Intrauterine Growth Restriction (IUGR)
Etiologies
Maternal factors
- Chronic illness (e.g. diabetes with vascular involvement**, hypertension, renal disease, anemia, pulmonary disease)
- Pre-eclampsia
- Early or advanced age
- Malnutrition
- Uterine malformations
- Substance abuse (e.g. cigarettes, alcohol, narcotics, cocaine)
- Medications (e.g. warfarin, anticonvulsants)
Placental factors
- Uteroplacental insufficiency
- Abnormal implantation
- Vascular anomalies
- Placental abruption
- Infarction
- Tumour
- Villous placentitis (bacterial, viral, parasitic)
Fetal factors
- Chromosomal disorders
- Congenital anomalies
- Multiple gestation
- Infection (e.g. TORCH, malaria, varicella)
- Metabolic disorders
*TORCH: Toxoplasmosis, Other (syphilis), Rubella, Cytomegalovirus, Herpes simplex virus **While diabetes with vascular involvement can cause restricted fetal growth, while DM without vascular involvement it typically causes excessive growth resulting in a fetus who is large for gestation age (LGA).
Complications
- Increase perinatal mortality.
- Cerebral palsy.
- Stillborn infants (IUFD).
- Delay milestones.
- Short stature.
- Intrapartum fetal distress and asphyxia.
- Meconium aspiration.
- Emergency CS.
- Necrotizing enterocolitis.
- Hypoglycaemia and hypocalcaemia.
- Later on life more borne to CVD & diabetes.
Diagnosis
-
History:
- Identifying mother at high risk
- Gestational age must be established with certainty, preferably in the first trimester, to assess fetal growth accurately.
- Clinically: A lag in fundal height of more than 4 cm from gestational age after 20 weeks should prompt sonographic evaluation.
-
Sonographic assessment:
- Most useful tool for diagnosis of IUGR.
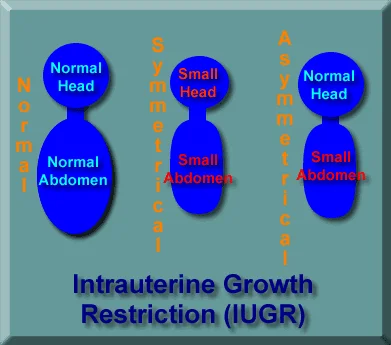
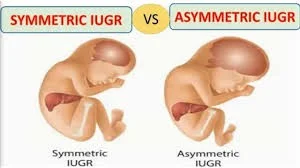
- To differentiate between symmetrical and asymmetrical IUGR
- To monitor fetal condition.
Sonographic component Used to Assess Fetal Growth
-
Fetal biometry:
- Estimated fetal weight
- Abdominal circumference(AC) : AC and weight are most accurate US parameters for diagnosis IUGR
- BPD (Biparietal diameter): to determine GA and type of IUGR
- Head circumference (HC) : better than BPD in predicting IUGR
- HC:AC ratio (head circumference/abdominal circumference)
- normally decreases linearly from 16 to 20 weeks of gestational age
- HC/AC increase > 2 SD above mean is predictive of IUGR (symmetrical)
- FL/AC ratio (Femur length /abdominal circumference) : norm ranges 22 % , ratio above 23 % consider abnormal
-
Placenta morphology
- Advanced placental grade.
-
Amniotic fluid index
- Presence of Oligohydramnios without ruptured membranes.
-
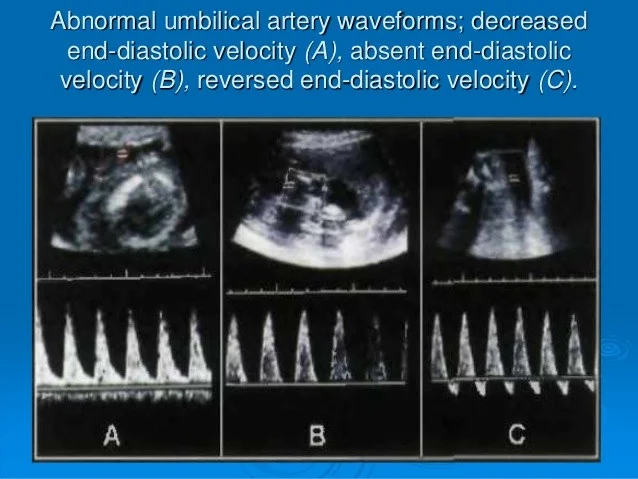
Umbilical artery Dopplers
Role of Dopplers in diagnosis IUGR
- Can help distinguish between constitutionally small vs. IUGR
- Useful for evaluating pregnancies at risk for adverse events
Doppler features:
- Umbilical artery doppler assessment (most important)
Increased S/D ratio(s) , absent end diastolic flow and finally reversed end diastolic flow. Perinatal mortality rate increases significantly in fetuses with absent end diastolic flow (9-41%) and reversed end diastolic flow (33-73%) in umbilical artery. Increased resistive index (RI)
- Middle cerebral a. (MCA) : ↓ resistance and ↑Peak systolic velocity (blood redistribution, brain sparing)
- Abnormal ductus venosus flows associated with fetal acidaemia and the highest perinatal mortality compared to those where flow abnormalities are confined to the umbilical or middle cerebral artery
- Umbilical venous doppler assessment
- Presence of pulsatility
- Uterine arterial doppler assessment
- Increased S/D ratio(s)
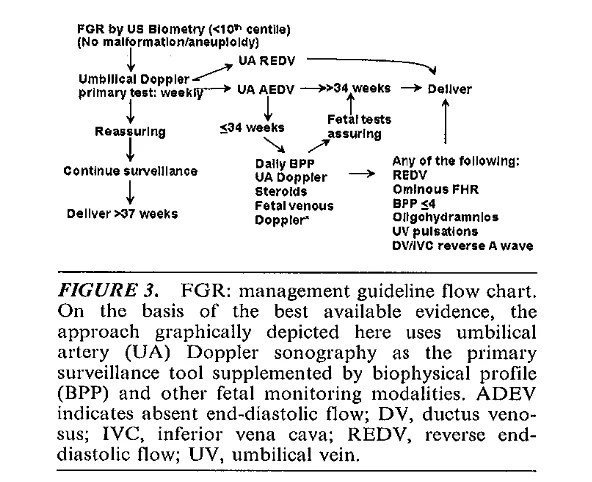
Management
-
Since IUGR fetus is at increased risk of intrauterine hypoxia and intrauterine demise, the decision needs to delicately balance the risk to the fetus in utero with continuation of pregnancy and that of prematurity if delivered before term
-
Identify cause : Growth restriction less than the third percentile diagnosed before 32 weeks prompts offering amniocentesis or fetal blood sampling for karyotype and viral studies.
Delivery vs conservative management :
Depend on gestational age
- Preterm IUGR :
- Conservative management : if less than 37 weeks of gestation
- Treat/modify underlying cause .
- Restrict physical activity, left lateral position , steroid , low dose aspirin, Maternal oxygen therapy
- Adequate nutrition ,
- Initiate fetal surveillance.(Includes daily kick counts, serial fetal growth ultrasounds every 3 to 4 weeks, and nonstress testing and biophysical profile twice per week , weekly or twice weekly Doppler .
- Continue expectant management and deliver if fetal lung maturation has been achieved at 37 weeks .
- Deliver earlier if no fetal growth has been documented ( 2 weeks interval) , oligohydramnios , reversed end diastolic , poor BPP, un-assure nonstress test
- Conservative management : if less than 37 weeks of gestation
- Term IUGR
- Delivery : if IUGR ≥37 weeks
FGR by US Biometry (<10th centile) (No malformation/aneuploidy)
Mode of delivery :
Vaginal delivery is not contraindicated, can be allowed as long as there is no obstetric indication for caesarian section and fetal heart rate is normal , but there is an increased risk of fetal intolerance of labor.
-
Fetuses with major anomaly incompatible with life should also be delivered vaginally.
- Caesarian section: is indicated In all cases of IUGR with features of acidosis , these include:
- Abnormal CTG ,poor BPP , reversed of end diastolic flow in UA , acidic fatal PH .
- Caesarian section: is indicated In all cases of IUGR with features of acidosis , these include:
Outcomes
- Symmetric vs. Asymmetric IUGR symmetric has poorer outcome compared to asymmetric
- Preterm IUGR has high incidence of abnormalities
- IUGR with chromosomal disease has 100% incidence of handicap
- Congenital infection has poor outcome - handicap rate > 50%
- IUGR has higher rate of learning disability.