Internal Medicine
Congestive Heart Failure
Dr Waqar
DEFINITION
IT IS A CONDITION IN WHICH THE HEART CAN NOT PUMP ENOUGH BLOOD TO THE PERIPHERAL TISSUES
ETIOLOGIES
Common:
- Ischemic heart disease (most common cause)
- HTN also very common
- DM and Obesity also very common
- Cardiomyopathies
B) Other causes:
- Valvular diseases (stenosis or regurgitation)
- Drugs (some chemo. agents)
- Alcohol
- Congenital heart diseases (ASD, VSD)
SOME IMPORTANT DEFINITIONS
-
End diastolic vol.: Amount of blood in the ventricle at the end of diastole (after all the blood has come from the atrium)
-
Stroke vol.: Amount of blood pumped out with each heartbeat.
-
Cardiac output: Amount of blood pumped in 1 min. (stroke vol. x heart rate) N: 5-6 L
-
Ejection Fraction(EF): “Percentage” of end-diastolic vol. which is pumped out (stroke vol expressed as a %) E.F. VALUES:
- Normal: 50-75%
- Borderline: 40-50%
- Low: less than 40%
( E.F. = Stroke volume X 100 / End diast vol)
Pathogenesis
In CHF, stroke volume (blood pumped with each beat) is reduced, so cardiac output is low, leading to tissue hypo-perfusion. Hypoperfusion results in compensatory mechanisms by the body:
- Sympathetic stimulation, and tachycardia
- Systemic vasoconstriction
- Activation RAS of renin-aldosterone secretion & salt/water retention by kidneys -⇒ edema
TYPES OF HEART FAILURE
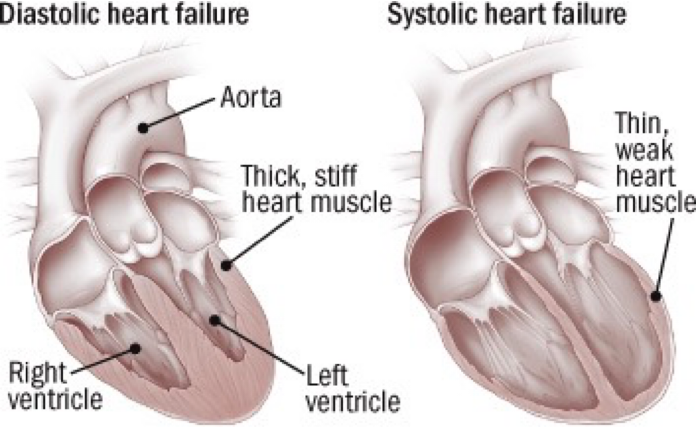
A) Based on what is abnormal: systole or diastole:
-
Systolic heart failure
(poor contraction) equal prevalence -
Diastolic heart failure
(poor relaxation) equal prevalence
B) Based on which part of the heart is affected:
-
Pure left ventricular failure (common)
-
Pure right ventricular failure (uncommon)
-
Bi-ventricular failure (common)
S/S of CHF
Patient’s Complaints:
- Dyspnea
- Orthopnea; dyspnea on lying down
- Paroxysmal nocturnal dyspnea
- Fatigue
- Exercise intolerance
- Palpitations
- Ankle swelling
- Cough (dry)
On Examination:
- Lung crackles on auscultation (pulmonary edema) (not in pure right HF)
- Tachycardia
- Cardiomegaly (in systolic heart failure)
- 3rd & 4th heart sounds)
- Raised JVP
- Pedal edema
- Hepatomegaly +/- ascites (not in pure left HF)
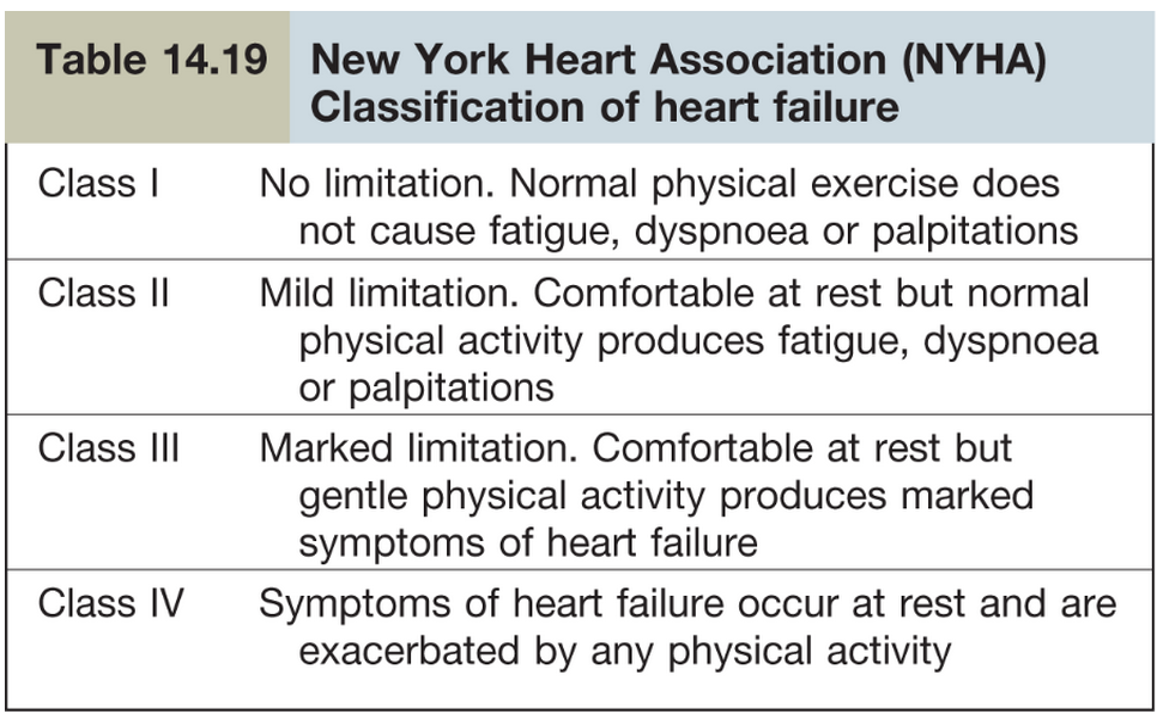
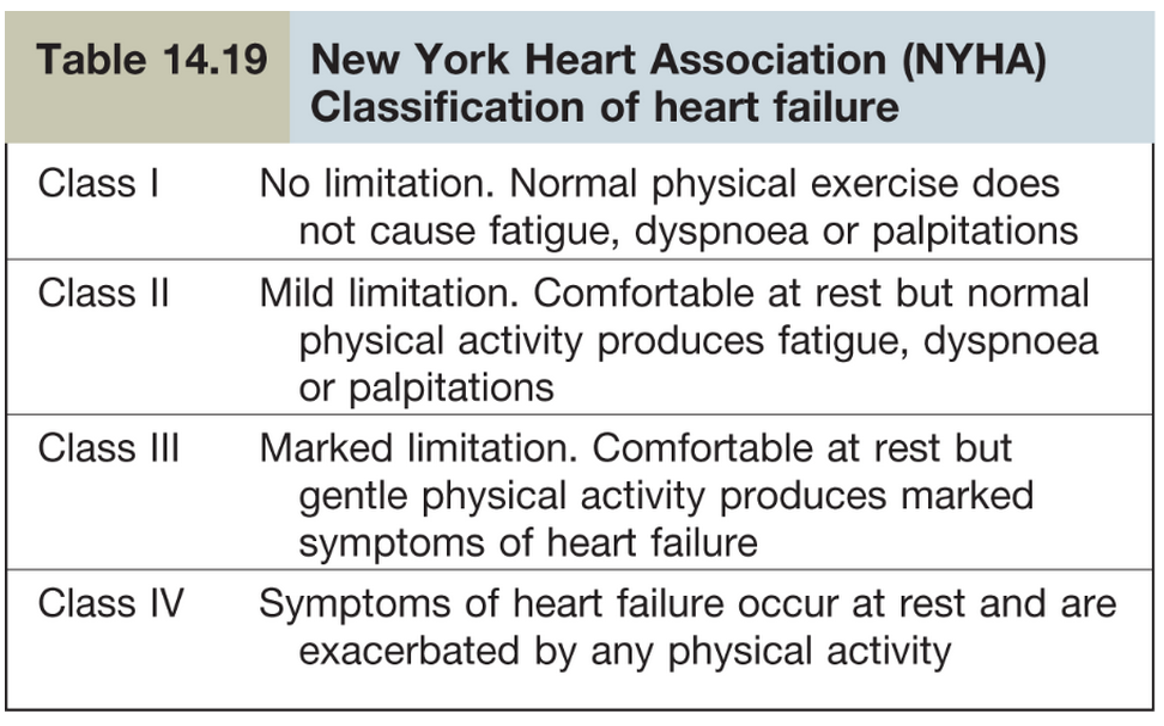
Functional classification of CHF
Investigation, Management, and treatment
-
Investigation of Congestive Heart Failure
-
Congestive heart failure Management & Treatment
-
Pulmonary Edema management and treatment
CASE
A 50-year-old male has a history of HTN, DM, and aortic stenosis. He complains of gradually worsening dyspnea since 2 months. He uses 2 pillows during sleep. His symptoms have gradually worsened and now even less than normal physical activity causes dyspnea. 2D echo and chest X-ray show congestive heart failure. What should be the management for him? 1- Life style management / Treat underlying conditions 2- Diuretics, Oxygen therapy, ACE, BB for long term
RAPID FIRE QUESTIONS
- How many types of heart failure are there based on ejection fraction? systolic diastolic
- Pure right-sided heart failure is common. Right or wrong? wrong
- What is the commonest cause of heart failure? ischemic, htn
- Name some other causes? htn dm valvular
- What is stroke vol? each beat amount blood
- What is ejection fraction? %
- What is the normal value of ejection fraction? >50-75%
- What are the patient’s complaints in heart failure? sob, dyspnea, orthopnea, fatigue, exercise intolerance
- What are the auscultatory findings in the lungs in CHF? crackles
- Which abnormal heart sounds can be heard? s3 & s4 gallop
- Which 2 systems are overactive in CHF, as a compensation? sympathetic & RAS
- What’s the name of the Functional Classification of CHF? NY heart association
- Name some causes of right heart failure? left sided HF, pulm HTN infacrtion Right Ventricle
- Name 3 chest X-ray findings in CHF? pleural effusion, pulmonary edema, karley b lines batwing
- Is cardiomegaly always MOJOOD on chest X-ray? no in diastolic
- Which is the diagnostic test for CHF? echo
- What is the specific ECG finding of CHF? no specific
- Commonest presentation of CHF is chest pain, right or wrong? wrong, usually its mi
- Dyspnea due to CHF or dyspnea due to other causes, how to know? serum BNP levels
- Name some lifestyle/dietary steps to take in CHF treatment? no smoke alcohol low salt
- Which 3 groups of drugs should be given to all CHF patients? ace, bb, diuretics
- Which drug to add in severe CHF? spironolactone
- Is digoxin used routinely? no
- ACE is better or ARB? ace
- Mode of action of ACE? block ras
- Contraindications of ACE & ARBs? angioedema, pregnancy, bilateral venous artery stenosis
- What to use if ACE or ARBs cannot be used? nitrates,…
- Which beta blockers to use? … specific b1
- Patient comes in acute CHF, not on any meds. What will you give? ?
- Name 3 things that can precipitate acute pulmonary edema in a CHF patient? excess fluid, HTN, Ischemia
- Patient in acute pulm edema. Name 4 things you will give?position, o2, lasix, iv nitrates
THERAPEUTICS
It is a condition in which the heart can not pump enough blood to the peripheral tissues
ETIOLOGIES
DM & OBESITY ARE VERY HIGH RISK FACTORS FOR CHF
A) Common:
- Coronary artery disease( most common)
- HTN
- Cardiomyopathies
B) Other causes:
- Valvular diseases (stenosis or regurgitation)
- Drugs ( some chemo. agents)
- Alcohol
- Congenital heart diseases (ASD, VSD)
DEFINITIONS
- End diastolic vol.: amount of blood in the ventricle at the end of diastole (after all the blood has come from the atrium)
- Stroke vol.: amount of blood pumped out with each heart beat.
- Cardiac output: amount of blood pumped in 1 min.( stroke vol. x heart rate) N: 5-6 L
- Ejection Fraction(EF): “percentage”of end diastolic vol. which is pumped out (stroke vol expressed as a %)
E.F. VALUES:
- Normal: 50-75%
- Borderline : 40-50%
- Low : less than 40% ( E.F. = (Stroke volume/End diast vol) X 100
TYPES OF HEART FAILURE
A) Based on which part of the heart is affected:
- [Pure left ventricular failure]
- Pure right ventricular failure (uncommon)
- Bi-ventricular failure (common)
B) Based on what is abnormal: systole or Diastole
- Systolic heart failure
- Diastolic heart failure
(Equal/Prevalence)
Pathogenesis
In CHF, stroke volume(blood pumped with each beat) is reduced, so cardiac output is low ⇒ tissue hypoperfusion.
Hypoperfusion results in compensatory mechanisms by the body:
- Sympathetic stimulation, and tachycardia
- Systemic vasoconstriction
- Activation of renin-aldosterone secretion & salt /water retention by kidneys ⇒ edema
Symptoms and signs
- Dyspnea
- Orthopnea
- Paroxysmal nocturnal dyspnea
- Fatigue
- Exercise intolerance
- Palpitations
- Ankle swelling
- Cough(dry)
On Examination
- Lung crackles on auscultation(pulm. edema) ( not in pure right HF)
- Tachycardia
- Cardiomegaly (how to find out?)
- 3rd & 4th heart sounds)
- Raised JVP
- Pedal edema
- Hepatomegaly +/- ascites(not in pure left HF)
Functional classification of CHF