Because of the health risks involved in exposure to ionizing radiation (cell death, teratogenicity, carcinogenicity), radiographical studies are bound to high safety standards.
It is recommends that all exams involving ionizing radiation should be performed only when medically necessary, i.e., for diagnosis, treatment, or guiding an invasive procedure.
Keeping the radiation dose “As Low as Reasonably Achievable“. (ALARA Principle)
ALARA Principle is achieved by:
-
Avoidance of unnecessary requests for x-ray examinations, particularly those that involve high radiation exposure such as lumbar spine x-rays and CT examinations.
-
If possible, alternative techniques such as ultrasound or MRI should be considered.
-
Appropriate equipment and good technique
-
Limiting the size of the x-ray beam to the required areas.
-
Limiting the number of films to those that are necessary.
-
keeping repeat examinations to a minimum and ensuring that the examination has not already been performed.
-
Exposed personnel monitored by a film badge
In fluoroscopy

DISTANCE: Radiation dose is high in fluoroscopy due to continuous x-rays use
- One step back from tableside: cuts exposure by factor of 4
- Move Image Intensifier close to patient: less patient skin exposure less scatter
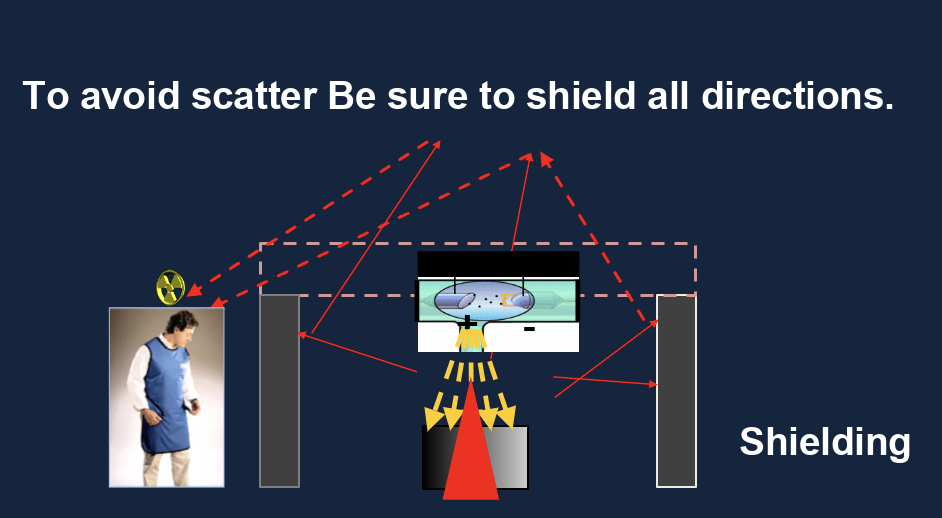
Shielding (Lead)
- Increasing the amount of shielding around a source of radiation will
- decrease the amount of radiation exposure.
In Nuclear Medicine
-
The radioisotopes used in medical diagnosis are artificially produced and most have short half lives, usually a few hours or days.
-
Nuclear medicine procedures are not recommended for pregnant women because unborn babies have a greater sensitivity to radiation than children or adults.; risk of cataracts.
To keep the radiation dose to the patient at a minimum: The smallest possible dose of an isotope with a short half life should be used.
The radiopharmaceuticals have undesirable biological effects and should be rapidly excreted from the body following completion of the investigation.
when a patient has been injected with radioactive substance maximize the distance from the patient.

Case
A 35-year-old woman comes to the physician as a new patient and requests a whole-body CT scan for cancer screening because she can feel that “there is something in her body.” Her medical history is unremarkable, and she takes no medications. She has had several jobs over the past 10 years but is currently unemployed and has Medicaid insurance. There is no family history of serious illness. Vital signs are within normal limits. Physical examination shows no abnormalities. The patient explains that she has seen several physicians in the past, but all of them refused to order the requested test for her. She says, “You seem wonderful, unlike my previous physicians. They were all incompetent!” On exploring the patient’s fear of cancer and the reasons for her inquiry, she reports that she saw an online direct-to-consumer advertisement about whole-body CT scans. The physician explains when whole-body CT scans are performed and why the test is not indicated in her case. The patient insists that the physician order the test. Which of the following is the most appropriate response to the patient’s request?
- “I understand that you are concerned about having cancer. I can order the test if you are willing to sign an against-medical-advice form.“
- “A whole-body CT scan is associated with high levels of radiation exposure. I would instead recommend an MRI scan, which is a safer alternative.“
- “There is no indication that you might benefit from this test. I cannot in good conscience order the test for you at this time.“
- “Unfortunately, your health insurance plan will not cover this test. Would you be willing to pay for it yourself?”