Atrial Fibrillation (AFib)
Definition: Atrial Fibrillation (AFib) is a common type of arrhythmia, or irregular heartbeat, where the atria (the upper chambers of the heart) beat irregularly and often rapidly. This irregular rhythm can lead to poor blood flow and increase the risk of stroke, heart failure, and other heart-related complications.
Types of AFib:
- Paroxysmal AFib: Episodes come and go, usually lasting less than 7 days, and often resolve on their own.
- Persistent AFib: Episodes last longer than 7 days and may require treatment to restore normal rhythm.
- Long-standing Persistent AFib: Continuous AFib lasting more than 12 months.
- Permanent AFib: The irregular rhythm cannot be restored to normal, and the condition is accepted as permanent.
Symptoms:
- Palpitations (feeling of a rapid, fluttering, or pounding heart)
- Fatigue
- Shortness of breath
- Dizziness or lightheadedness
- Chest pain (less common, but requires immediate medical attention)
- Weakness
- Reduced ability to exercise
Causes:
- High blood pressure
- Coronary artery disease
- Heart valve disease
- Heart failure
- Hyperthyroidism
- Sleep apnea
- Excessive alcohol or caffeine consumption
- Stress
- Certain medications
- Genetic predisposition
Risk Factors:
- Age (more common in older adults)
- Family history of AFib
- High blood pressure
- Obesity
- Diabetes
- Chronic kidney disease
- Smoking
- Excessive alcohol use
- Physical inactivity
Complications:
- Stroke: Blood clots can form in the atria due to poor blood flow, which can travel to the brain and cause a stroke.
- Heart Failure: The heart may not pump efficiently, leading to heart failure.
- Other Complications: Increased risk of other cardiovascular conditions, such as heart attack.
Diagnosis:
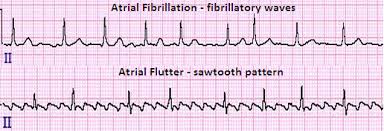
- Electrocardiogram (ECG or EKG): The primary test to diagnose AFib by recording the heart’s electrical activity.
- Holter Monitor: A portable ECG device worn for 24-48 hours to detect intermittent AFib.
- Event Monitor: Similar to a Holter monitor but used for longer periods.
- Echocardiogram: An ultrasound of the heart to assess its structure and function.
- Blood Tests: To check for underlying conditions like thyroid disease or electrolyte imbalances.
- Stress Test: To evaluate how the heart functions under physical stress.
Treatment:
-
Medications:
- Rate Control: Beta-blockers, calcium channel blockers, or digoxin to control heart rate.
- Rhythm Control: Antiarrhythmic drugs to restore and maintain normal rhythm.
- Anticoagulants: Blood thinners (e.g., warfarin, dabigatran, rivaroxaban) to reduce the risk of stroke.
-
Cardioversion:
- Electrical Cardioversion: A procedure where an electric shock is delivered to the heart to restore normal rhythm.
- Pharmacological Cardioversion: Use of medications to restore normal rhythm.
-
Catheter Ablation:
- A procedure where areas of the heart causing abnormal electrical signals are destroyed using radiofrequency energy or cryotherapy.
-
Surgical Procedures:
- Maze Procedure: A surgical technique to create scar tissue in the heart to block abnormal electrical signals.
- Left Atrial Appendage Closure: A procedure to reduce stroke risk by closing off the left atrial appendage where clots often form.
-
Lifestyle Modifications:
- Weight management
- Regular physical activity
- Limiting alcohol and caffeine intake
- Smoking cessation
- Managing stress
Prognosis:
- AFib is a chronic condition that requires ongoing management. With appropriate treatment, many people with AFib can lead normal, active lives. However, the condition does increase the risk of stroke and heart failure, so regular follow-up with a healthcare provider is essential.
Monitoring and Follow-Up:
- Regular check-ups with a cardiologist
- Monitoring of INR levels if on warfarin
- Periodic ECGs to assess heart rhythm
- Blood pressure and cholesterol management