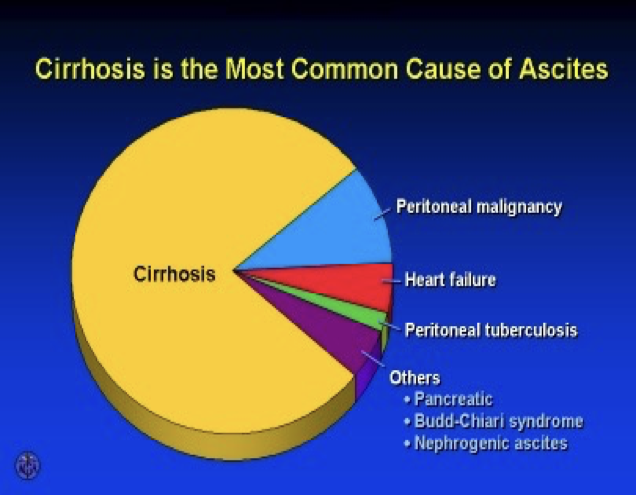
COMMONEST CAUSE OF ASCITES IS CIRRHOSIS W/ PORTAL HTN Why ascites occurs in cirrhosis
- Low serum albumin ⇒ low oncotic pressure ⇒ ascites
- Backpressure in portal vein ⇒ fluid comes ⇒ out
INVESTIGATIONS IN ASCITES
- CBC, electrolytes, serum albumin
- LFTs
- Hepatitis serology
- Abd. ultrasound
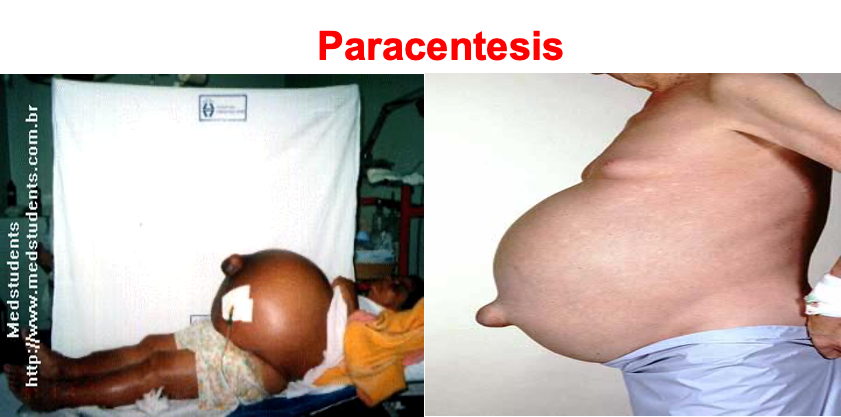
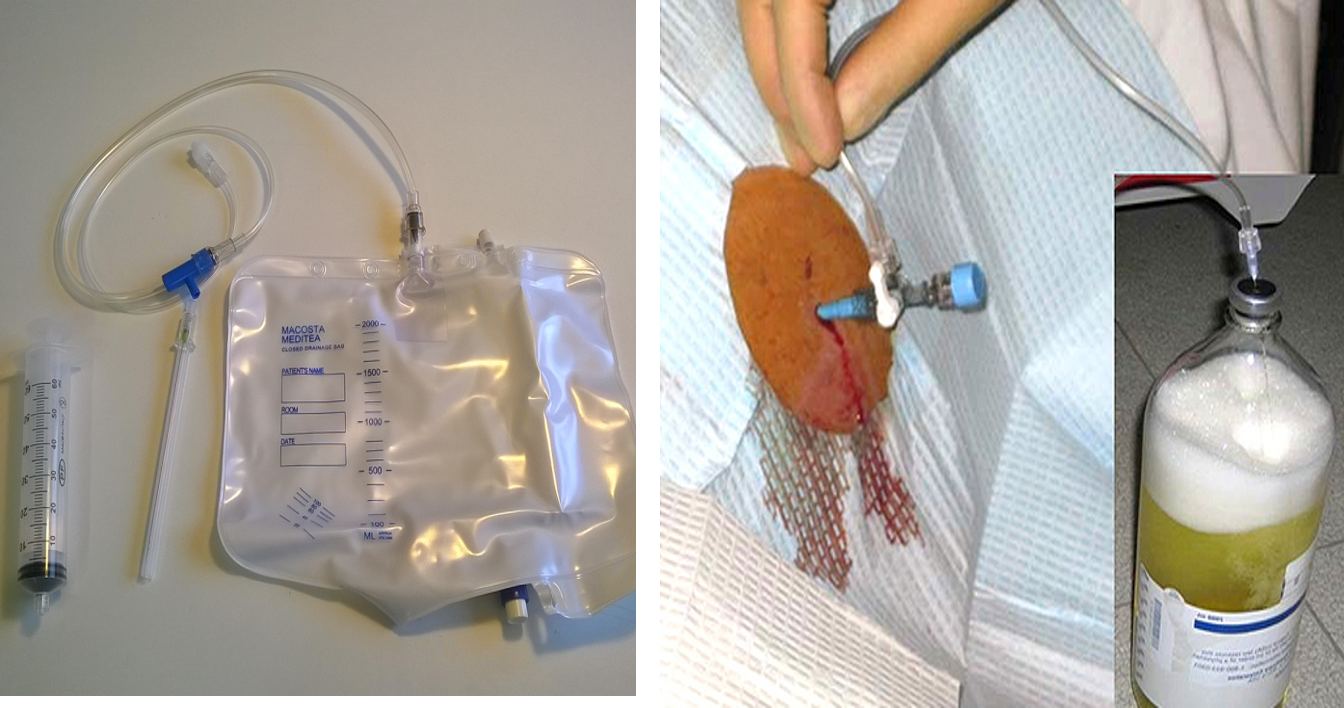
- Paracentesis(ascitic tap):
- Every new patient with ascites should get a “diagnostic” tap:
- Take out 10-20 cc fluid
- Check albumin (to calculate SAAG), neutrophils (to see infection), RBC, Gram stain & culture, cytology (malignant cells), amylase levels (in suspected pancreatic ascites)Z
Complications of paracentesis:
- Infection * Intestinal perforation
Relative contraindications:
- Pregnancy
- Bleeding disorders
MANAGEMENT OF ASCITES
Low salt & water intake | Diuretics | Paracentesis
In very resistant ascites, a procedure called TIPS is sometimes used.
(transjugular intrahepatic porto-systemic shunt).
MANAGEMENT OF ASCITES
- Low salt & water: < 2 g/d of salt ( less than ½ tea spoon)
- Diuretics:
-
Spironolactone ( aldactone): 1st choice. side effects : gynecomastia, hyperkalemia
-
Can add lasix (furosemide) if needed
-
Reduce ascites gradually (0.5 to 1 kg wt. loss daily). Too much wt. loss “suddenly” is not good!
-
*In 95% of cases, ascites can be controlled by 1) & 2) *
- “Therapeutic Paracentesis”
- It is done if medicines don’t help (resistant ascites) or very big ascites causing respiratory difficulty.
- Up to 7 L can be removed at one time.
- Removal of more than 7L can cause problems like hypotension, renal failure, encephalopathy
- i.v. albumin given at the time of paracentesis can prevent these complications
Complications of Ascites
- SPONTANEOUS BACTERIAL PERITONITIS (S.B.P.)
- Resp. distress (spontaneous bact. peritonitis)
Other Presentations
RAPID FIRE QUES SDL
-
More than how much fluid is detectable by examination?
-
How to detect ascites by physical exam?
-
How do you classify ascites based on albumin content? Which ratio?
-
What is the commonest cause of ascites?
-
Name some causes of ascites with SAAG more than 1.1?
-
Name some causes with ratio less than 1.1?
-
Hemorrhagic ascites means?
-
What is chylous ascites?
-
What color is chylous ascites?
-
Which disease causes chylous ascites?
-
What investigations to do in ascites patient?
-
After paracentesis, what things to check in the fluid?
-
Complications of paracentesis?
-
When not to do paracentesis?
-
Name 3 basic ways to treat ascites?
-
Which procedure to do in resistant ascites?
-
Which diuretic is the best?
-
Name 2 side effects of this diuretic?
-
Patient with ascites. Weight is 80kg. Diuretic started. Weight next day was 75kg. Good or bad?
-
During large volume paracentesis, what complications can happen?
-
What to give to prevent them?
-
Name 2 complications of ascites?
-
What is SBP?
-
Diagnostic test for SBP?
-
How does it present?
-
2 risk factors for SBP?
-
Ascitic fluid shows bacteria, neutro. Count 100 cells. Is this SBP?
-
Ascitic fluid shows no bacteria, neutro count is 300. Is this SBP?
-
What to give for secondary prophylaxis of SBP?
-
What is Budd Chiari syndrome?
-
S/S?
-
Risk factoirs for BUDD CHIARI?
-
Treatment of Budd Chiari?
Surgery
-
Collection of excessive, free intraperitoneal fluid
-
Fluid movement: hydrostatic/ colloid pressure balance
-
Clinical assessment:
- Fluid thrill (large)
- Shifting dullness (small)
-
Causes:
- Transudates (Protein <25/L)- low pp, CCF, PH
- Exudates: TB, peritoneal malignancy, chylous, pancreatic ascites
-
Diff. diagnosis:
- Int. obst., large ovarian cyst/abd. mass, advance pregnancy
-
Investigations:
- underlying cause, US, CT
-
TREATMENT:
- Underlying cause, low Na diet, diuretics, paracentesis, peritoneo-venous shunt (LeVeen)

Therapeutics
Fluid accumulation within peritoneal cavity
Causes:
(cc TB)
most important cause is liver cirrhosis
Mechanism of cirrhotic ascites:
A- Classic Starling theory: Hypoalbuminaemia decrease plasma osmotic pressure (ascetic threshold= 3) and due to portal hypertension (act as localizing factor which localizes fluid in the peritoneal cavity rather than peripheral tissues)
B-generalized fluid retention:
- hyperaldosteronism due to decreased renal blood flow which stimulate RAS also, due to decreased degradation of aldosterone by the liver.
- Others:
Complications:
1- Spontaneous bacterial peritonitis with:
- Clinical manifestations:
- clinical onset of Fever, chill
- generlaized Abdominal pain
- Abdominal tenderness
- Altered mental status
Can be treated by amioglycosides and ampicillin or third. generation cephalosporin or quinolones.
2-Complication due to treatment e.g hepatorenal syndrome if vigorous dieresis.Z
Treatment :
- Bed rest to decrease metabolites handled by the liver and to increased renal perfusion.
- diet: Na and water restriction.
- diuretics:
- best is I.V albumin. ((rational treatment; due decreased liver function))
- Spironolactone (maximum rate of ascetic fluid mobilization is 1-2 L / day and if very rapid (dehydration, hepatorenal syndrome and electrolyte imbalance and hepatic encephalopathy)Z
Medical Management of Ascites:
Diuretic therapy: ParacentesisZ have patient void before procedure then needle puncture of abdominal cavity to remove ascitic fluid- temporary
Assessment/Grading of ascites
-
Grade 1 — mild; Detectable only by US
-
Grade 2 — moderate; Moderate symmetrical distension of the abdomen
-
Grade 3 — large or gross asites with marked abdominal distension
Imaging studies for confirmation of ascites Ultrasound is probably the most cost-effective modality