Case Scenario
A 32-year-old G0P0 presents to the infertility clinic with a 3-year history of infertility. She states that her menses began at age 13 and occurs on regular 28-day intervals. She complains of severe monthly pain 1 week before each menses and pain with intercourse. She denies a history of sexually transmitted diseases. Her husband has a child from a previous marriage. On rectovaginal exam, she has uterosacral nodularity and a fixed, retroflexed uterus.
- What diagnostic test would be the most appropriate at this point to make the diagnosis? Laparoscopy and send it to Pathology Lab
- What findings would you see on a tissue biopsy?
Definition
-
Endometriosis is defined as the extrauterine presence of functioning endometrial glands and stroma.
-
Estrogen stimulates the growth of endometriotic implants similar to its effect on normal endometrial tissue.
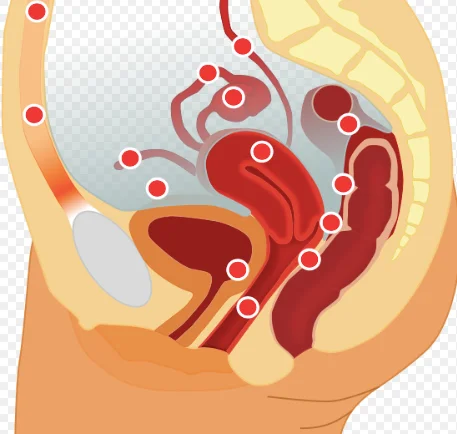
Sites of Endometriosis
Common
- Ovary : 60%.
- posterior cul-de-sacs.
- vesicouterine space
- Peritoneum over uterus.
- Broad ligaments/fallopian tubes/round ligaments.
- Uterosacral ligaments.
- Bowel.
- Pelvic lymph nodes
Less Common
- -laparotomy and episiotomy scars.
- -appendix
- -pleural, and pericardial cavities
- -cervix.
Sites
Etiology
- Theories of the Pathogenesis of Endometriosis
- The etiology of endometriosis is unknown. Several theories have been postulated:
- Retrograde menstruation.
- Immunologic factors
- Inflammatory factors
- Hormonal factors
- Coelomic metaplasia
- Lymphatic spread
- Genetic factors
Patient Characteristics
-
Mean age at diagnosis is 25 to 30 years. The greatest incidence has been observed in nulliparous women with early age at menarche and shorter menstrual cycles.
-
Rare in multiparous because most of them came with infertility.
Clinical Presentation
- Up to one-third of women may be asymptomatic
- Pelvic pain (that is especially worse during menses, but can be chronic): * Secondary dysmenorrhea (pain begins up to 48 hr prior to menses). * Dyspareunia (painful intercourse) as a result of implants on pouch of Douglas; occurs commonly, with deep penetration. * Dyschezia (pain with defecation): Implants on rectosigmoid. * Dysuria: implant in urinary system. * Infertility. Z
- Intermenstrual bleeding.
- Cyclic bowel or bladder symptoms (hematuria).
The most common symptoms are infertility and pelvic pain.
Abnormal Clinical Findings Associated with Endometriosis
- Nodularity of the uterosacral ligaments, which are often tender and enlarged
- Painful swelling of the rectovaginal septum
- Pain with motion of the uterus and adnexa
- Fixed retroverted uterus and large immobile adnexa are indicative of severe pelvic disease.
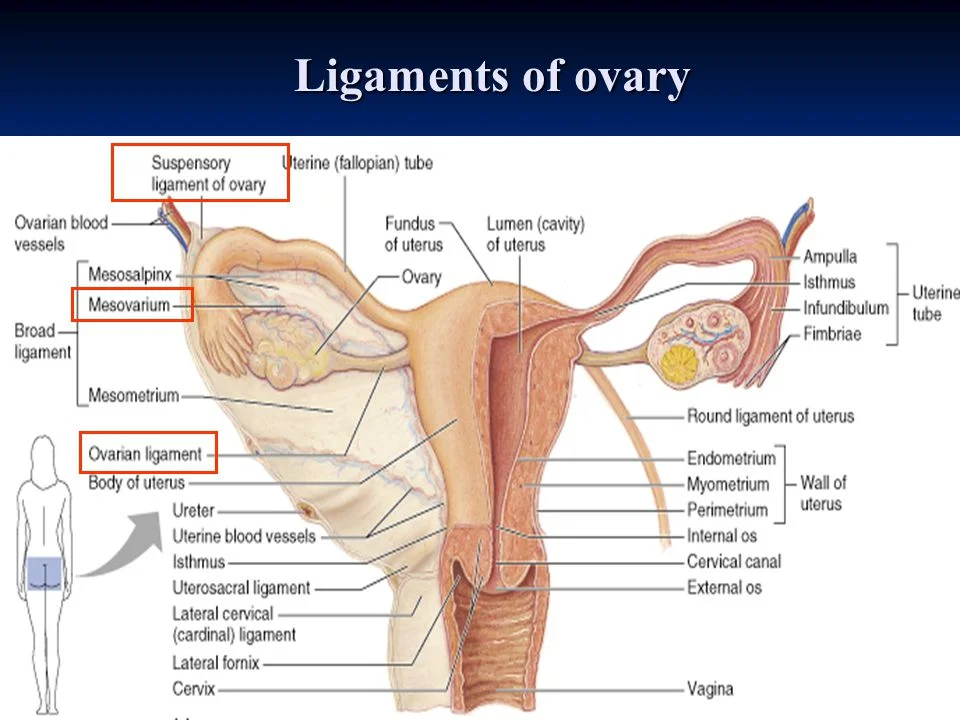
Ligaments of Ovary
Diagnosis
- Experienced clinicians often presumptively diagnose endometriosis based on clinical history and timing of symptoms.
- Pelvic ultrasonography can be useful in differentiating the presence of endometriomas (CHOCOLATE CYST) from other adnexal masses.
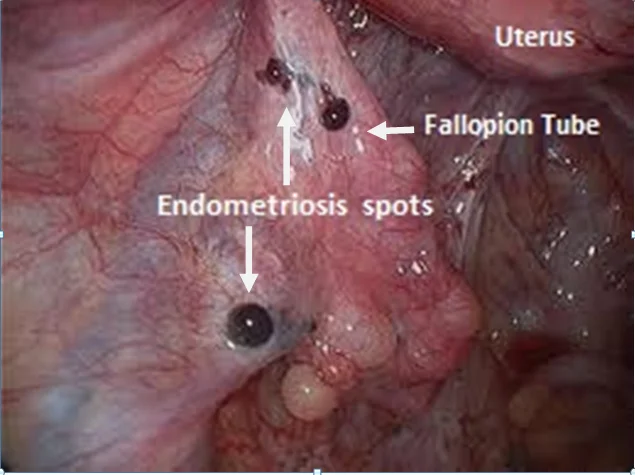
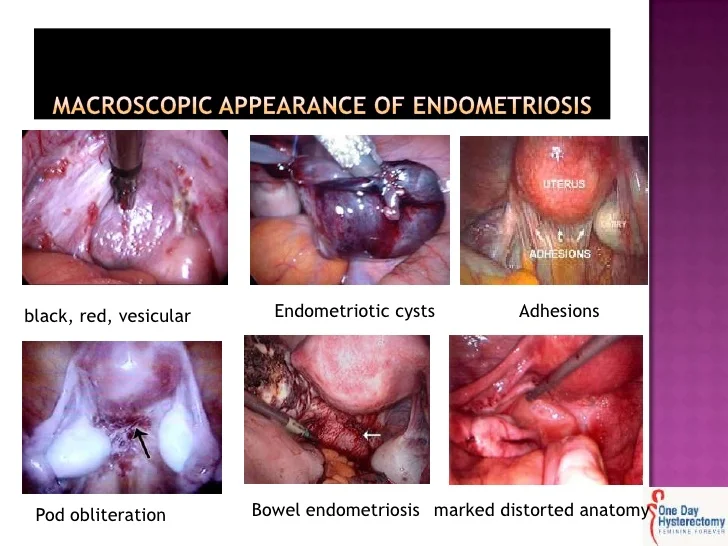
- Diagnostic laparoscopy (gold standard) a marked discrepancy in appearance of the endometriotic lesions: a. classically appear as blue-black powder-burn. b. Nonclassic lesions may appear vesicular, red, white, tan, or nonpigmented. The presence of defects in the peritoneum (usually scarring overlying endometrial implants) is known as Allen-Masters syndrome. c. Endometriomas, “chocolate cysts,” appear filled with dark brown blood.
Laparoscopic Findings
 Choclate cysts
Choclate cysts
Macroscopic Appearance of Endometriosis
Definitive Diagnosis Z
-
Histology and examination of lesions removed at the time of surgery.
-
Histology reveals both endometrial glands and stroma containing Hemosiderin-laden macrophages.
Management
Medical Treatment
-
Pain control with nonsteroidal anti-inflammatory drugs (NSAIDs) inhibits prostaglandin production by ectopic endometrium, good first-line agent.
-
Medical therapy is aimed at suppressing ovarian estrogen stimulation (induce amenorrhea) and cause regression of the endometriotic implants.
-
Oral contraceptive pills (OCPs):
- cause anovulation and atrophy of endometrial tissue.
- Symptomatic relief of pelvic pain and dysmenorrhea is reported in 60% to 95% of patients.
-
Gonadotropin-releasing hormone (GnRH) agonists: when given over the longterm suppress pituitary function by downregulating pituitary GnRH receptors. Induce “pseudomenopause.”
- e.g leuprolide acetate injection every month for 6 months only.
- Side effects: use of a 6-months course to avoid the long-term consequences of the hypoestrogenic state on bone metabolism, vasomotor symptoms and lipid profile changes.
-
Add-back therapy : combined estrogen/progesterone Is largely used for minimization of side effect of GnRH.
-
Progestins: Progestins inhibit ovulation by luteinizing hormone (LH) suppression.
-
Danazol (Danocrine) a testosterone derivative. It suppresses the midcycle LH surge
- Androgenic side effects.
-
Aromatase inhibitors
-
Surgical Treatment
-
Conservative surgery:
- For patients with endometriosis-related pain but who desire future fertility.
- With laparoscopic excision or destruction of endometrial implants
-
A “semidefinitive” procedure that preserves an uninvolved ovary to avoid the long-term risks of surgical menopause.
-
Definitive surgery entails total abdominal hysterectomy with bilateral salpingooophorectomy, excision of peritoneal surface lesions or endometriomas, and lysis of adhesions.
Hormone replacement therapy (HRT) after definitive surgery for the prevention of surgical menopausal symptoms
Endometriosis and Ovarian Malignancy
- INCIDENCE :0.3% to 0.8% of patients with endometriosis. will get ovarian malignancy
- TYPE : Clear cell and endometrioid carcinoma