Knee Examination
Introduction & Preparation
- Introduction:
- Introduce yourself (e.g., “Hello, I’m khalid, a medical student”).
- Confirm the patient’s details (Name, age).
- Wash hands/use alcohol rub (before and after examination).
- Ensure privacy and take consent.
- Briefly explain the purpose and procedure of the examination (e.g., “I need to examine your knee. This will involve looking at it, feeling it, moving it, and doing some special tests. Is that okay?”).
- Inquire about any pain before starting.
- Ask the patient to undress appropriately, exposing both knees fully (up to the groin if necessary, typically shorts are sufficient).
- Positioning: The examination will involve the patient standing, sitting, and lying supine.
- General Assessment: Note the patient’s general appearance, vital signs, and BMI.
History Taking Y
- Establish Rapport: Use communication skills effectively.
- Chief Complaint: “What brings you today?”
- Onset, duration, timing, character, localization, radiation, frequency, severity.
- Precipitating factors (e.g., trauma, mechanism of injury) and relieving factors.
- Functional limitations.
- Associated symptoms: Swelling, morning stiffness, giving way, knee locking, clicking feeling, fever, unexplained weight loss.
- Specific Enquiries (if suspecting arthritis):
- Involvement of other joints and signs of inflammation.
- Systemic symptoms (skin, chest, abdominal, urinary).
- Past Medical History:
- Previous trauma (especially to the knee) or surgical interventions.
- History of chronic diseases (e.g., Gout, RA, SLE, OA, DM).
- Drug history/allergies (e.g., corticosteroids).
- Family History: Any family members with similar symptoms or relevant conditions?
- Social History:
- Occupational history (e.g., heavy workloads, frequent squatting/kneeling).
- Lifestyle (e.g., sports activity, smoking, diet, physical activity).
- Psychosocial: Assess Ideas, Concerns, Expectations (ICE), mood (depression), effect of the condition on life.
- Review Previous Investigations: Ask if any tests have been done already.
- Summarize: Briefly summarize the history and ask “Anything you want to add?”
Examination
Inspection (Look)
- Standing:
- Gait: Assess for limp, asymmetry, antalgic gait.
- Alignment/Deformity: Look for Varus (bow-legged) or Valgus (knock-kneed) deformities. Compare both sides.
- Muscle Bulk: Note quadriceps muscle bulk/atrophy. Measure quadriceps circumference (e.g., 15-20 cm above the tibial tubercle) if asymmetry is suspected.
- Supine:
- Compare both knees.
- Skin: Look for scars, redness (erythema), rashes, bruising, discoloration, lacerations.
- Swelling: Note any joint effusion or localized swelling.
- Deformity: Gross deformities, asymmetry of bony or soft tissue landmarks.
- Muscle Wasting: Particularly quadriceps.
- Popliteal Fossa: Inspect for swelling (e.g., Baker’s cyst).
Palpation (Feel)
- Ask about pain before touching.
- Temperature: Assess skin temperature using the back of your hand, comparing both knees and surrounding areas.
- Tenderness: Palpate systematically for pain/tenderness over:
- Quadriceps muscle and tendon.
- Patella (facets, borders) and patellar tendon.
- Tibial tubercle.
- Joint line (medial and lateral).
- Medial Collateral Ligament (MCL) origin and insertion.
- Lateral Collateral Ligament (LCL) origin and insertion.
- Hamstring tendons.
- Head of fibula.
- Surrounding bursae (prepatellar, infrapatellar, pes anserine).
- Effusion:
- Bulge/Sweep Test: For minimal effusion. Stroke upwards on the medial side to milk fluid into the suprapatellar pouch, then stroke downwards on the lateral side and watch for a fluid bulge medially.
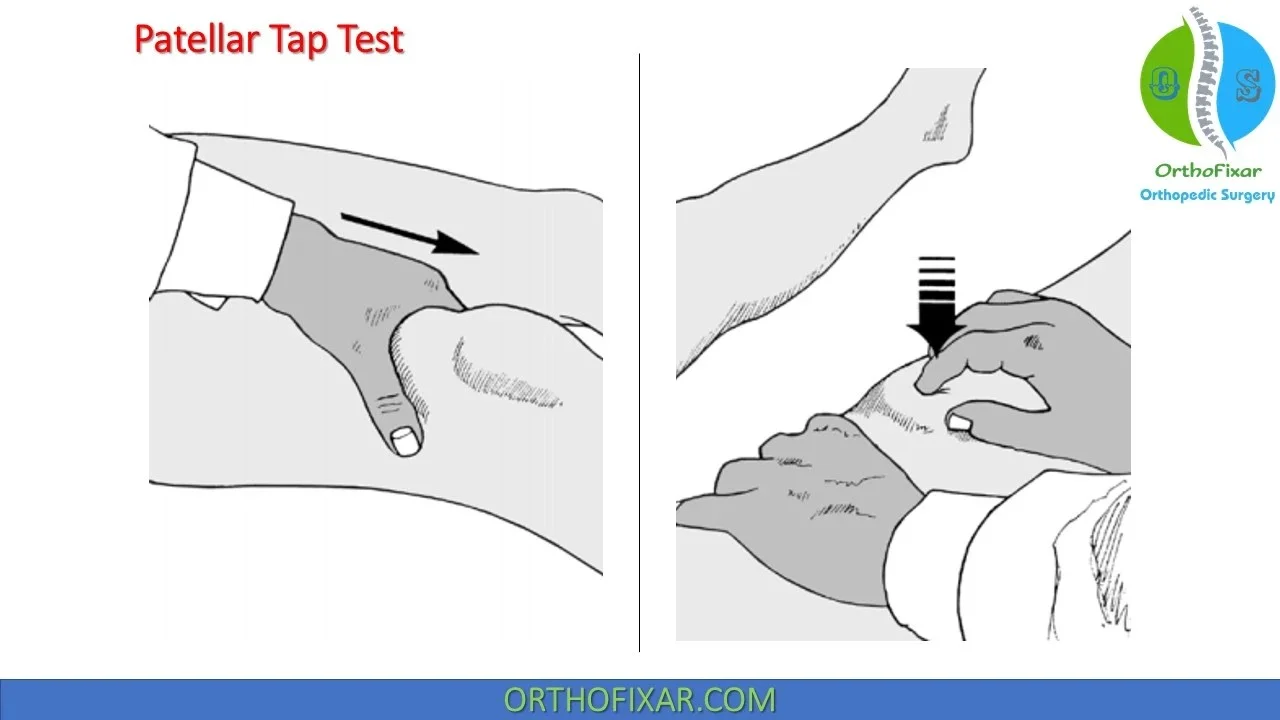
- Patellar Tap Test: For larger effusion. Empty the suprapatellar pouch by sliding one hand down the thigh. Use the other hand to push the patella downwards sharply. A distinct tap indicates significant effusion as the patella strikes the femur.
- Video Reference: Effusion Tests
- Popliteal Fossa: Palpate for masses (e.g., Baker’s cyst), tenderness, or pulsations (popliteal aneurysm).
Movement (Move)
- Range of Motion (ROM):
- Active ROM: Ask the patient to bend (flex) and straighten (extend) the knee as much as possible.
- Normal Flexion: ~135°
- Normal Extension: 0° to -10° (hyperextension)
- Passive ROM: Gently move the patient’s knee through flexion and extension, feeling for the end range and any crepitus. Compare with the active range. Note any pain during movement.
- Straight Leg Raise (SLR): Ask the patient to lift their straight leg off the couch (assesses quadriceps function and nerve root irritation if pain radiates).
- Active ROM: Ask the patient to bend (flex) and straighten (extend) the knee as much as possible.
- Strength Testing:
- Assess flexion (hamstrings) and extension (quadriceps) against resistance. Grade power (e.g., using MRC scale).
- Crepitus: Feel for grating or clicking during passive ROM.
Special Tests
-
Collateral Ligaments (MCL & LCL):
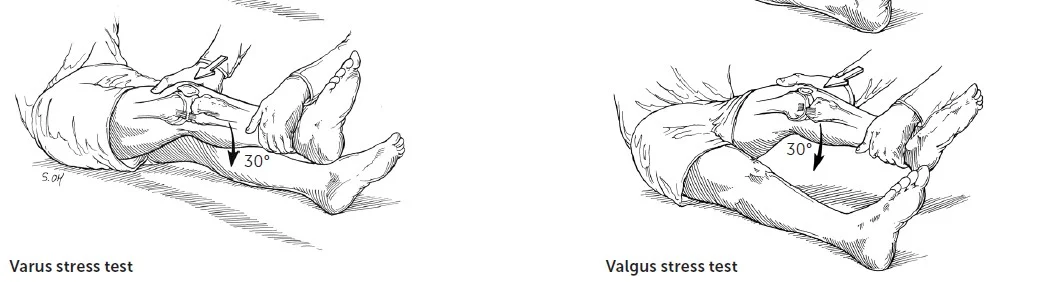
- Valgus Stress Test (MCL): With the knee slightly flexed (20-30°), stabilize the femur and apply an outward (valgus) force to the lower leg. Increased laxity or pain suggests MCL injury. Repeat in full extension (if lax in extension, suggests more severe injury involving capsule/cruciates).
- Varus Stress Test (LCL): With the knee slightly flexed (20-30°), stabilize the femur and apply an inward (varus) force to the lower leg. Increased laxity or pain suggests LCL injury. Repeat in full extension.
-
Cruciate Ligaments (ACL & PCL):
-
Anterior Drawer Test (ACL): Patient supine, hip flexed to 45°, knee flexed to 90°, foot flat on the couch (sit gently on the foot to stabilize). Place hands around the upper tibia with thumbs on the tibial plateau. Pull the tibia anteriorly. Increased anterior translation compared to the other side suggests ACL tear.
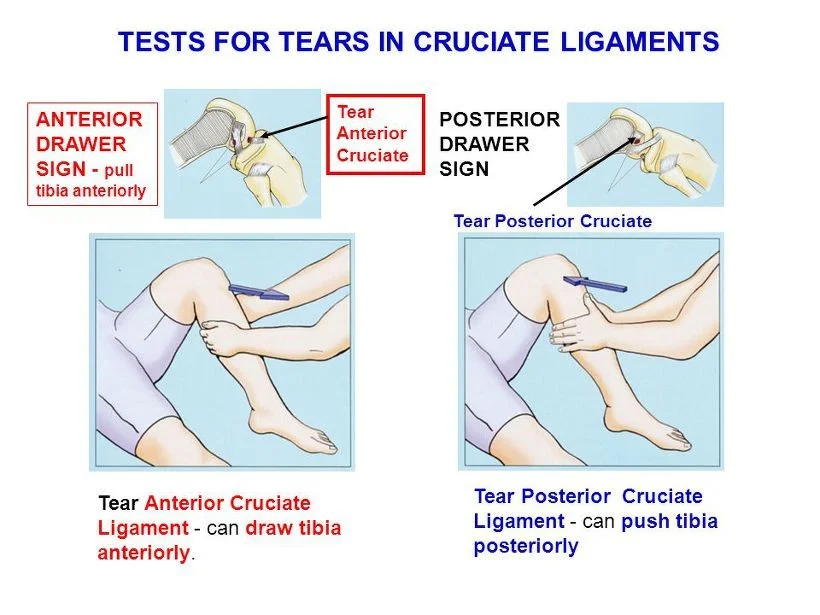
- Interpretation: Tear of Anterior Cruciate Ligament allows tibia to be drawn anteriorly.
-
Posterior Drawer Test (PCL): Same position as Anterior Drawer. Push the tibia posteriorly. Increased posterior translation compared to the other side suggests PCL tear.
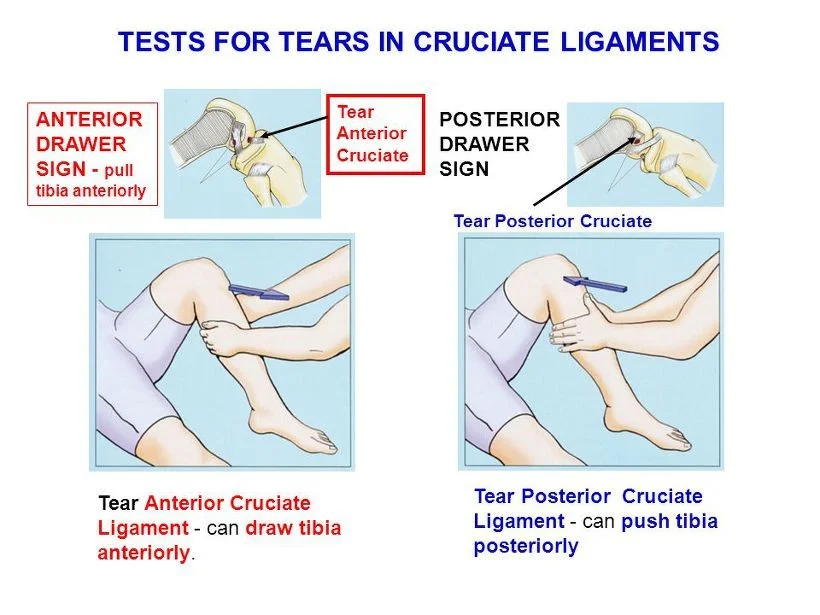
- Interpretation: Tear of Posterior Cruciate Ligament allows tibia to be pushed posteriorly.
-
Lachman’s Test (ACL): Patient supine, knee flexed to 20-30°. Stabilize the distal femur with one hand. With the other hand, grasp the proximal tibia and pull it anteriorly. Considered more sensitive than Anterior Drawer. Look for increased translation and assess the quality of the endpoint (soft/mushy vs. firm).
-
Posterior Sag Sign (PCL): Patient supine, hips and knees flexed to 90° with feet flat on the table. Observe the profile of the knees from the side. If the proximal tibia sags posteriorly on the affected side compared to the unaffected side, it suggests a PCL tear.
-
-
Menisci:
-
McMurray’s Test: Flex the knee fully. Palpate the joint line.
- Lateral Meniscus: Internally rotate the tibia and slowly extend the knee while applying a valgus stress.
- Medial Meniscus: Externally rotate the tibia and slowly extend the knee while applying a varus stress.
- A palpable or audible click, clunk, or pain localized to the joint line during the maneuver suggests a meniscal tear.
-
Apley Compression Test: Patient prone, knee flexed to 90°. Stabilize the thigh. Apply downward (axial) compression through the heel while internally and externally rotating the tibia. Pain suggests meniscal injury. (Distraction test can help differentiate ligamentous injury).
-
Duck Walk: Ask the patient to squat fully and walk a few steps. Inability to perform or pain suggests significant meniscal or cartilage injury.
-
Video Reference: Meniscal Tests
-
-
Patellofemoral Joint / Patellar Stability:
- Patellar Apprehension Test: Patient supine, knee relaxed (or slightly flexed). Gently push the patella laterally. A look of apprehension or quadriceps contraction by the patient suggests patellar instability/previous dislocation.
- Q Angle Measurement: Angle between a line from the ASIS to the center of the patella, and a line from the center of the patella to the tibial tubercle. Normal: <10-15° (males), <15-20° (females). Increased angle may predispose to patellofemoral problems.
- Video Reference: Patellar Tests
Neurovascular Examination
- Vascular: Check distal pulses (dorsalis pedis, posterior tibial), capillary refill time in the toes.
- Neurological:
- Assess sensation in the dermatomes around the knee and lower leg (L3, L4, L5, S1).
- Assess motor function (already partially done with strength testing).
- Knee Reflex (L3/L4): Test the patellar tendon reflex.
Conclusion
- Thank the patient and allow them to redress.
- Summarize findings (e.g., “Today I examined Mr./Ms. [Name]‘s knee. On examination, there was [mention key positive/negative findings like effusion, tenderness location, ROM, stability]…”).
- State further examinations: “To complete my examination, I would also examine the hip and ankle joints, and perform a full neurovascular assessment of the lower limb.”
- Suggest further steps: “Based on these findings, I would consider [mention relevant investigations like X-ray, MRI, blood tests, aspiration].”
- Ask the patient if they have any questions.
OSCE Checklist Summary (Key Points)
- Introduction: Introduce, wash hands, explain, consent, expose.
- Inspection (Standing): Gait, asymmetry, deformity, muscle bulk.
- Inspection (Supine): Scars, symmetry, swelling, skin changes.
- Palpation: Temperature, swelling (Patellar Tap, Bulge Test), palpate structures (quads, patella/ligament, tibial tuberosity, joint line, collaterals, popliteal fossa).
- Movement: SLR, Active & Passive ROM (Flexion/Extension), Strength testing (Flexion/Extension against resistance).
- Special Tests: Anterior/Posterior Drawer, Lachman’s, Varus/Valgus Stress.
- Conclusion: Thank patient, mention examining adjacent joints (hip/ankle), summarize.
Potential Investigations
- X-ray: Standard views (AP, lateral, skyline/merchant for patella). Weight-bearing views are often useful for OA.
- Bloods (CBC, ESR, CRP): If infection, inflammation, or systemic condition suspected.
- Autoimmune screen (RF, anti-CCP, ANA): If RA/SLE suspected.
- Synovial Fluid Aspiration: If effusion present, especially if infection (septic arthritis) or crystal arthropathy (gout/pseudogout) is suspected. Send for cell count, Gram stain, culture, crystal analysis.
- MRI: For detailed assessment of soft tissues (ligaments, menisci, cartilage).
- CT: Less common for knee, mainly for complex fractures or bony detail.
- Ultrasound: Useful for assessing tendons, bursae, effusions, Baker’s cysts.
Management Principles (Condition Dependent)
- General/OA:
- Education, advice, reassurance.
- Weight management.
- Exercise therapy (physiotherapy referral): strengthening, ROM.
- Assistive devices (cane, brace), appropriate footwear.
- Analgesia: Acetaminophen, topical/oral NSAIDs.
- Intra-articular corticosteroid injections for flares.
- Consider surgical referral for joint replacement if conservative measures fail.
- Gout:
- Acute: NSAIDs, Colchicine, Corticosteroids.
- Chronic: Allopurinol (or other urate-lowering therapy).
- RA/SLE:
- Acute: Steroids.
- Chronic: DMARDs (e.g., Methotrexate, Hydroxychloroquine), Biologics. Referral to Rheumatology.
- Septic Arthritis: Emergency! Joint aspiration, IV antibiotics (e.g., Ciprofloxacin, pending cultures), surgical washout may be needed.
- Ligament/Meniscal Tears: RICE (Rest, Ice, Compression, Elevation), physiotherapy, bracing, surgical repair/reconstruction depending on severity, patient age/activity level.
Doctor-Patient Interaction
- Establish rapport.
- Understand patient’s perspective (Ideas, Concerns, Expectations - ICE).
- Use appropriate non-verbal behavior (eye contact, posture).
- Show interest, concern, respect.
- Use open and closed questions appropriately.
- Listen attentively, facilitate responses.
- Summarize periodically to ensure understanding.
- Use clear, jargon-free language or explain technical terms.
- Promote shared decision-making.
- Manage time effectively.