Thyroid, Parathyroid, Neck swellings
History
Framework
- Demographics (Name, Age, Gender, Nationality, Martial, Residency)
- Chief of complaint (Cause of hospitalization + days)
- HOPI (OPERATES NON PAIN | SOCRATES PAIN)
- B-Symptoms
- Systemic Review
- Past history (medical, surgical, medication, allergies, family, social)
- summary
- differential + justify differential
- investigations - appropriate
- treatment - suggestive
Introduction, explain, Permission, Assure privacy, chap. Greetings im Mohammed 5th year medical student; could you tell me your name..“amm ahmad”. im here to take your full history, may i proceed? =-
call nurse, assure privacy.
1) Demographics
…
2) Chief of Complaint
…
3) HOPI
OPERATES OR SOCRATES
I- Site
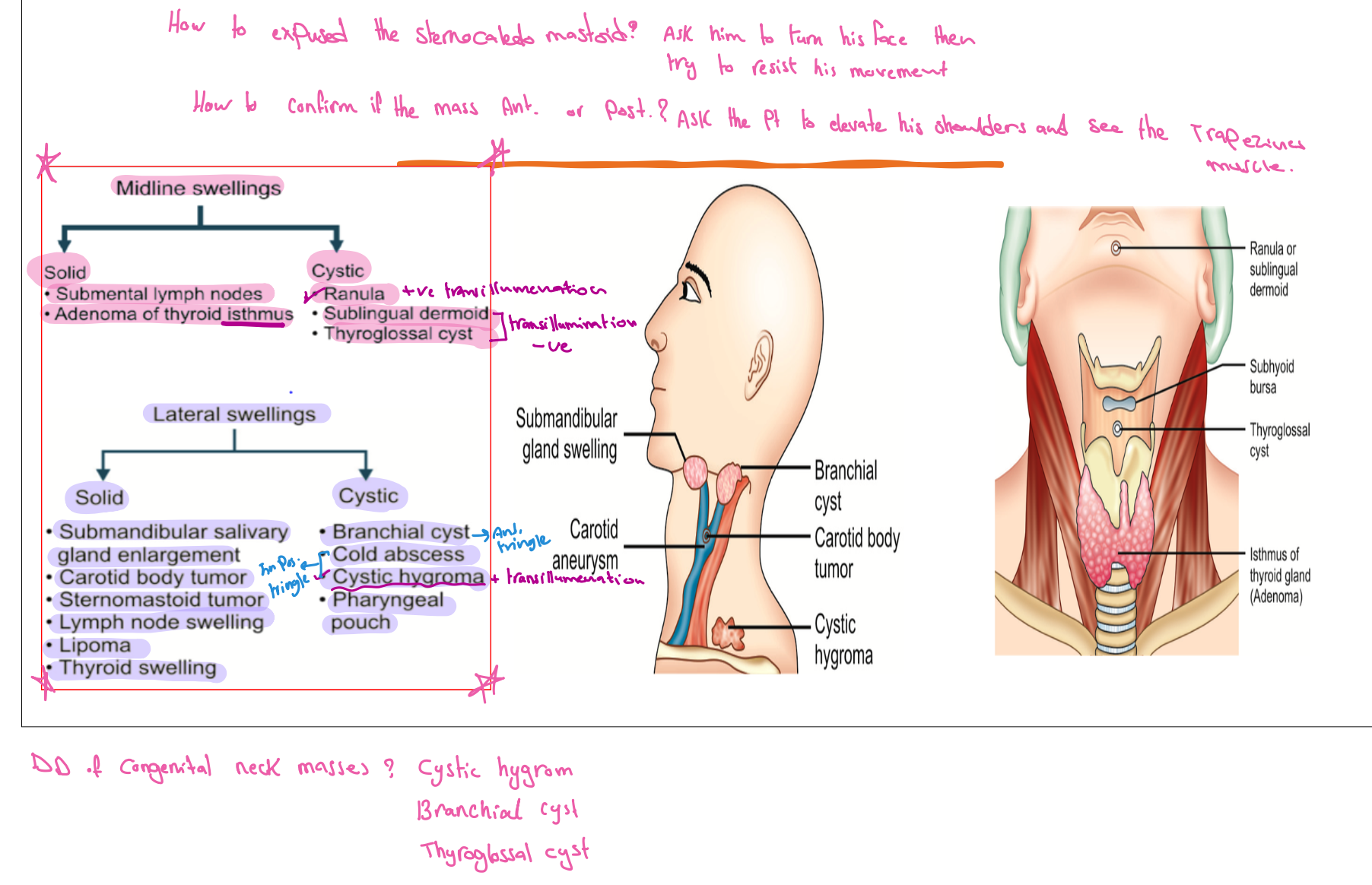
Midline swelling Solid
- Submental lymph nodes
- Adenoma of thyroid isthmus
- Calcular disease (Sialolithiasis)
Cystic
Lateral Swellings Solid
- Carotid Body Tumour
- Sternomastoid tumor
- Cervical Lymphadenopathy
- Salivary gland swellings - Viral
- Bacterial Infection
- Lipoma
- Thyroid swelling
Cystic
II- Onset/Progression
- When was the lump first noticed?
- How has it changed since it was first noticed?
- What does the patient think caused it?
III- Character
…
IV- Radiation
…
V- Associated Symptoms
General
- voice changes (malignancy)
- Dysphagia & Dyspnea (pressure on esophagus/trachea)
- Throat pain / oral ulcer / nasal symptoms / scal lesion / loss of hair
VI- Timing/Episode
- More after waking up, waking up in middle of night, more in the afternoon?
- timing, Duration, episodes of free disease.
Lump
- Has it ever disappeared or healed?
VII- Relieving/ Exacerbating Factors
Lump A lump may disappear on lying down, or during exercise, and yet be irreducible at the time of
VIII- Severity
1-10 Grading with Limitations - cant walk, work, or think
4) B Symptoms
- Fever
- Night Sweating
- Contact with infectious disease
- Weight loss
- Change in appetite
- Respiratory / gastrointestinal symptoms
5) Systemic Review
can be after HOPI or past Hx
- Nervousness
- Weight loss/gain
- Palpitation
- Preference for cold / warm weather
- Muscle fatigue
- Sweating
Thyroid
- GI – appetite, wt. change, bowel habit (thyroid, LN)
- RS- dyspnea on exertion, (retrosternal extension)
- CVS- palpitation, ankle swelling
- GU- amenorrhea
- CNS- nervousness, irritability, insomnia (thyrotoxicosis)
- Endocrines- preference to warm or cold weather
Parathyroid
-
Older women, >40 years of age.
-
Renal calculi or renal calcification – occurs in 20% of patients, polyuria (‘renal stones’).
-
Bone pain or deformity, osteitis fibrosa cystica, pathological fractures (‘painful bones’).
-
Muscle weakness, anorexia, intestinal atony, psychosis (‘psychic moans’).
-
Peptic ulceration and pancreatitis (‘abdominal groans’)
-
Muscle spasms, face twitching
6) Past Hx
Past medical / Surgical / Family
-
similar episode as before similar problem - (you can mention with HPI)
-
Chronic diseases + Family Hx / similar conditions (MEN2, MTC, Pheochromcytoma, HPT)
-
Past Admission + transfusion + Surgeries
-
Pregnancy / Lactation
Lump Has (or had) the patient any other lumps or ulcers?
(lymphonedapathy), (neurofibromatosis)lipoma - benign (excision)Multiple Painful Lipoma - Dorcum's diseaseHernia - (Repair/Suture or Excision)I&D - Abscess drainage
Medications / Allergies
Social im going to ask some specific question to reach to diagnosis, may i?
- Occupation,
- Travel,
- kids,
- smoking,
- alcohol,
- drugs,
- sexual activity
7) Summary
77 yo sudanese male complaining of neck pain for 9 days which was severe compressing associated with cough, with no hx of palpitation, sweating.
8) Differential, Impression, most likely diagnosis
-
Congenital: Thyroglossal cyst, Lingual thyroid
-
Simple:
-
Non-toxic goitre,
-
MNG,
-
Solitary Thyroid Nodule (STN),
-
-
Functional disorders:
- Hypothyroidism
- Hyperthyroidism: Grave’s disease, Toxic adenoma, Toxic goiter (Toxic MNG), Thyrotoxicosis factitia
-
Thyroiditis:
-
- Benign: Follicular adenoma
- Malignant: Papillary, Follicular, MTC, Anaplastic, Lymphoma, Metastatic
9) Investigations
General
- CBC, Serology, Tuberculin
- Thyroid function (TSH, T3, T4, Antibody) (very important)
- CXR, U/S, CT scan, MRI, Angio.
- FNAC
- Laryngoscopy, Endoscopy (preop, to check if both vocal cords are functioning or not)
- Open biopsy
Assessment of thyroid disease
- FT4, T3,TSH (TSH low in hyper, high in hypo) TRH (hypothalamus)
- Serum Calcitonin (MTC)
- Antibodies: TSI-thyroid stimulating immunoglobulin, Anti-thyroglobulin antibody, anti-TPO- thyroid peroxidase
- Ultrasound
- FNA: accurate, palpation/US guided- non-diagnostic /benign/ undetermined / follicular neo./ suspicion of malignancy/ malignant- Bethesda system
- Radioisotope scanning (Tc99-Sodium pertechnetate)- toxic goitres
- CXR, CT, MRI ( retrosternal mass, staging malignancy, local invasion)
- PET scan
- Laryngoscopy- vocal cord assessment
Assessment of parathyroid disease Hyper
- DEXA: Wrist, spine, and hip
- KUB, IVP, CT (For renal stones)
- High PTH, urinary/serum CA, Alkaline phosphotase
- Low Mg, Phosphate
Hypo
- Blood levels of ionized Calcium and PTH are low,
- Reduced serum calcium increases neuromuscular excitability.
- Also measure vitamin D and magnesium.
- ECG: shows a lengthened Q–T interval
10) Treatment Plan
… depends on cause
Examination
-
WIPER
- Wash hands
- Introduce
- Right side of bed
- Explain Procedure
- Permission for examination
- Position & Exposure
-
Preliminary examination
- General Appearance (man, comfortable, comatose, connected device)
- General examination (Vitals, hand/arm/axilla, hair, face, neck, chest, abd,leg)
-
Focused Examination + (correct technique)
- Specific System Exam - IPPA
- Inspection
- Palpation
- Percussion
- Auscultation
- Lesion/Swelling/Ulcer if present - SSSS TTEDC
- Specific System Exam - IPPA
-
Describe correct physical findings
1) WIPER
Exposure | position | privacy | Ask for vitals
- W ash hands (before and after)
- I ntroduce yourself to the patient and seek his or her consent
- P osition the patient correctly.
- E xpose the patient as needed (e.g. ‘Please take off your shirt for me now, if that is all right’)
- R ight side of the bed
Position & Exposure Neck exam: Sitting - Chin to Nipple line
Intro
Greet, Introduce (5th year med), assure privacy (curtain, nurse), explain procedure, position (mention good position - supine semisitting) & exposure (from midchest to midthigh - cover genatelia)
In the end thank the patient document.
2) General Appearance
- Conscious and alert
- features
- connected devices
elderly male with good build lying comfortable to be - connected to cannula - not connected oxygen. (note general exam findings)
Agitation, nervousness or lethargy, myxedema,
“Now i will do focused examination after general apperance, should i do general examination?”
Is the patient well or unwell, comfortable or in pain, moving easily or lying motionless? e.g. peritonitis?
Writhing in agony, e.g. ureteric or biliary colic?
3) General Examination
dont touch patient until needed
- Hand: organized explaination from distal to proximal
- Clubbing -
- Capillary refill
- Pulse:
- water hammer pulse
- Vital signs
- Face & Neck:
- Abdomen:
- Lower Limb: Edema - thumb
Neck: Whole Patient Agitation, nervousness or lethargy, myxedema,
Hands sweating, tremor, tachycardia, dry, irregular pulse/temprature, palmar erythema thyrotoxicosis - fine fast tremor
Face Myxedema
Eyes lid retraction, exophalamos, lid lag H test, ophthalmoplegia, chemosis, Lid lag Ophthalmoplegia, particularly of the superior rectus and inferior oblique muscles (cannot look ‘up and out’) Exophthalmos, which also causes difficulty with convergence and absent forehead wrinkling when looking upwards
Neck
- Lump moves with swallowing? protrusion of tongue?
- skin
- scar transverse cervical incision
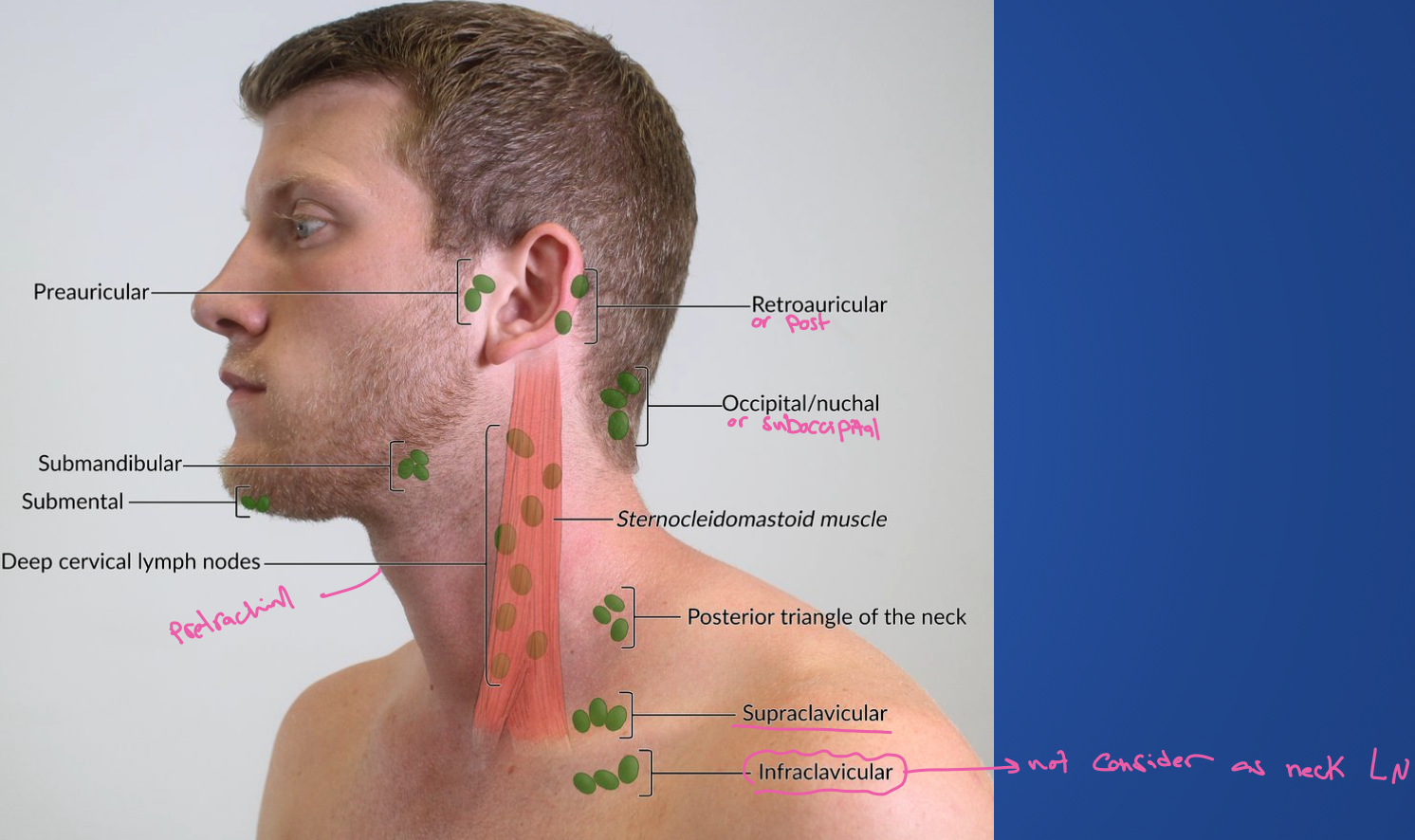
Palpate Cervical LN’s
Extremities
- edema
4) Focused Examination
Lesions/Mass/Ulcer Examination
I- Comment on lesion if found while examining anywhere in body, ask instructor to Start its own inspection palpation auscultate percussion then continue with previous focused examination
- Site (right neck swelling, lateral of second toe)
- Size (0.2x0.8 Meters/cm use ruler)
- Shape (Irregular, regular (round), Oval)
- Surface (feel surface Nodular or Smooth)
- Depth (Deep or superficial - check contraction after squeeze hand)
- Color (strawberry, portwine?, purple, orange, chronic inflammation; hyperpigmentaiton, redness; active inflammation) (thick granulation tissue with slight oozing of serious discharge)
- Temperature ( Hot; Abscess, Malignancy , Cold, Normal; Lipoma)
- Tenderness (Painful or Painless)
II- Composition: Solid, fluid or gas
- consistency (Hard/Firm/Soft like?) (soft if pheripheral??)
- fluctuation (Fluid; Cyst - Pseudocyst; without epithelium Push two fingers against another in between pressing from above) (Cystic push in central)
- fluid thrill ()
- translucence (Torch; hydrocele - any cyst vs hernia)
- resonance
III- Mass Pull skin to see if its attached to skin (such as sebaceous cyst) (video?)
put your fingers in between sternocleidomastoid to separate mass (video?) - attached to muscle
IV- Vascular
-
pulsatility (Transmitted/True? - aneurysm, varicose) - Expansile vs transmission (two finger))
-
compressibility (Tumour/Hernia/)
-
bruit (Turbulence/Murmur - thrill if palpable)
- Reducibility (Renal Hernia, cough)
- Relations to surrounding structures – mobility/fixity
- Regional lymph glands (Malignancy/Infection — Primary / Secondary
V- State of local/Surrounding tissues:
- scars/edema
- Arteries (examine arteries before & after the swelling (Parathesia, loss of pulse etc..))
-
nerves - cotton, pin prick, position/vibration sense etc…
-
Bones and joints
Neck Focused Examination
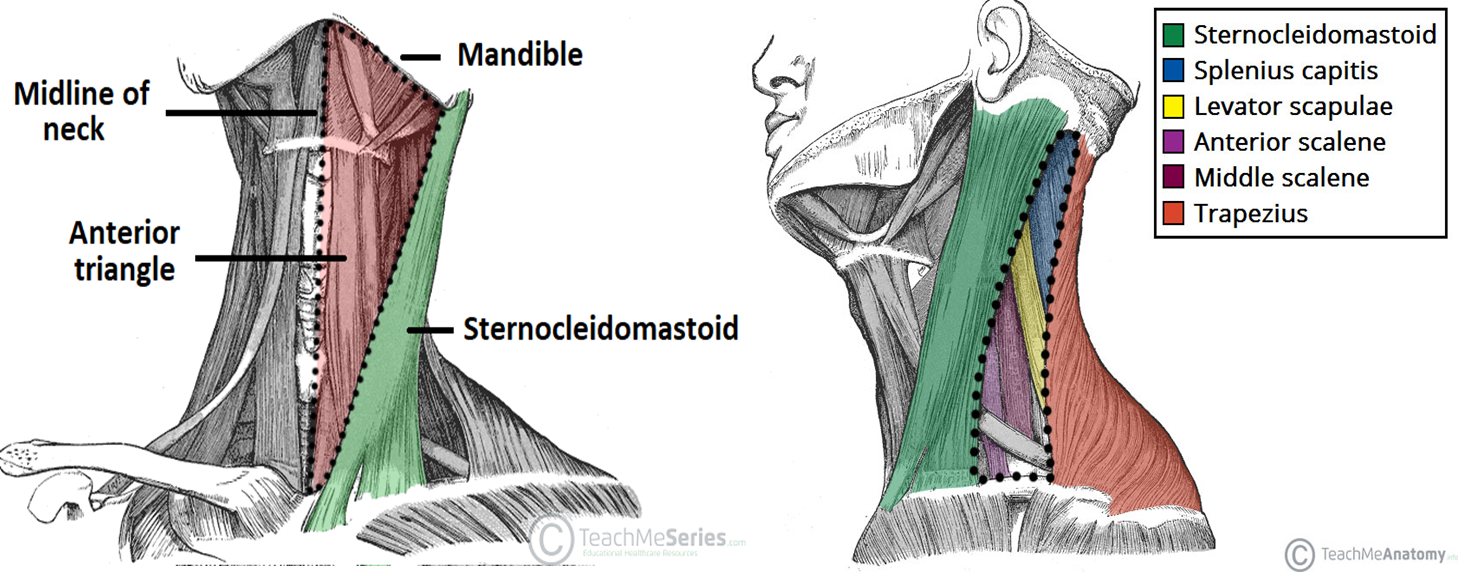
Inspection
-
at same level - check for wounds, sinuses, discharges, neck vein distension, (Pemberton’s sign; raise both arms), discoloration; hyperpigmentations, retrosternal thyroid extension
-
check from sides (to check visible pulsations, bulging)
-
Movement from swallowing (This indicates it is deep to the pretracheal fascia and likely to be thyroid. (thyroid, lymph nodes pretracheal fascia)
-
Protrusion of tongue (thyroglossal cysts)
-
Ask patient to raise arm to check for PEMERTON’s SIGN with goiters
Palpation
Infront Patient
-
Tracheal deviation/position - 2 fingers placed on head clavicle w/ middle finger on rings of trachea.
- once hands are placed you would feel tracheal position then comment.
Behind
-
palpate three fingers against one side of lobe pushing the other against it - ask patient to swallow (give water). dont move both hands at same time. then palpate while patient protruding his tongue
-
Palpate lower pole/edge of thyroid/mass to exclude retrosternal goiter - if its positive non palpable its retrosternal goiter) -
-
Comment on lesion (solitary in one sided? toxic solitary?)) - comment on lesion as previously mentioned S4 DECTT,
-
Comment on palpation lesion/Thyroid - follow through with Lesion format in inspection
- Site
- Size
- Shape
- Tenderness -by staring at patient eyes from behind at all times
- Temperature - of each side - compare with sternum
- Number
- Consistency (Fluctuation; Cystic or firm)
- Surface
-
Thrill by palpation - bruit by asucultation
-
pulsation is seen - is it transmitted or expansile?
-
Carotid/ superficial temporal Pulsation - carotid pulse is present but deviates - if both not felt = malignant (berry’s sign)
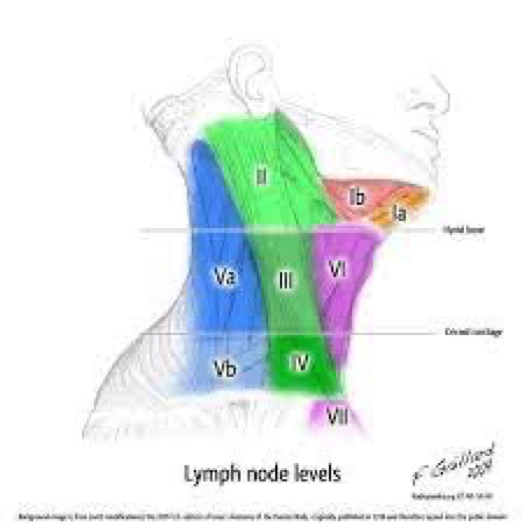
Lastly behind patient examine LN’s Neck (submental, submandiublar, pre-pot auricular, sub-occipital, Anterior/Deep cervical, Post/Superficial cervical supraclavicular)
Clinically, Lymph Nodes are arranged in 2 Main groups: Transverse - Submental, Submandibular, Pre and Post Auricular, and Occipital.
Longitudinal – Cervical group (Anterior and Posterior Cervical), and Supra-Clavicular Listening for Bruiting is required for the Neck examination, but not for the Thyroid. As the Carotid Artery is part of the neck.
-
I- submental submandibular
-
II, III, IV - Sternoclediomastoid
-
V- Post Sterno
-
VI - Pre Sterno
-
VII - Sternum
Percussion
on manubrium sterni - direct tapping any dullness - retrosternal goiter
Auscultation
- Auscultate both lobes to check for any Bruit while patient holding his breath
- carotid auscultation for bruit also
5) Complete examination with
- CVS- sinus tachycardia/ fibrillation
- Respiratory system: Tumor, TB
- Abdomen: Hepatomegaly, splenomegaly, other mass, testis
- Extremity- proximal muscle weakness, pretibial myxedema (thyroid dermopathy) – localized lesions of the skin from the deposition of hyaluronic acid
6) Summarize Findings, Thank patient
…
Other notes
Types
functional
- (hypothyroidism, hyperthyroidism; graves/ toxic)
structural
- (goiter, multiple nodule enlargement; could be benign or )
both of them
- ?
S/S
HYPER
- Exophalamos with graves
Investigation
Iodine scan can differentiate all major types
normal hypo would not have any uptake
TSH T3, T4, ANTI-TPO - then confirm with thyroid scan
TSH is most important to differentiate between primary vs secondary Subclinical when TSH is normal and T3 & T4 is abnormal - such as thyroiditis
Anatomy
- Sup & Inf thyroid artery : ICA & SBClavian branch to INF
- Middle thyroid vein: IJV
Superior laryngeal nerve (internal & External; preserve sensory branch)
- External branch: loss high pitch voice
reccurent laryngeal nerve
- Vocal - quality of voice
Steps of incision
Kocher / Collar incision is made
- skin
- subcutanous fat
- superficial fascia (platysma, anterior jugular veins)
- create four flaps from each side
- Strap muscles - linear frafle? four muscles -
- sternohyoid, sternothyroid, thyrohyoid, Omohyoid,
- Thyroid seperate muscles, look for the lobes - thyroid gland is attached in place by suspensory ligament, peri ligament
- Deep cervical faccia ()
Isolate, ligate, divide
- Ligate (Superior and inf vessels ) (inf sup pedicle)
- Divide (middle thyroid vein)
- isolate? (disect surrounding structure for pedicle)
tracheoesophageal group for reccurenty, reserve
dissect berry ligament
cut by the distal to avoid death or parafoliccalar cells
thyroid trachea lobe?
Parathyroid each has overlying fat - if blood vessel compromised and it died attempt transplantation - dissect fat away, keep gland cut it in small slices, implant it in sternocleidomatoid muscle with non-absorable suture
Cut smaller sizes to avoid ischemic events for some of the pieces, and there would be higher perfusion and sucess rate within 6 months