Acute Pancreatitis
most common due to alcohol - clinical presentation with epigastric pain - radiation to the back - following by vomiting, fever. High C- amylase labarotary investigation
Acute pancreatitis causes abdominal pain, fever, vomiting and leucocytosis, together with elevation of the serum amylase.
sentinal loops; dilated bowel not due obstruction but due infllamation of pancreas mediators - may happen in appendicitis, peritonitis - generally any inflammation in the gastric
CT and ultrasound findings:
-
The pancreas is usually enlarged, often diffusely, and may show irregularity of its outline.
-
There may be low density areas at CT and echo-poor areas at sonography, representing oedema.
-
Peripancreatic fluid and/or ascites.
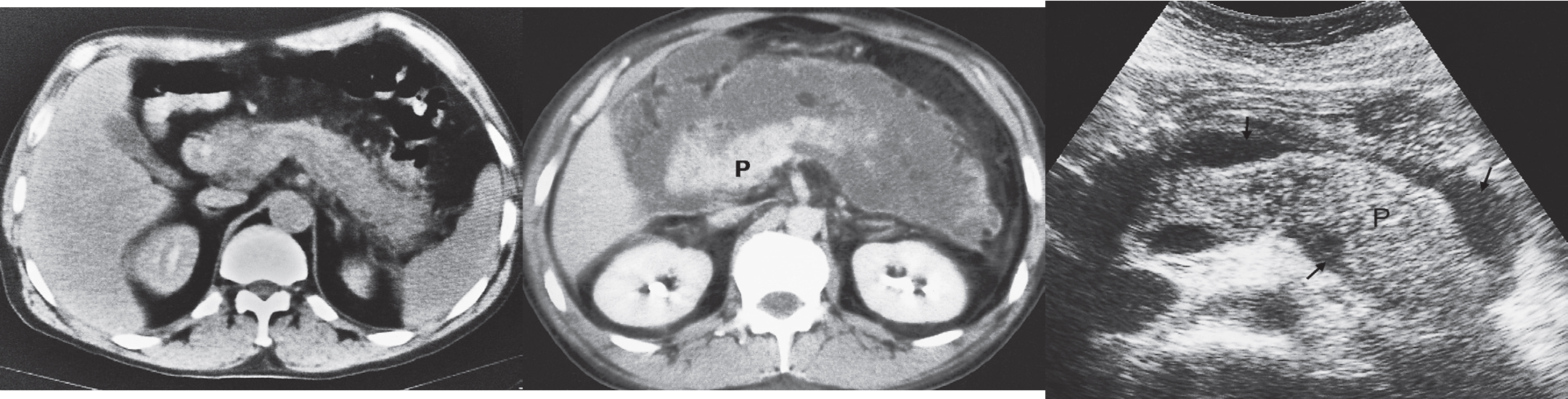
- (a) CT scan showing diffuse enlargement of pancreas w/ ill-defined edges.
- (b) CT scan showing considerable inflammation around the pancreas (P).
- (c) Transverse ultrasound scan showing a swollen pancreas (P) with some fluid around the pancreas. defined margins, irregular, bulky
Chronic Pancreatitis
Chronic pancreatitis results in calcifications; calcifications in chronic pancreatitis are often recognizable on plain films and ultrasound, but are particularly obvious at CT. - The pancreas may atrophy focally or generally.
(A) Within the body of pancreas, the main pancreatic duct shows alternating segments of dilatation and stenosis. There is atrophy of the pancreatic parenchyma, and a few punctate calcifications are seen.
The CT features are compatible with a diagnosis of chronic pancreatitis.

-
(B) CT scan showing numerous small areas of calcification within the pancreas (arrows).
-
(C) MRCP showing a normal biliary duct system but irregular dilatation of the pancreatic duct (arrows).
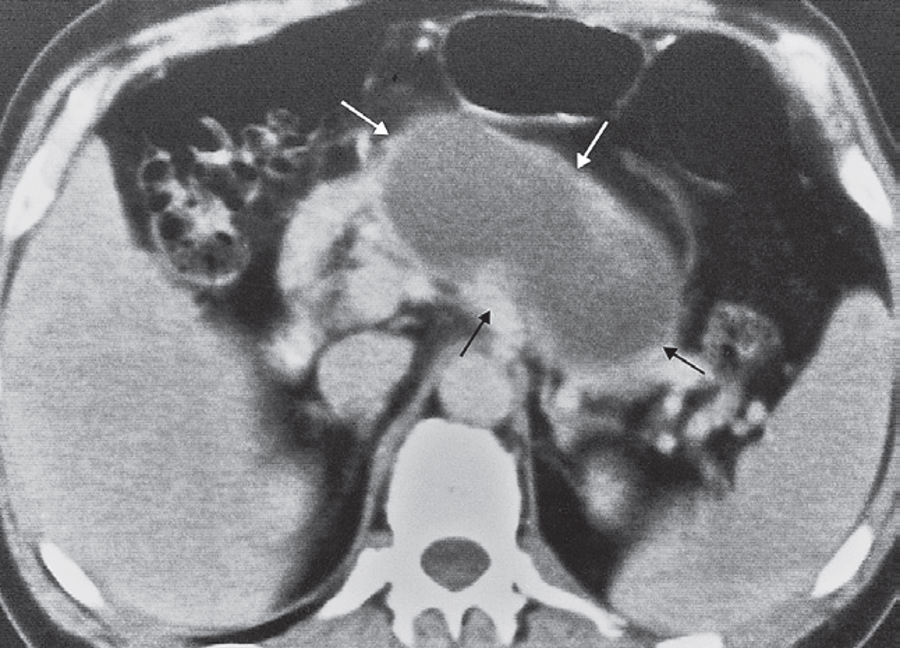
Pancreatic pseudocyst
CT scan showing a large cyst; fluid density arising within the pancreas (arrows).
Trauma to the pancreas is uncommon but serious. Injuries to other structures are frequent, so CT is the best method of investigation.