IM
HEPATITIS B
Epidemiology
- Worldwide problem, especially in Africa, the Middle East, and South America.
- 1/3rd of the world population has serological evidence of past or present infection.
- About 1 million deaths occur per year due to Hep B-related liver disease and carcinoma.
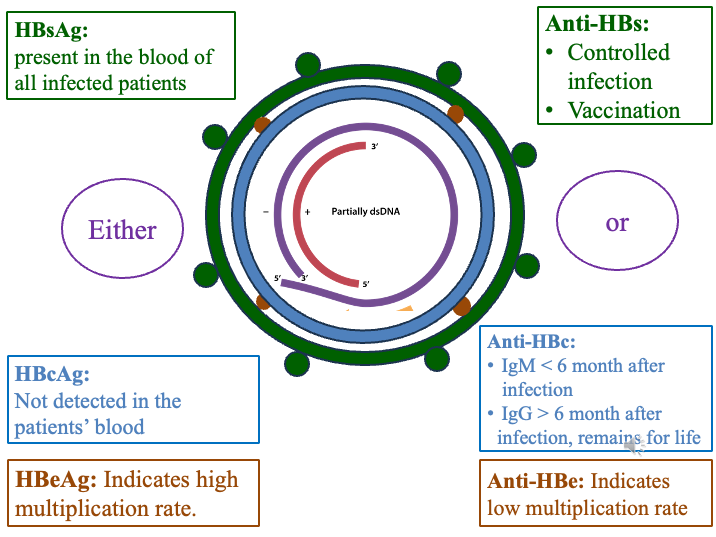
Structure of Hepatitis B Virus
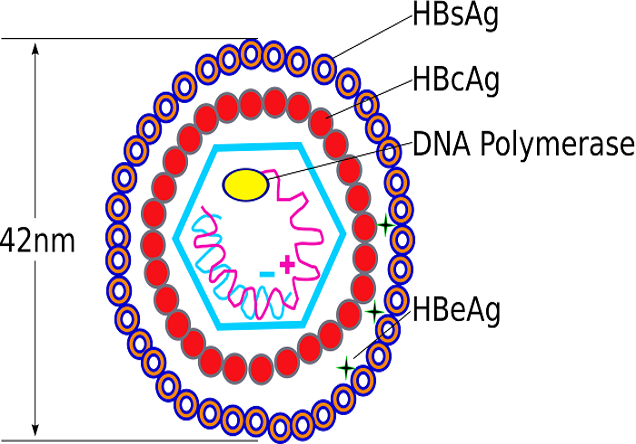 The Hepatitis B virus is a DNA virus (Hep A and Hep C are RNA viruses). It has the following structure:
The Hepatitis B virus is a DNA virus (Hep A and Hep C are RNA viruses). It has the following structure:
- Outer Covering: Contains the surface antigen (s ag).
- Inner Center: Contains:
- “e” antigen (envelop antigen)
- “c” antigen
- DNA
Serologic Markers
- After infection with Hep B, “s” antigen, “e” antigen, and Hep B DNA are detectable in the blood.
- “c” antigen is not detectable in the blood.
Antibodies that appear in the blood and clear the infection:
- Anti-HBs (against “s” antigen)
- Anti-HBe (against “e” antigen)
- Anti-HBc (against “c” antigen)
Note:
- Appearance of Anti-HBs and Anti-HBe means infection is resolved.
- Anti-HBc does not kill the virus.
Routes of Transmission
1. Vertical Transmission (Mother to Fetus)
- Most common route worldwide.
2. Parenteral Transmission (Through Blood)
- Needle sharing (IV drugs, tattooing)
- Transfusion of infected blood and blood products (rare in developed countries due to blood screening).
- Needle stick injuries (doctors and nurses at high risk)
- Sexual transmission
- Direct contact with the blood of a Hep B patient (even small skin breaks are risky)
Note: Saliva, sweat, and tears also contain the virus but are not considered significant modes of transmission (may spread).
Spectrum of Hepatitis B Infection
Hepatitis B can cause:
- Acute Hepatitis: Duration less than 6 months.
- Chronic Hepatitis: Duration more than 6 months.
Chronic Hepatitis B can be further classified into:
- Chronic Active Hepatitis
- Chronic Carrier State
Acute Hepatitis B
- Incubation Period: Highly variable, averaging 6 weeks.
- Symptoms:
- Jaundice and other symptoms similar to Hep A.
- May be asymptomatic.
Blood Tests:
- LFTs: ↑ Bilirubin, ↑ AST, and ↑ ALT (similar to Hep A).
- Hep B Serology: Antigens and antibodies.
Serology in Acute Hepatitis B
Antigens that appear:
- “s” antigen
- “e” antigen
- Hep B DNA levels
Antibodies that appear:
- Anti-HBs (indicates recovery) (first to appear in blood)
- Anti-HBe (infectious)
- Anti-HBc (indicates recovery) Z
Serconversion: Disappearance of antigens and appearance of antibodies.
Anti-HBc Antibody:
- Does not kill the virus.
- Appears early in infection and persists forever.
- Initially IgM type, then changes to IgG type.
IgM + IgC in window period
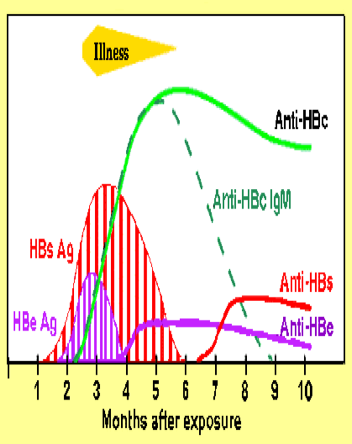
Important Points (Acute Hepatitis B)
- “s” antigen is the first to appear in the blood.
- “e” antigen is highly infectious.
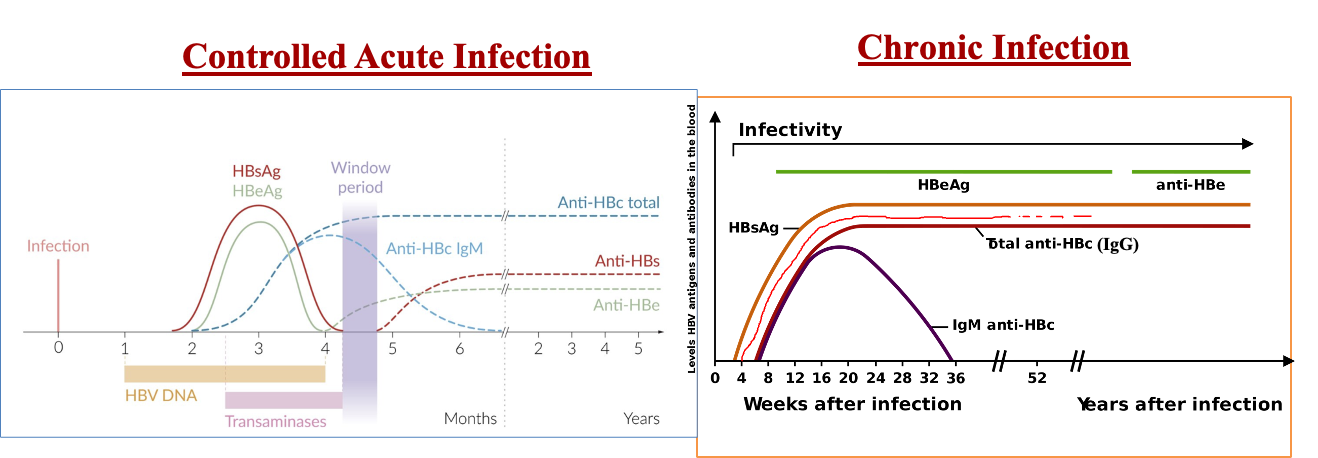
- Window Period: Time period when infection has just resolved. “s” antigen has disappeared, but Anti-HBs antibody is still undetectable. Only Anti-HBc IgM type is positive.
Treatment of Acute Hepatitis B
- Symptomatic treatment.
- Usually, no specific treatment is needed in acute cases.
Chronic Hepatitis B
Chronic (Active) Hepatitis:
- Infection present for more than 6 months.
- Patient may or may not have symptoms.
- Elevated LFTs and abnormal liver biopsy.
- “s” antigen, “e” antigen, and Hep B DNA present in the blood.
- Patient is highly infectious (because “e” antigen is present).
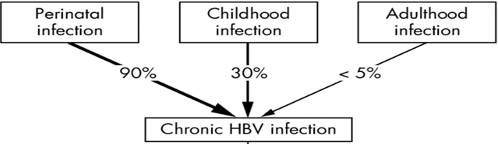
- Higher chances of chronic infection in children and people with poor immunity (diabetes, long-term steroid use, HIV, etc.).
Chronic (Carrier) State:
- Infection present for more than 6 months.
- Patient is asymptomatic.
- Normal LFTs and biopsy.
- “s” antigen present in the blood.
- No “e” antigen in the blood (so the patient is much less infectious).
- DNA levels may be low or absent in the blood.
Comparison of Chronic Active Hepatitis B and Chronic Carrier State
| Feature | Chronic Active Hepatitis B | Chronic Carrier State |
|---|---|---|
| Symptoms | Usually symptomatic | Usually asymptomatic |
| LFTs & Biopsy | Abnormal | Normal |
| ”e” Antigen | Present | Absent |
| Hep B DNA Levels | High | Low or Absent |
| Treatment | Given | Not Given |
Serologies in Different Phases of Hepatitis B
- Acute Hep B:
- “s” antigen positive
- “e” antigen positive
- Anti-HBc positive (IgM type)
- Anti-HBs negative & Anti-HBe negative
- Resolved Infection:
- “s” antigen negative
- “e” antigen negative
- Anti-HBc positive (IgG type)
- Anti-HBs positive
- Anti-HBe positive
- Window Period:
- “s” antigen negative
- “e” antigen negative
- Anti-HBc positive (IgM type)
- Anti-HBs negative
- Chronic Hepatitis (Active & Carrier):
- “s” antigen positive
- “e” antigen positive (in active hepatitis)
- Anti-HBc positive (IgG type)
- Anti-HBs negative
- Anti-HBe negative (in carrier state)
Look for the “s” antigen first.
Positive “s” antigen: Infection present. Could be
- acute,
- chronic active, or
- chronic carrier state in hepatitis Negative “s” antigen: No current infection. Could be due
- never being infected,
- resolved infection,
- window period (igm, anti-hbc)
- vaccination (anti-s).

Treatment of Chronic Hepatitis B
Drugs: * Nucleoside analogues: e.g., Entecavir (oral) * Nucleotide analogues: e.g., Tenofovir (oral) * Interferon: (Injections)
- Treatment duration is typically 6 months to 1 year.
- Treatment is not given to chronic carriers (patients who have only “s” antigen positive with normal LFTs and normal liver biopsy).
Liver Transplant:
- Considered in end-stage liver disease or fulminant hepatic failure.
So
- Acute hep B: no antiviral meds
- Chr. Active hep B: antiviral meds yes
- Chr carrier : no meds
Prevention of Hepatitis B
- Avoid risk factors: IV drug use, needle sharing, sexual contact with an unknown or Hep B-positive person, avoid direct contact with blood, no sharing of razors, etc.
- Vaccination: Given routinely to everyone.
- 3 doses: 0, 1 month, 6 months (from the first dose).
- Immune Globulins: Given for immediate protection if:
- Needle stick injury from a Hep B patient.
- Sexual exposure to a Hep B patient.
- Newborn baby (if the mother is Hep B positive).
Important Notes:
- Vaccines: Produce protective antibodies after some time (weeks to months) but provide long-term immunity.
- Immunoglobulins: Provide immediate protection but only for a short time.
Complications of Chronic Hepatitis B
- Cirrhosis
- Hepatic Carcinoma (Liver Cancer)
Hepatitis B and Pregnancy Z
- High chances of vertical transmission, so Hep B-positive mothers should be treated.
- Tenofovir is safe to give during pregnancy. Z
- Breast milk does not transmit the infection to the baby.
- Babies born to Hep B-positive mothers should receive the Hep B vaccine and Hep B immunoglobulin within 12 hours of birth. Z
Rapid Fire Questions (Hepatitis B)
- What are the modes of transmission? Vertical, parenteral
- Name the 3 antigens of Hep B. S, C, E
- Which antigen is not detectable in the serum? Anti-C
- Which antibody is not protective (does not kill the virus)? Anti-C
- Of all the antigens, which is the most important to check to see infection? S & C
- Appearance of which antibodies means infection is resolved? anti-s & anti-e
- Saliva, sweat, and tears of a Hep B patient are highly infectious, right or wrong? wrong
- Duration of acute Hep B? <6M
- Duration of chronic Hep B? >6M
- Name the 2 types of chronic Hep B. Active/Carrier
- Name 2 differences between the 2 types of chronic Hep B. Biopsy & LFT
- What will LFTs show in acute Hep B? High LFT, AST & ALT, direct bilirubin
- What do you mean by “seroconversion”? change antigen to antibody
- In the window period, what is detectable in the blood? Anti-… cc
- Which antiviral drug is used to treat acute Hep B? no antivirals
- In acute Hep B, what is detectable in the blood? chronic active only
- Which drug is used for the chronic carrier state? Interferons, … cc
- Name the drugs used for Hep B treatment. interferons
- What’s the vaccination schedule for Hep B? 0, 1, 6
- Who should get vaccinated? Everyone, espicially children
- What to give immediately after exposure? immunoglobulin anti-s
- Vaccines provide quick immunity, right or wrong? Wrong
- Complications of chronic Hep B? liver cirrhosis, carcinoma
- Hep B is a contraindication to pregnancy, right or wrong? wrong, can be treatment
- What to give to a pregnant lady who has chronic Hep B? tenovofil
- During pregnancy, the Hep B virus goes to the baby during which trimester? at delivery vertical
- Baby born to a Hep B mother. How to deal with it? vaccination and i on one and other hand cc
Thera
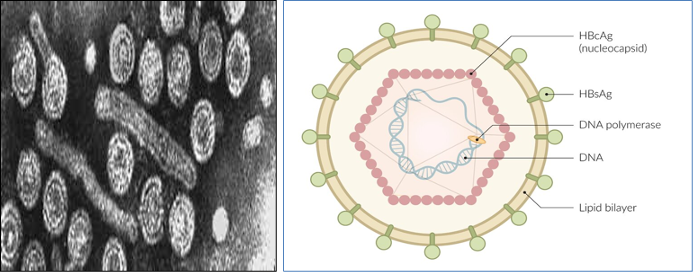
Viral structure:
- Lipid envelope with surface antigen (HBsAg).
- HBeAg.
- Viral core protein (HBcAg)
- Partial double strand DNA.
- RT: Reverse transcriptase enzyme.
Transmission
- Parenteral (blood transfusion, needlestick, tattooing, piercing….)
- Perinatal (during birth)
- Sexual contact.
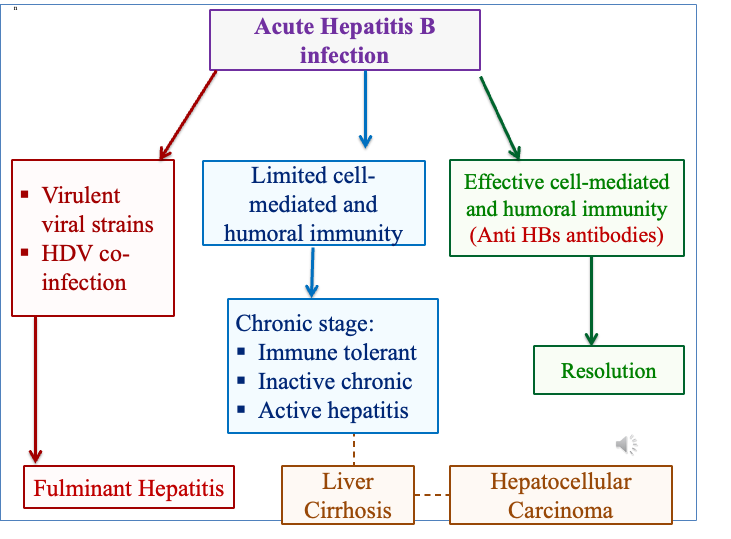
Pathogenesis and the Immune Response:
- Acute Infection:
- Entry into hepatocytes is mediated by the surface antigen.
- Interferon-α production → cell-mediated immune response.
- Destruction of the hepatocytes by the T cytotoxic cells.
- Production of anti-HBcAg +/- anti-HBsAg +/- anti-HBeAg.
- Chronic infection:
- Failing immune clearance→ viral persistence→ persistent inflammation → necrosis and regeneration processes → cirrhosis→ hepatocellular carcinoma (HCC).
- Integration of HBV DNA into the host genome → HCC
Clinical Presentation:
Acute phase: infection acquired during the last 6 months
- Incubation period: 1-6 months.
- 70%: Asymptomatic (anicteric hepatitis): greater risk for chronic infection.
- 30%: Symptomatic (icteric hepatitis): Anorexia, nausea, vomiting, low-grade fever, myalgia, arthralgia, rash, right upper quadrant pain, jaundice.
- Fulminant hepatitis: Hepatic encephalopathy, disturbances in sleep pattern, confusion, coma, ascites, gastrointestinal (GI) bleeding, coagulopathy.
- Chronic phase: persistence of DNA & HBs Ag > 6 months
Symptoms in chronic phase are the same acute symptoms.Immune tolerance: high viral load with minimum hepatic damage. Leads to active hepatitis after 30 years.
Risk for chronicity:
- 90% in infants
- 30% in children 1-5 years old
- 5% in adults
Phases of chronic infection:
-
Immune tolerant: Asymptomatic, infection during birth or early infancy.
-
Inactive chronic (carrier state): Asymptomatic
-
Active hepatitis: Symptomatic Highest risk of cirrhosis & HCC. Target for HBV treatment.
-
Symptoms in chronic phase are the same acute symptoms. -
Active & immune tolerant: HBeAg +ve (active replication) -
Inactive (little viral replication): Anti-HBe Abs +ve limited replication -
If the AST levels are higher than the ALT levels, the diagnosis of cirrhosis must be considered.
Most of the patients are asymptomatic, but patients with anicteric hepatitis have a greater tendency to develop chronic hepatitis.
Some patients clear HBV and develop anti-HBs; however, as long as the individual has antibody to hepatitis B core antigen (HBcAg), he or she is at risk for reactivation because HBV infection remains an incurable disease, like EBV, CMV, HSV infections.
The term “healthy carriers” is no longer used because a person who is positive for HBsAg has a high risk of cirrhosis and hepatocellular carcinoma (HCC) and, therefore, cannot be defined as healthy.``
Laboratory Diagnosis
- Liver function test.
- PCR: measure viremia for follow up of the treatment.
- Serology:
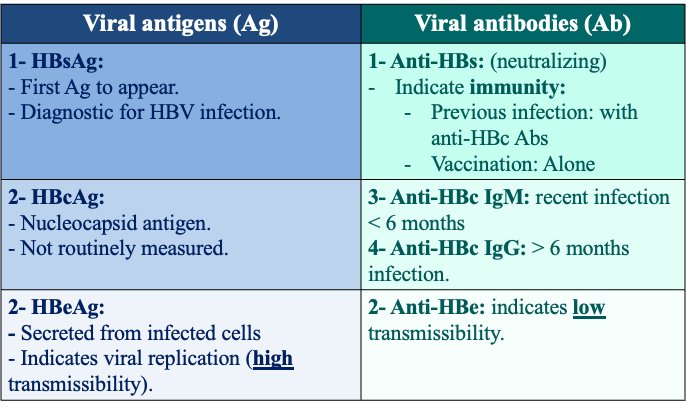
IgM anti-HBc is generally detectable 4 to 6 months after onset of illness and is the best serologic marker of acute HBV infection.
HBc Ag does not circulate as a free protein in significant quantities in the blood.
To evaluate the patient’s level of infectivity, quantification of hepatitis (HBV) DNA is essential, and the presence of hepatitis B e antigen (HBeAg) should be determined. Indeed, the best indication of active viral replication is the presence of HBV DNA in the serum.
Diagnosis of Hepatitis B Infection T
Incubation period:
- HBs Ag
- HBe Ag.
Convalescence phase:
- HBs Antibodies (neutralizing).
- Anti-HBc IgG Antibodies
Window period:
- Anti HBc IgM.
Acute icteric phase:
- HBs Ag
- HBe Ag.
- ↑ HBc IgM antibodies.
Chronic period > 6 months:
- HBs Ag: positive
- Anti-HBs Antibodies: negative.
- Anti-HBc IgG Antibodies: positive.
- HBe Ag (+ve/-ve)
Vaccinated:
- Anti-HBs Abs.
Low vaccination response: obesity, smoking, immunosuppression, and advanced age. Approximately 25-50% of persons who initially do not have a vaccine response will show a response to 1 additional vaccine dose, and 50-75% of individuals will have a response to a second 3-dose series.
Testing for anti-HBs: 4-12 weeks following vaccination.
Do not defer vaccination in pregnant patients.
| HBsAg (Active Infection) | Anti=HBc IgM (Window Peroid) | Anti-HBc IgG (Chronic/Treatment) | Anti-HBs (Resolved/Vaccinated) | Diagnosis |
|---|---|---|---|---|
| + | + | - | - | Acute |
| - | + | - | - | Window |
| - | - | + | + | Resolved |
| + | - | + | - | Chronic tolerant; +Ve HBeAg Inactive; -Ve HBeAg Active; +Ve HBeAg |
| - | - | - | - | Not infected |
| - | - | - | + | Vaccinated |
Treatment:
Pegylated interferon, reverse transcriptase inhibitors,
Prevention:
Active vaccination:
- Recombinant hepatitis B surface antigen (HBsAg). Injectable 3 doses.
- Protective titer of anti-HBs antibodies ≥ 10 IU/mL.
Post exposure prophylaxis: hepatitis B immunoglobulin (HBIG) + the active vaccine.
- Infants born to HBV infected mothers
- Needle stick injury
- Sexual contact
Currently used drugs: Nucleoside/nucleotides analogs: tenofovir, entecavir.
The vaccine contains antibiotics neomycin and polymyxin B, and streptomycin
HepB vaccination and 1 dose of HBIG administered within 24 hours after birth are 85% to 95% effective in preventing chronic HBV infection. HepB vaccine administered alone beginning within 24 hours after birth is 70% to 95% effective in preventing perinatal HBV infection.
Older age (40 years and older), male gender, obesity, diabetes, smoking, and chronic illness have been independently associated with nonresponse to HepB vaccine.
E antigen was named e because three antigens were discovered before it and were named a b c. https://link.springer.com/article/10.1007/s11262-020-01733-9 . Could be e for extra particulate or extra ordinary.
C stands for capsid is more logical than core.
Ten HBV genotypes, designated A through J, have been described. Immunity by one genotype confers immunity to all the other types
Approximately third the population are infected. 250-350 million people have lifelong chronic infection, [3] with approximately 1.5 million new cases every year.
HBV can survive for 15 years at –20°C, for 6 months at room temperature, and for 7 days at 44°C. Indeed, the approximately 400-year-old mummified remains of a child found on a mountain top in Korea had HBV in the liver that could be sequenced, and a viral genotype C was identified.
Lower titers are found in other fluids, such as saliva, tears, urine, and semen. saliva can be a vehicle of transmission through bites.
most body fluids are not efficient vehicles of transmission (unless they contain blood) because they contain low quantities of infectious HBV.``