IM
Absence seizures
| * Sudden onset | |
| * Interruption of ongoing activities | |
| * Blank stare | |
| * Brief upward rotation of eyes | |
| * Few seconds to 1/2 minute | |
| * Evaporates as rapidly as it started | |
| * Stops hyperventilating | |
| * Mild eyelid clonus | |
| * Slight loss of neck muscle tone | |
| * Oral automatisms |
Pediatrics
- Occurs in children aged 4-12 years
- More common in girls than boys
- Ceases at puberty
- Abrupt lapses of consciousness lasting a few seconds (5-10)
- No alteration in muscle tone
- May go unrecognized
- Abrupt in onset, no aura, and amnesia
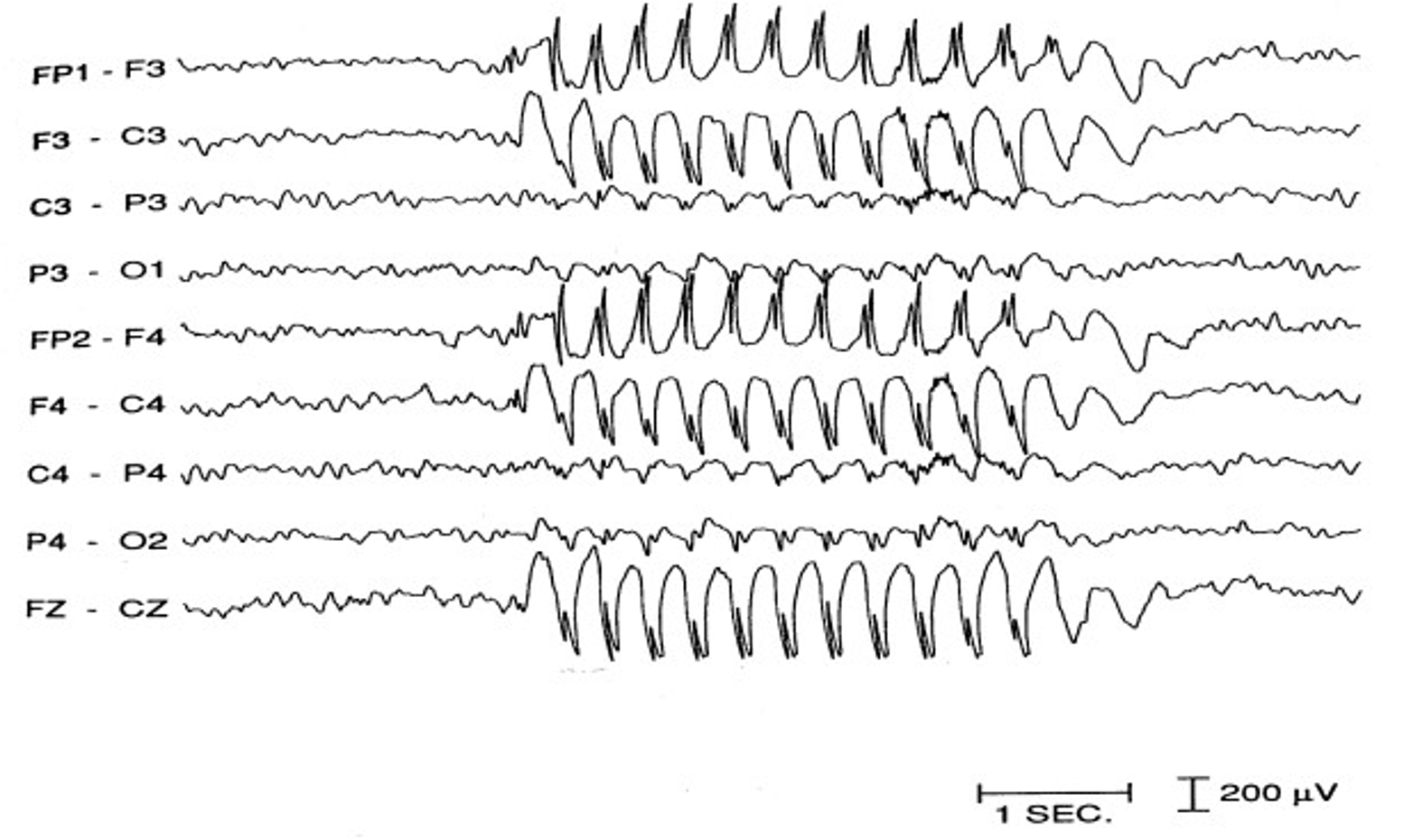
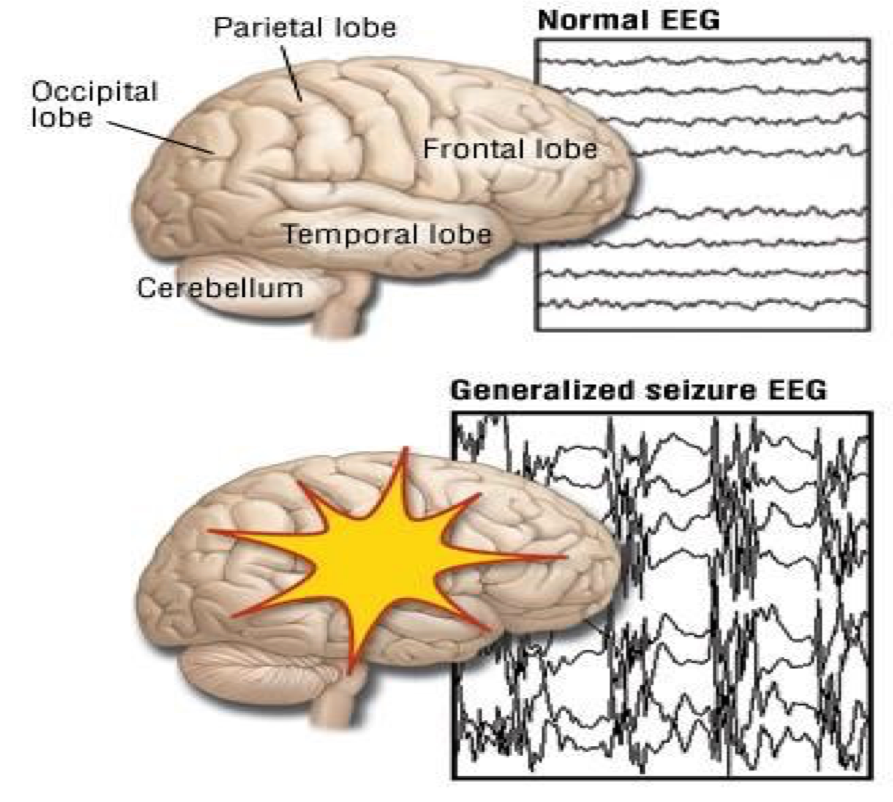
Diagnostic Evaluation
- History Collection
- Physical Examination
- Laboratory Investigations
- Serum glucose & calcium levels
- Lumbar puncture – 1st febrile seizures
Main Periods According to Age
Neonates
- Subtle seizures, non-febrile
- Deviation of the eyes
- Eyelids are flickering
- Swimming or pedaling movements
- Apnoeic spells
- Tonic
- Clonic
- Myoclonic
- Seldom tonic-clonic seizures
Infancy and Early Childhood (3 months to 3 years)
- Febrile seizures
- Infantile spasms
- Lennox Gastaut
- Myoclonic seizures
- Status epilepticus
- Partial complex
Childhood to Early Adolescence
- Cryptogenic
- Absences
- Benign rolandic epilepsy
Nine Years to Adulthood
- Primary generalized epilepsy
- Focal epilepsy with brain injury
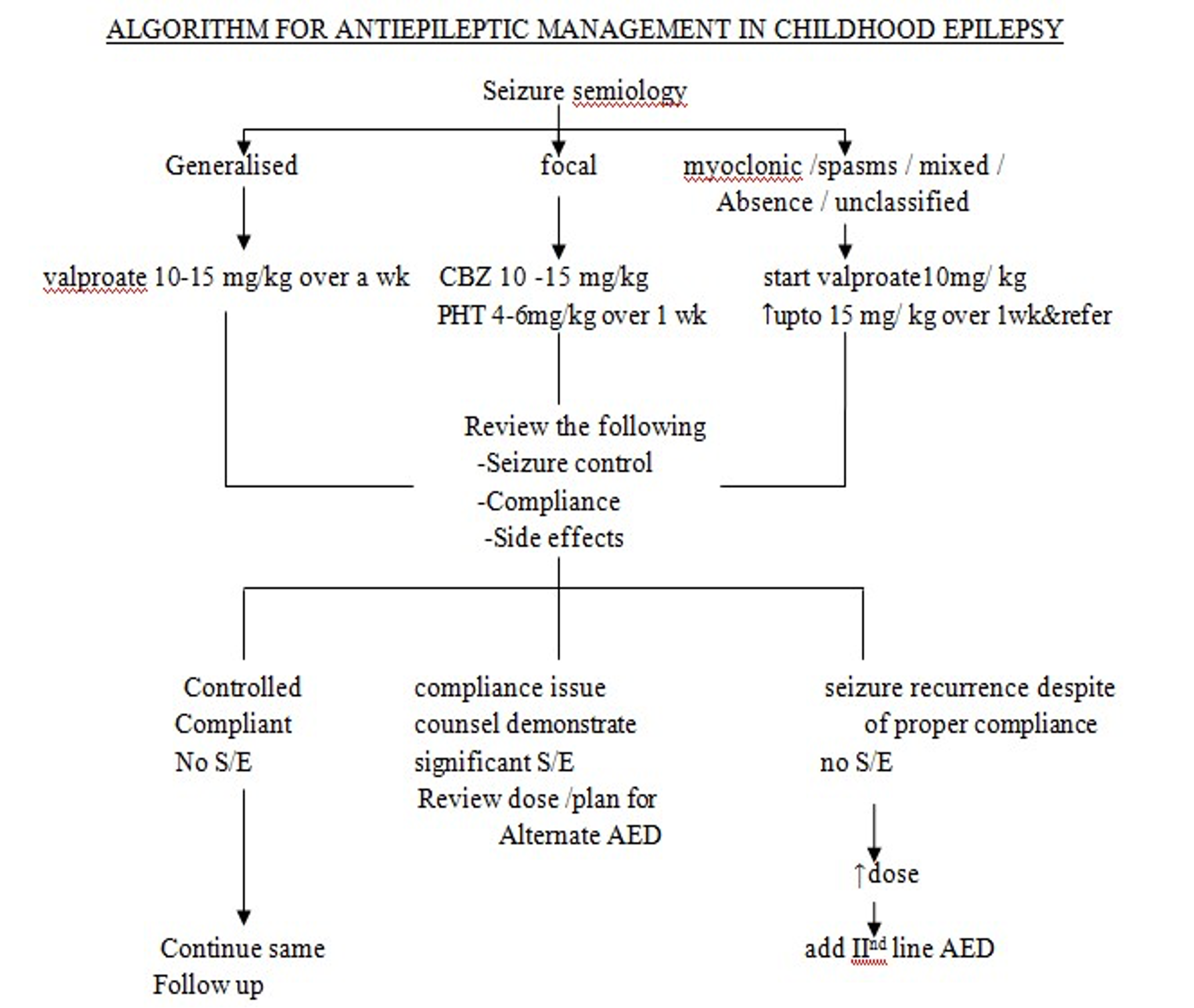
Steps in Management
- Confirm diagnosis
- Establish seizure type & syndrome
- Evaluate the need for treatment
- Select AED
- Start monotherapy (start slow, go slow policy)
- Switch to another monotherapy