Orthopedics
Osteomyelitis
Definition and Basic Concepts
-
Osteomyelitis: Bone and marrow infection
- Osteo = bone
- myel = bone marrow
- itis = inflammation
-
Infection: Multiplication and spread of pathogenic organisms within the body tissues
-
Inflammatory reaction: Acute / Subacute / Chronic
- Redness, Heat, Swelling, Pain, Loss of Function
- Rubor, Calor, Tumor, Dolor, Functio Laesa
Classification
-
Timing:
- Acute OM
- Subacute OM
- Chronic OM
-
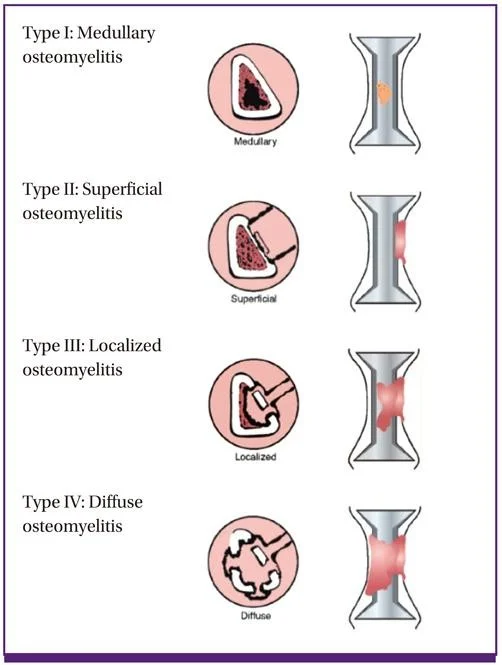
Location:
- Medullary
- Superficial
- Localized
- Diffuse
-
Organism:
- Specific (e.g. TB, Brucellosis, Fungal)
- Nonspecific (most common)
Types of Osteomyelitis
Type I: Medullary osteomyelitis
Type II: Superficial osteomyelitis
Type III: Localized osteomyelitis
Type IV: Diffuse osteomyelitis
Pathophysiology
Bone vs Soft Tissue Infection
- Bone infection is different from soft-tissue infection:
- Bone consists of rigid compartments
- Pressure is increased in acute inflammation
- More vascular damage and cell death because of the tight compartments
- If not rapidly suppressed, will lead to necrosis
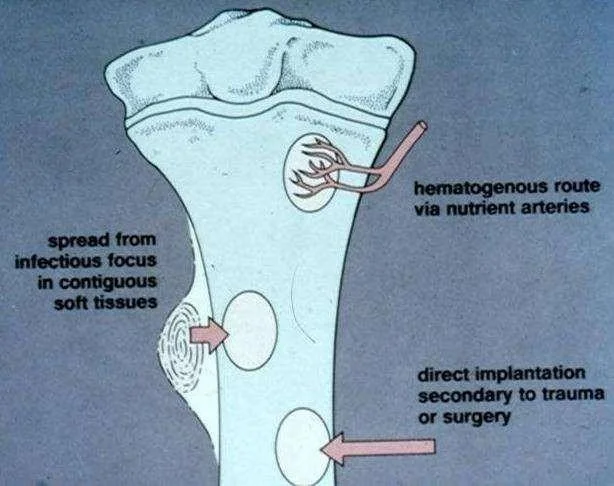
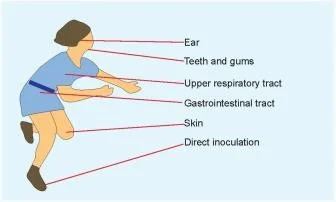
Mechanism of Spread
- Hematogenous: Originated or transported by blood due to skin lesion, infection, or trauma
- Contiguous-focus: Associated with trauma, cellulitis, or poor vascularity
- Direct-inoculation: Penetrating injuries or surgical contamination
Factors Affecting Type and Severity
- Type of invader (virulence)
- Site of infection
- Host response
Host Response Factors
- Host immunocompetency
- Extremes of age
- Diabetes
- Obesity
- Alcohol or Tobacco abuse
- Steroid use
- Malnutrition
- Medications
- Previous radiation
- Vascular insufficiency
Acute Osteomyelitis
Epidemiology
- Mostly children
- Boys > girls
- History of trauma often present
- ? Micro-hematoma
- ? insignificant
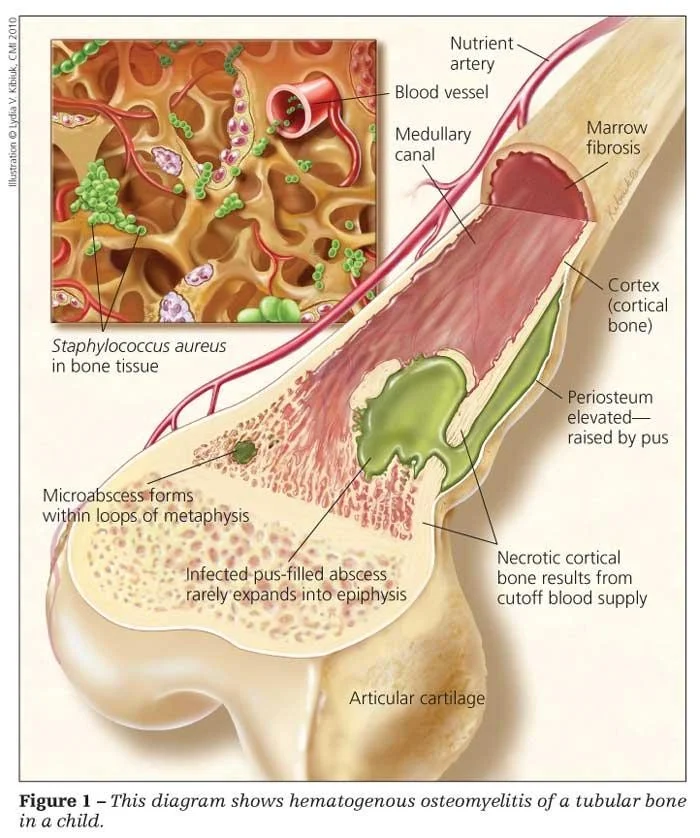
Pathology
Formation of Pus
- Concentrate of defunct leucocytes, dead and dying bacteria, and tissue debris
- Localized in an abscess
- Pressure builds up (tight space)
Spread of Infection
Local spread:
- Through the cortex
- Along adjacent tissue planes
- Nearby joint
Distant spread:
- Via lymphatics, causing lymphangitis & lymphadenopathy
- Via the blood stream (bacteremia & septicemia)
Common Organisms by Age Group
| Age group | Most common organisms |
|---|---|
| Newborns (younger than 4 mo) | S. aureus, Enterobacter species, and group A and B Streptococcus species |
| Children (aged 4 mo to 4 y) | S. aureus, group A Streptococcus species, Kingella kingae, and Enterobacter species |
| Children, adolescents (aged 4 y to adult) | S. aureus (80%), group A Streptococcus species, H. influenzae, and Enterobacter species |
| Adult | S. aureus and occasionally Enterobacter or Streptococcus species |
| Sickle Cell Anemia | S. aureus is most common, Salmonella is pathognomonic |
| Drug addicts | Staph aureus is most common, Pseudomonas is pathognomonic |
| Implant | S. Epidermidis is most common |
Source of Infection
Hematological (the commonest):
- Infants: Infected umbilical cord
- Children: Boils, tonsillitis, skin abrasions, pricks, otitis media, gastroenteritis, teeth, …
- Adults: UTI, urinary catheter, indwelling arterial line, septic tooth, dirty needle…

Typical Location
- Metaphysis of long bones
- Upper tibia, proximal or distal femur
- ?Trauma
- Peculiar arrangement of blood vessels
- Terminal arteries twist back in hairpin loops
- Vascular stasis
- Lowered oxygen tension
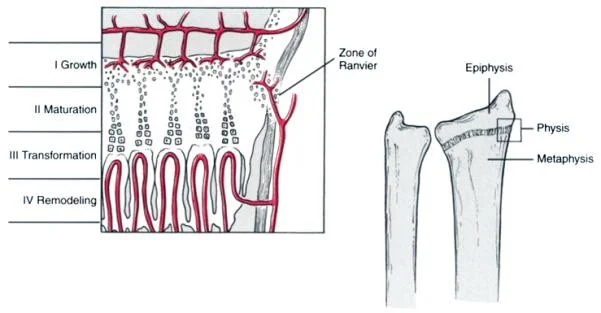
Age-Specific Vascular Considerations
- In infants, infection may reach Epiphysis
- Anastomoses between metaphyseal and epiphyseal blood vessels
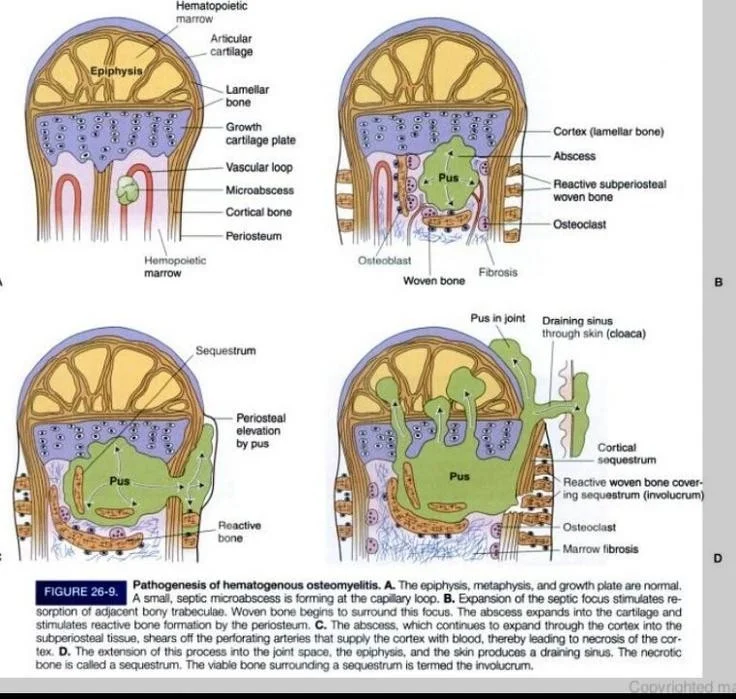
Disease Progression
Inflammation:
- Intra-osseous pressure rises
- Severe pain & obstruction of blood flow
Suppuration:
-
Pus from day 2
-
Sub-periosteal pus collection
- Re-enters bone
- To soft tissue
- To joint
-
May spread to the joint causing Septic Arthritis
- In infants
- In joints where metaphysis is partly intra-capsular (Hip, shoulder, elbow)
Necrosis (> 7 days):
- Blood supply compromised by raised pressure, stasis, thrombosis, periosteal stripping
- Biofilm formation: Bacteria produce biofilm that covers necrotic bone and hardware
- Made of an exopolysaccharide
- Antibiotics have difficulty penetrating biofilm
- Sequestrum formation (dead bone)
- Involucrum formation (Sub-periosteal New bone)
- Resolution: If infection controlled, & pressure released

Diagnosis
hx, radio, labs, aspiration
Clinical Presentation
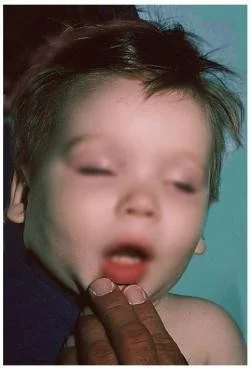
Infants
- Commonest around the knee
- Constitutional symptoms may be mild
- Failure to thrive, drowsy, irritable
- History of other infections (umbilical)
- Metaphyseal tenderness
- Decreased range of motion (ROM)
Children
Systemic symptoms:
- Severe pain
- Malaise
- Fever
- Reluctant to move
- Toxemia
- History of previous source of infection (sore throat, skin infection, prick, injury, otitis media, gastroenteritis, teeth/gums, …)
Local signs:
- Localized pinpoint tenderness
- Hotness
- Local redness, swelling, edema (late signs)
- Reduced range of motion


Adults
- Fever
- Commonly thoracolumbar spine
- Backache
- History of UTI or urological procedure
- Old, diabetic, immune-compromised …
Radiology
X-ray
- AP and lateral of the limb in question Changes:
- Soft tissue swelling (early)
- Osteolysis (10-14 days): Metaphyseal rarefaction
- Late films (1-2 weeks): reduction in metaphyseal bone density (bone refraction)
- In Chronic OM:
- Sequestrum → dead bone with surrounding granulation tissue
- Involucrum → periosteal new bone
First sign (10-14 days):
- Metaphyseal rarefaction
- Periosteal reaction (new bone formation)



Ultrasound
- Detects sub-periosteal pus collection

CT
- Useful for surgical planning and determining extent of bony destruction
MRI
- Detects abscesses and early marrow and soft tissue edema
- Distinguishes between bone & soft tissue infection
- T1 signal decreased, T1 with gadolinium signal increased & T2 signal increased
- 88% to 100% sensitivity

Bone Scan
Increased activity – early
- Sensitivity comparable to MRI, but specificity is poor Indications:
- Non-diagnostic x-ray
- Localize pathology in infant or toddler with non focal exam
- Cold bone scan may be associated with more aggressive infections


Laboratory Tests
Basic Tests
-
WBC: Elevated in acute osteomyelitis
-
Erythrocyte Sedimentation Rate (ESR): Elevated but not specific; less reliable in neonates and sickle cell patients
-
C-reactive Protein:
- Elevated in 98% of patients with acute hematogenous osteomyelitis
- Becomes elevated within 6 hours
- Most sensitive to monitor therapeutic response
- Failure to decline after 48 to 72 hours of treatment should indicate that treatment may need to be altered
Cultures
- Blood Culture: Positive only 30% to 50% of the time; will be negative soon after antibiotics are administered
- Bone Aspiration / Biopsy: Required for definitive diagnosis; 50% to 85% of affected patients have positive cultures
Differential Diagnosis
- Cellulitis
- Acute septic arthritis
- Acute rheumatism
- Sickle cell crisis
Treatment
Principles
- Acute infections, if treated early with effective antibiotics, can usually be cured
- Operative drainage needed once there is pus and bone necrosis
Treatment Outline
- Admission, Hydration, Immobilization, Analgesics & Correction of electrolyte
- Take samples for culture
- Start empirical broad-spectrum Abx (Not indicated as empirical treatment in chronic OM)
- Observe improvement with clinical parameters and blood tests
- Review culture results and proceed accordingly
- Decide duration of Abx (IV vs oral)
- If no improvement, proceed to surgical debridement
- Use of fixation according to stability
Surgical Treatment
Surgical Drainage, Debridement And Antibiotic Therapy
- If start antibiotic early, may not need surgery
Indications:
- Deep or subperiosteal abscess
- Failure to respond to antibiotics for >24 hrs
- Frank pus on aspiration
- Spinal cord decompression & fusion in cord injury or instability
Contraindications:
-
Hemodynamic instability, as patients should be stabilized first
-
Delay of drainage may lead to chronic OM
Antibiotic Treatment
Children & Fit Adults (Staphylococcus aureus)
- I.V. flucloxacillin (a penicillinase-resistant penicillin)
- Change according to result of culture & sensitivity
- If MRSA, change to Vancomycin
- Use Vancomycin or clindamycin if penicillin-allergic
- Duration: 2 weeks I.V to start with, followed by 3-6 weeks oral
Children < 4 yrs (H influenzae & Gram-negative)
- Third generation cephalosporin
Complications
- Septicemia
- Metastatic infection
- Septic arthritis
- Pathological fracture
- Altered bone growth
- Chronic osteomyelitis
- DVT
Case Example - 5 Year Old Boy
Initial Presentation:
-
Pain, tenderness, fever lower thigh
-
WBC high, CRP high
-
MRI: positive

 Progression:
Progression: -
After open drainage and drilling - only of lower part (8 days)

-
After 3 weeks
-
After 2 months: pathological fracture

-
After 8 months: poor healing with infection
-
After 11 months: after plating


Subacute Osteomyelitis
Characteristics
- Mild form: Less virulent organism, more resistant patient
- Most commonly involves femur and tibia
- May occur in:
- Partially treated acute osteomyelitis
- Occasionally in fracture hematoma
Clinical Features
- Long history (weeks, months)
- Pain, limp
- Swelling occasionally
- Local tenderness
Laboratory Findings
Frequently normal:
- WBC count
- Blood cultures
Usually useful:
- ESR
- Bone cultures
Radiology
- X-ray: Brodie’s abscess
- Well defined cavity in metaphysis
- Localized radiolucency seen in long bone metaphyses
- Difficult to differentiate from Ewing’s sarcoma
- Bone scan / MRI
- Biopsy / aspiration: (50%) grow organism; to rule out tumor

Treatment
- Antibiotics for 6 months
- Surgery to evacuate the abscess
Chronic Osteomyelitis
Etiology
May follow acute OM:
- Not treated properly
- Inadequate antibiotic
- Inadequate duration
- Needed drainage not performed
May start De Novo:
- Following operation
- Following open fractures
Organisms
- Usually mixed infection
- Mostly:
- Staph. aureus
- E. coli
- Staph. pyogenes
- Proteus
- Pseudomonas
- Staph. epidermidis: with implants (metal)
Pathology
- Cavities
- New bone formation: (Involucrum)
- Cloacae: openings in Involucrum
- Dead bone: (Sequestrum)
- Sinuses: draining sero-purulent discharge
- Histological picture: chronic inflammation

Sclerosis. Bone destruction, cavities, new bone formation, sequestrum

Clinical Picture
Symptoms:
- Recurrent bouts of pain, redness, tenderness, and fever
- Sinuses: old and new discharging


Radiology
Findings:
- X-ray: Rarefaction surrounded by sclerosis
- Cavities and sequestra (bacteria adheres to dead bone and escapes the antibiotic effect)
- Sclerosis. Bone destruction, cavities, new bone formation, sequestrum



Treatment
Approaches:
- Antibiotics: According to culture and sensitivity; culture from discharging sinus may not show all causative organisms
- Sinogram: to show extent
- Sequestrectomy and surgical debridement
- May use local antibiotic beads

Complications
Potential Outcomes:
- Recurrence & Recurrence & Recurrence
- Pathological fractures
- Growth disturbance
- Malignant transformation (Marjolin’s ulcer) of sinus
- Most commonly squamous cell carcinoma

Radiology
The initial radiographs are normal as bone changes are not visible until 10–14 days after the onset of infection.
X-ray is the recommended initial imaging modality because it is inexpensive and can rule out differential diagnoses.
The earliest signs on plain radiographs are soft tissue swelling and bone destruction in the metaphysis, with a Periosteal reaction.
The 99mTc radionuclide bone scan and MRI show changes within a day or two of the disease
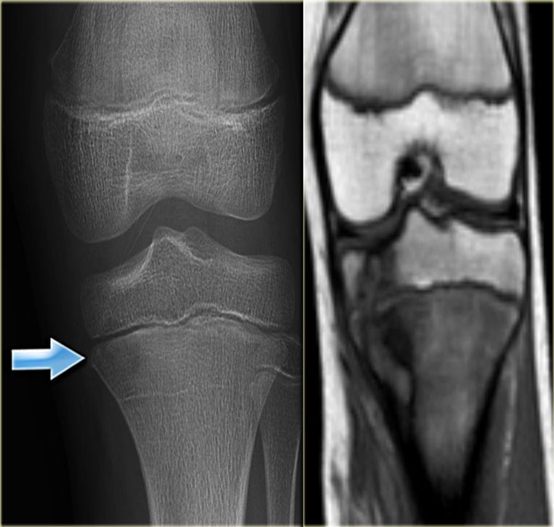
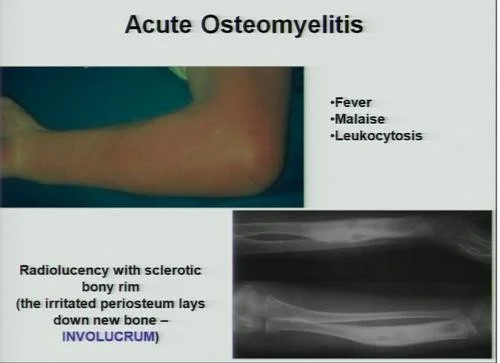
Compare X-ray and MRI in this case of acute osteomyelitis.
- It is difficult to be seen on plain x-ray.
- The extent of disease is well demonstrated by MRI
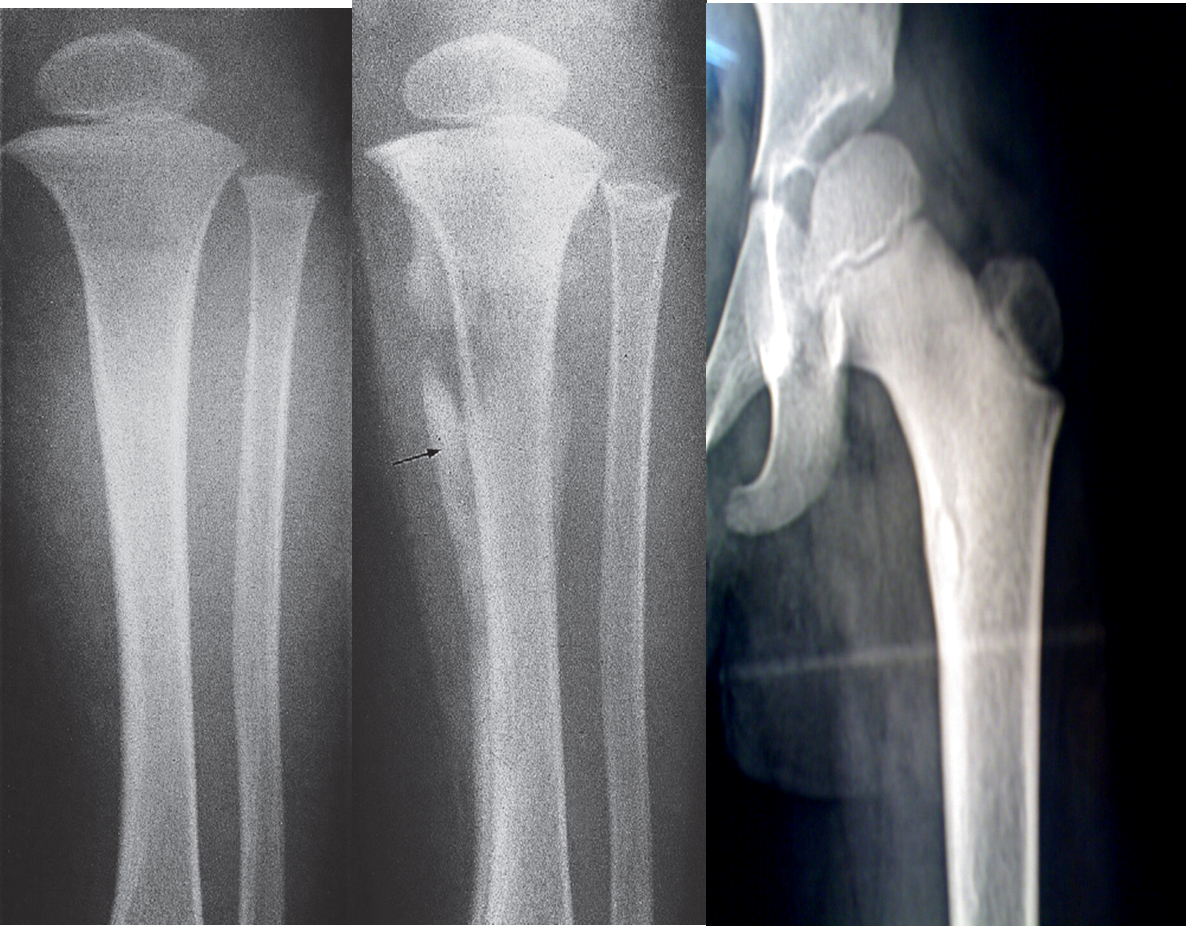 (A) An initial films reveals no abnormality
(A) An initial films reveals no abnormality
(B) A film taken 3 weeks later shows some destruction of the upper end of the tibia and an extensive periosteal reaction along the tibia, particularly the medial side (arrow).
(C) Bony sequestrum X-ray leg (left; AP view) of a child A fragment of bone has separated from adjacent bone and is surrounded by a lucent rim. chronic osteomyelitis.
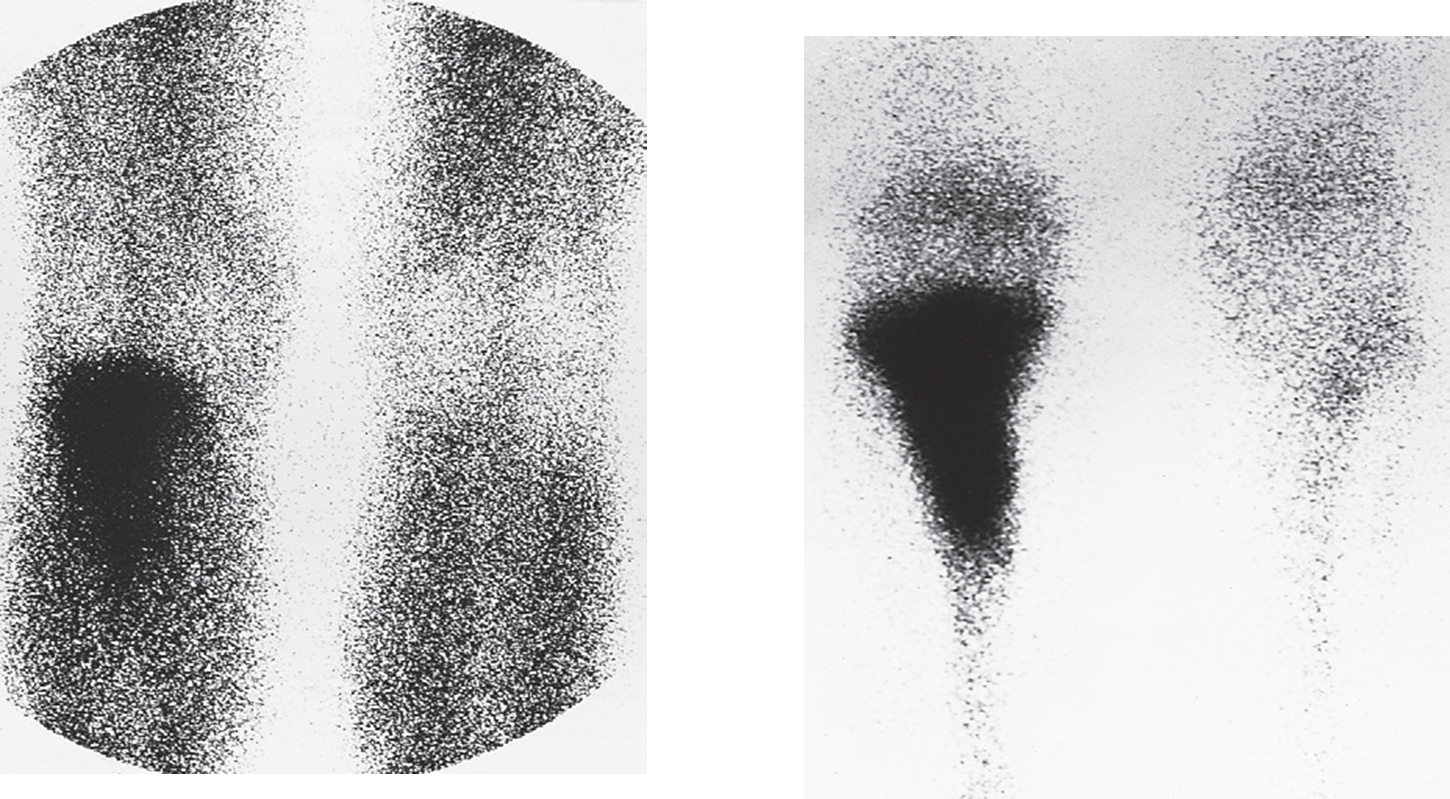 Osteomyelitis; radionuclide scans of knees.
(a) Scan taken 1 minute after injection of radionuclide showing increased uptake in the upper part of the leg.
(b) The delayed scan taken 3 hours later shows substantially increased uptake in the bone itself.
Acute osteomyelitis:
No abnormality on plain radiograph
Radionuclide study show high uptake
Osteomyelitis; radionuclide scans of knees.
(a) Scan taken 1 minute after injection of radionuclide showing increased uptake in the upper part of the leg.
(b) The delayed scan taken 3 hours later shows substantially increased uptake in the bone itself.
Acute osteomyelitis:
No abnormality on plain radiograph
Radionuclide study show high uptake
Spinal
PLAIN FILMS
- Narrowing and destruction of an intervertebral disk
- Paravertebral soft tissue mass
- Endplate sclerosis (during healing phase)
Spondylodiscitis (discitis-osteomyelitis)
X-ray lumbar spine (lateral view)
The inferior endplate of L2 and superior endplate of L3 are osteopenic and the cortices appear fragmented. The intervening L2–3 disc space is narrowed.

MRI
- Bone marrow edema in infected vertebrae, discs and paraspinal soft tissues
- Dark on T1 and bright on T2 images
- Enhancement of inflamed tissues after contrast
Spinal epidural abscess, osteomyelitis, and discitis MRI cervical spine (T2-weighted; sagittal plane) High signal intensity collections are seen in the posterior epidural space. The largest collection causes anterior displacement and compression of the spinal cord from C7-T2. The appearance is consistent with epidural abscess. High signal intensity consistent with osteomyelitis and discitis involves the C6 and C7
