Process
•Before starting •Introduce yourself to the patient. •Confirm his name and date of birth. •Explain that you are going to ask him some questions to uncover the nature of his chest pain and obtain his consent. •Ensure that he is comfortable
1) Presenting complaint (PC)
- •Chest pain
- •Breathlessness (dyspnoea)
- •Palpitation
- •Dizziness
- •Blackouts (syncope)
- •Lower limb swelling
- •Intermittent claudication
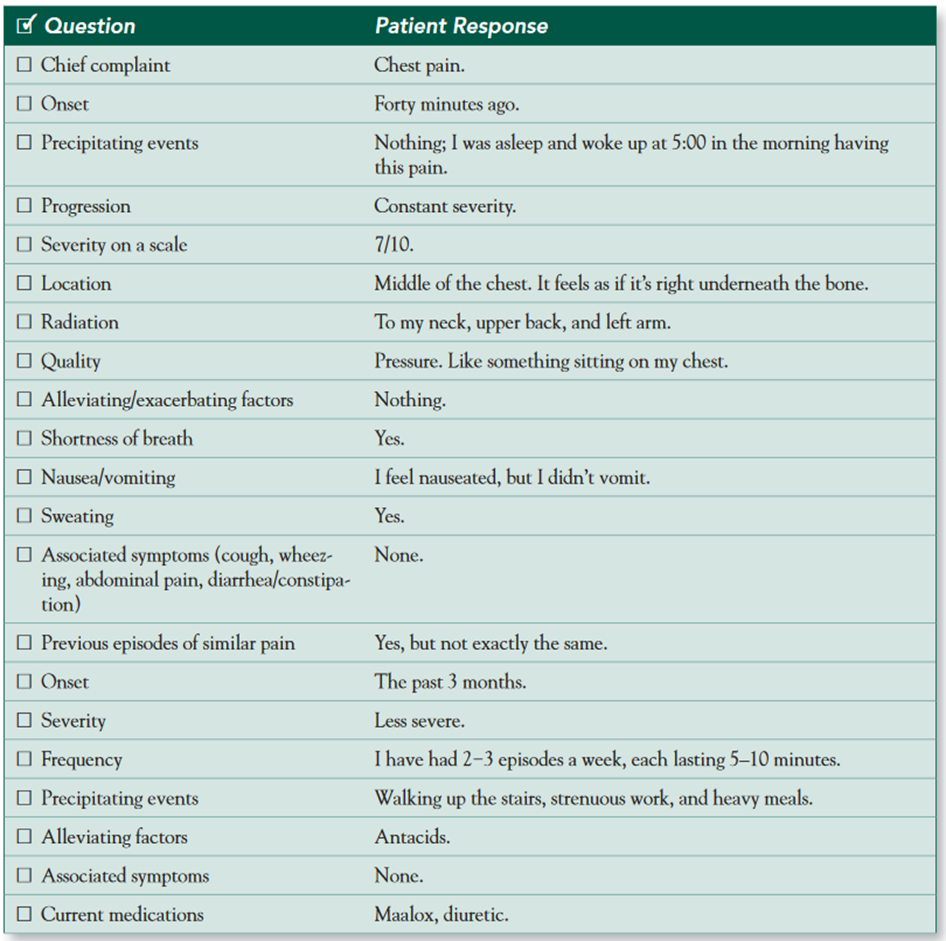
2) History of presenting complaint (HPC)
As with any pain history, the mnemonic SOCRATES can help develop your differential diagnosis:
- Site: where exactly is the pain?
- Onset and progression: when did the pain start and how has it changed or evolved?
- Character: what type of pain is it (dull, sharp, or crushing)?
- Radiation: does the pain move anywhere (into the jaw, arm, or back)?
- Associated S&S: ask about sweating, N and V, SOB, cough, haemoptysis, dizziness, & palpitations
- Timing and duration: does the pain occur at particular times of the day? How long does each episode last?
- Exacerbating and alleviating factors: what make the pain better or worse (exercise, movement, deep breathing, coughing, cold air, large or spicy meals, alcohol, rest, GTN, sitting up in bed)?
- Severity: “How would you rate the pain on a scale of 1 to 10, & effect on everyday life.
Ask about any previous episodes of chest pain.
Other symptoms of CVS
-
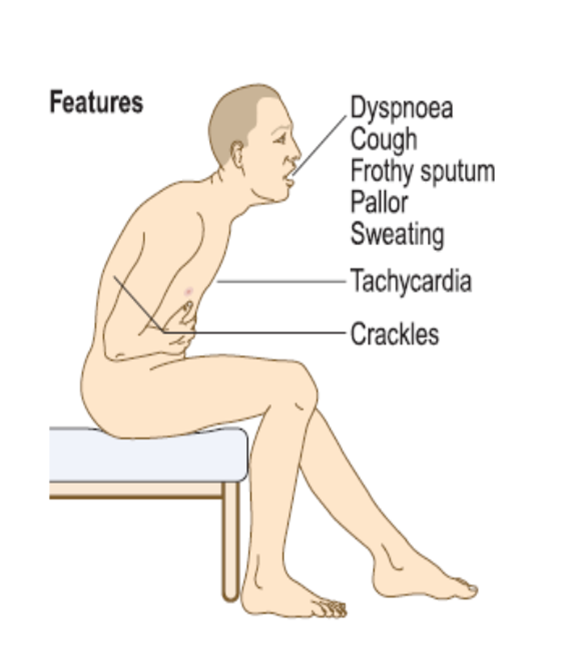
Breathlessness: orthopnoea, paroxysmal nocturnal dyspnoea, ankle swelling, cough, wheeze, haemoptysis?
-
Palpitation: sudden onset and offset, ‘thumps’ or ‘pauses’, presyncope or syncope?, Fatigue
-
Dizziness/syncope: provoking factors, warning, duration, recovery?
Infective endocarditis, : non-specific symptoms, including weight loss, tiredness, fever and night sweats.
Embolisation of intracardiac thrombus, tumour (such as atrial myxoma) or infective ‘vegetations’ symptoms of stroke , acute limb ischaemia or acute mesenteric ischaemia.
Advanced heart failure: abdominal distension due to ascites, or weight loss and muscle wasting (‘cardiac cachexia’) due to a prolonged catabolic state.
 Risk factors of cardiovascular disease
Risk factors of cardiovascular disease
- Coronary heart disease ( myocardial infarction)
- Stroke
- Pneumonia
- Pulmonary embolism
- Deep vein thrombosis
- Hypertension
- Hyperlipidaemia
- Diabetes
- Smoking, alcohol use, and recent long-haul travel.
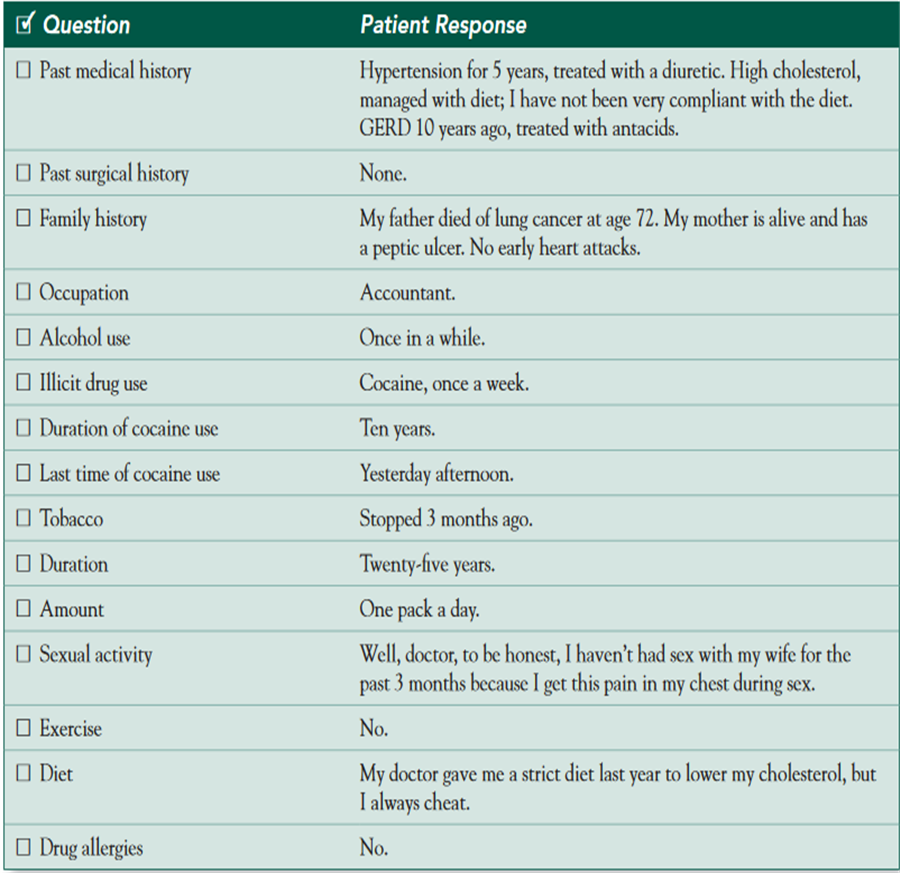
3) Past medical history (PMH)
- Current, past, and childhood illnesses.
- Stroke or transient ischaemic attack (TIA),
- Renal impairment,
- rheumatic fever, heart murmur
- Peripheral vascular disease
- Systemic disorders (pericarditis and Raynaud’s
- Marfan’s syndrome (aortic dissection)
- myotonic dystrophy (atrioventricular block).
- Operations, hospital clinic attendances
• potential causes of bacteraemia in patients with suspected infective endocarditis, such as skin infection, recent dental work, intravenous drug use or penetrating trauma
• systemic disorders with cardiovascular manifestations such as connective tissue diseases (pericarditis and Raynaud’s phenomenon), Marfan’s syndrome (aortic dissection) and myotonic dystrophy (atrioventricular block).
4) Family history
- Parents, siblings, and children.
- Ask specifically
- Heart disease
- Hypertension,
- other heritable cardiovascular risk factors
- Sudden death
5) Drug history
- Current, compliance with treatment
- Prescribed medication, including the oral contraceptive pill if female.
- Over-the-counter medication.
- Recreational drugs.
- Allergies.
6) Social history
- Effect of the chest pain on the patient’s life:
- Employment.
- Housing.
- Hobbies.
- Smoking
- Alcohol
- Recreational drugs such as cocaine and amphetamines
Smoking is the strongest risk factor for coronary and peripheral arterial disease. Take a detailed smoking history (p. 14). Alcohol can induce atrial fibrillation and, in excess, is associated with obesity, hypertension and dilated cardiomyopathy. Recreational drugs such as cocaine and amphetamines can cause arrhythmias,
After taking the history
- Ask the patient if there is anything else that he might add that you have forgotten to ask.
- Summarize your findings and offer a differential diagnosis.
- Thank the patient
- State that you would like to examine the patient and order some investigations,
- for example, ECG and chest X-ray, to confirm your diagnosis
What is your diagnosis?
Mr. Short, the source of your pain can be a cardiac problem such as a heart attack or angina, or it may be due to acid reflux, lung problems, or disorders related to the large blood vessels in your chest. It is crucial that we perform some tests to identify the source of your problem. We will start with an ECG and some blood work, but more complex tests may be needed as well. Do you have any questions for me?
References
Macleod’s Clinical Examination : 15 edition Page 43-50
Nicholas J Talley: clinical examination. A systematic guide to physical diagnosis 8th edition: 57- 108
HUTCHISON’S CLINICAL METHODS . Page 189-194