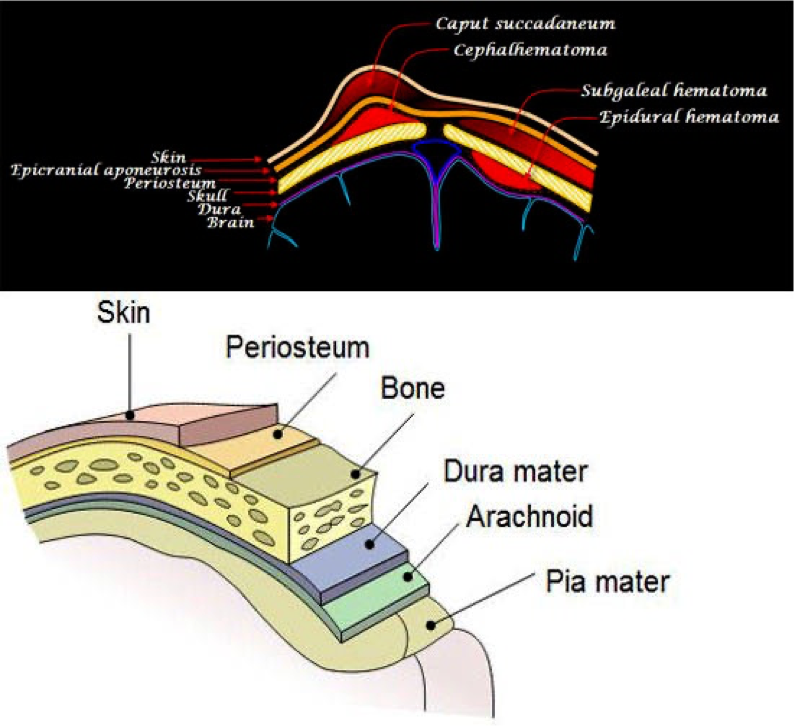
I. Extracranial Injuries
-
Cephalhematoma
- It is a sub-periosteal hemorrhage, thus it is limited to the borders of a cranial bone (usually parietal).
- There is no discoloration of the overlying scalp.
- It begins to appear after several hours because sub-periosteal bleeding is a slow process.
- In some cases, there is an underlying linear fracture (detected by X-ray).
- It resolves gradually and usually leaves an elevated edge.
Complications:
- Anemia (blood loss).
- Hyperbilirubinemia (resorption of the hematoma) may occur with large cephalhematomas.
- Infection may occur if aspiration is done.
Management:
- Usual management is mainly observation (Do not aspirate).
- Phototherapy may be necessary if blood accumulation is significant leading to jaundice.
- Rarely anemia can develop needing blood transfusion.
- The presence of a bleeding disorder should be considered but is rare.
- Skull radiography or CT scanning is also used if concomitant depressed skull fracture is a possibility.
Differential Diagnosis:
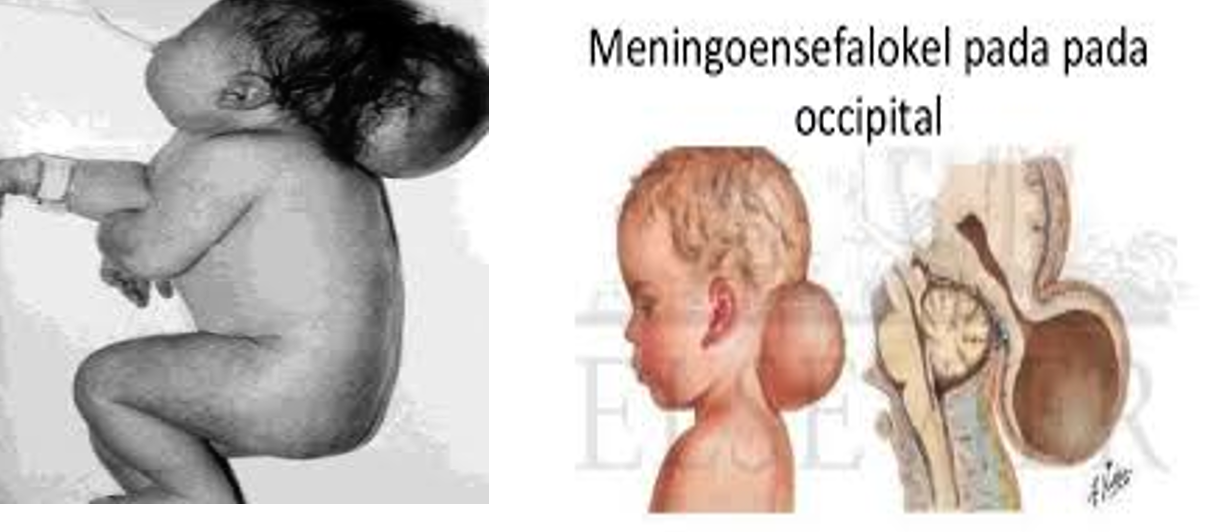
- It should be differentiated from:
- Caput succedaneum.
- Meningocele (pulsating, increases with crying, x-ray shows a bone defect).
- Subaponeurotic hemorrhage.
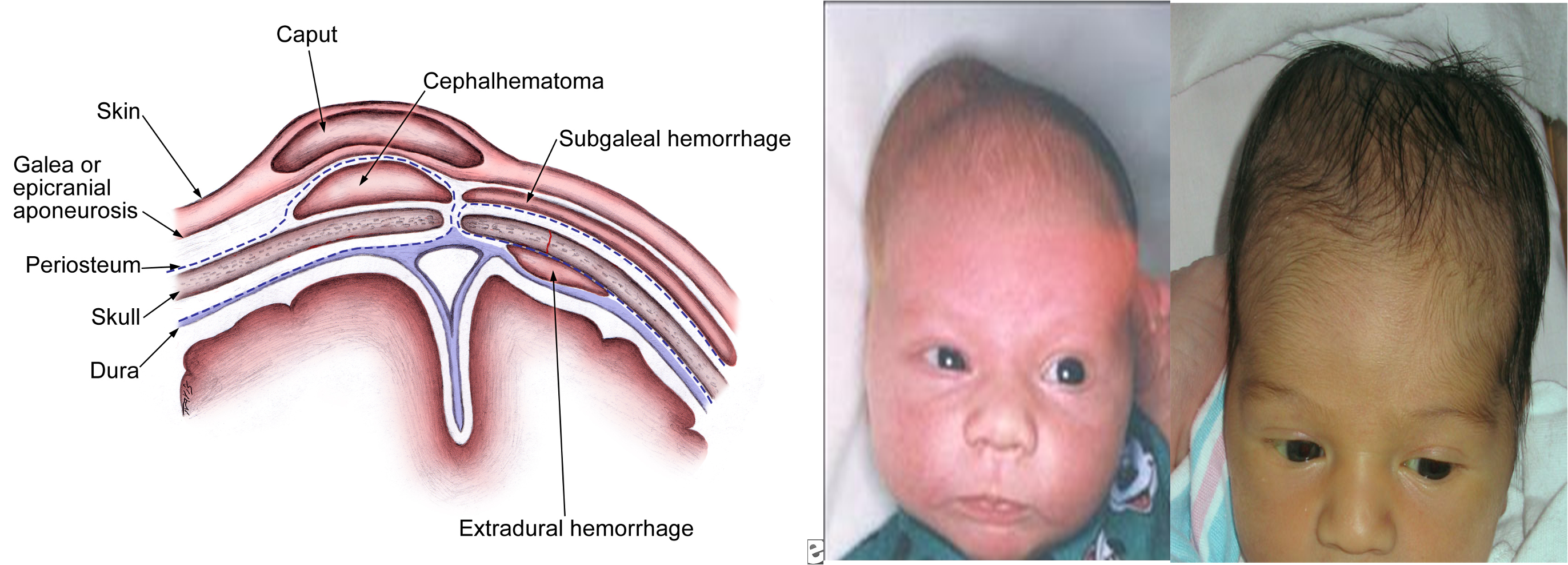
- Caput Succedaneum
- This is a diffuse edematous swelling of the scalp, presents at birth, not limited to a bone which resolves in a few days.
| CAPUT SUCCEDANEUM | CEPHALHEMATOMA |
|---|---|
| 1. Present at birth on normal vaginal delivery. | 1. Appears within a few days after birth on normal or forceps delivery. |
| 2. May lie on sutures, not well defined. | 2. Well defined by suture, gradually developing, hard edge. |
| 3. Soft, pits on pressure. | 3. soft, elastic but does not pit on pressure. |
| 4. Skin ecchymotic. | 4. No skin change. |
| 5. Size largest at birth, gradually subsides within a day. | 5. Becomes largest after birth and then disappears within 6-8 weeks to few months. |
| 6. No underlying skull bone fracture. | 6. May have underlying skull bone fracture. |
| 7. No treatment required. | 7. No treatment required. |
 |
Caput Succedaneum
 It is a localized swelling or edema which is commonly present on the head of newborn following vaginal delivery. It shows soft pitting when pressure is applied.
It is a localized swelling or edema which is commonly present on the head of newborn following vaginal delivery. It shows soft pitting when pressure is applied.
- Subaponeurotic Hemorrhage
- The whole scalp is swollen and boggy with bluish discoloration.
- Hemorrhage is in the loose areolar area (under the aponeurosis) i.e., not limited to bone.
- Clinical picture of shock may be present.
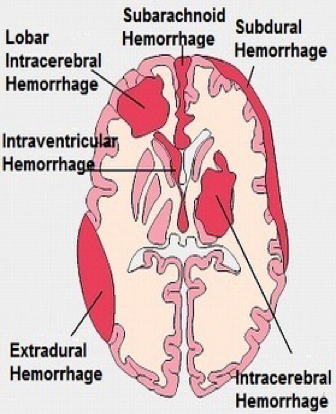
II. Intracranial Hemorrhage
Definition:
Hemorrhage inside the cranial cavity.
Types:
- Outside the brain (epidural, subdural, subarachnoid).
- In the brain ventricles (interventricular).
- In the brain parenchyma (e.g., intracerebral).
The Most Common:
- In preterm → interventricular.
- In full-term → subarachnoid and intracerebral.
Important Causes:
- Instrumental delivery.
- Hypoxia (perinatal, hyaline membrane disease).
- Spontaneous in extreme prematurity.
- Bleeding tendency is a rare cause.
Clinical Manifestations:
-
Pallor, cyanosis with irregular breathing, later on jaundice (resorption of concealed blood).
-
Lethargy, poor Moro reflex, weak suckling.
-
High pitched cry.
-
Convulsions, usually tonic.
-
Tense bulging anterior fontanel.
-
Localizing neurological deficits may occur like ocular palsies, and unequal pupils.
-
N.B. Triad of pallor, high-pitched cry, tense bulging ant. fontanel you should suspect intracranial hemorrhage.
Diagnosis:
- Beside the history and clinical picture:
- Cranial ultrasonography is very useful and as sensitive as the CT scan.
- A hemorrhagic CSF occurs in subarachnoid hemorrhage.
Complications:
- Death from respiratory failure.
- Obstructive hydrocephalus.
- Cerebral palsy.
Prevention:
- Good maternal and obstetric care.
Treatment: The treatment is a symptomatic one:
- Vitamin K to help coagulation.
- Ventilatory support (if there is respiratory difficulty).
- Phenobarbitone (if there are convulsions).
- Blood transfusion (if there is anemia).
- Treatment of complications like hydrocephalus.