Uterine Fibroids (Leiomyomas)
Definition
Uterine fibroids (leiomyomas) are:
- Benign, monoclonal smooth muscle tumors of the uterus that contain varying amounts of fibrous connective tissue.
- The most common pelvic tumors in women, are hormonally responsive, and may be asymptomatic or associated with symptoms such as heavy menstrual bleeding, pelvic pain, and infertility.
Pathogenesis
Step 1: Initiation of Fibroids
- Fibroids begin from one muscle cell in the uterus wall (myometrium).
- This cell undergoes a genetic change (mutation).
- The most common mutation is in the MED12 gene.
- Others include HMGA2 and some rare ones.
- Because of this mutation, that single cell starts multiplying → forming a clonal tumor (all cells come from one parent cell).
Step 2: Growth Due to Hormones
- Fibroids need hormones to grow:
- Estrogen → increases the number of progesterone receptors in the fibroid.
- Progesterone → the main hormone that makes the fibroid bigger, prevents cell death, and increases fibrosis (scar-like tissue).
- That’s why:
- Fibroids grow in reproductive years (high hormones).
- They shrink after menopause (low hormones).
- They enlarge in pregnancy (hormones high).
Step 3: Role of Growth Factors & Extracellular Matrix (ECM)
- Fibroid cells release growth factors like TGF-β (Transforming Growth Factor), IGF, EGF.
- These growth factors:
- Stimulate more cell division.
- Stimulate fibroblasts to make collagen and fibronectin → this builds up ECM.
- Result: fibroids feel hard, rubbery, and fibrotic.
Step 4: Local Environment & Blood Supply
- Fibroids create their own mini environment:
- Poor blood supply → relative hypoxia (low oxygen).
- This triggers VEGF (angiogenesis factor) to form new vessels.
- Local cytokines & inflammation keep the tumor alive and expanding.
✔ In short: Fibroids start from a genetic change in one muscle cell, then hormones (estrogen & progesterone) feed the growth, while growth factors and fibrosis make them enlarge and hard. That’s why they are hormone-dependent, benign tumors.
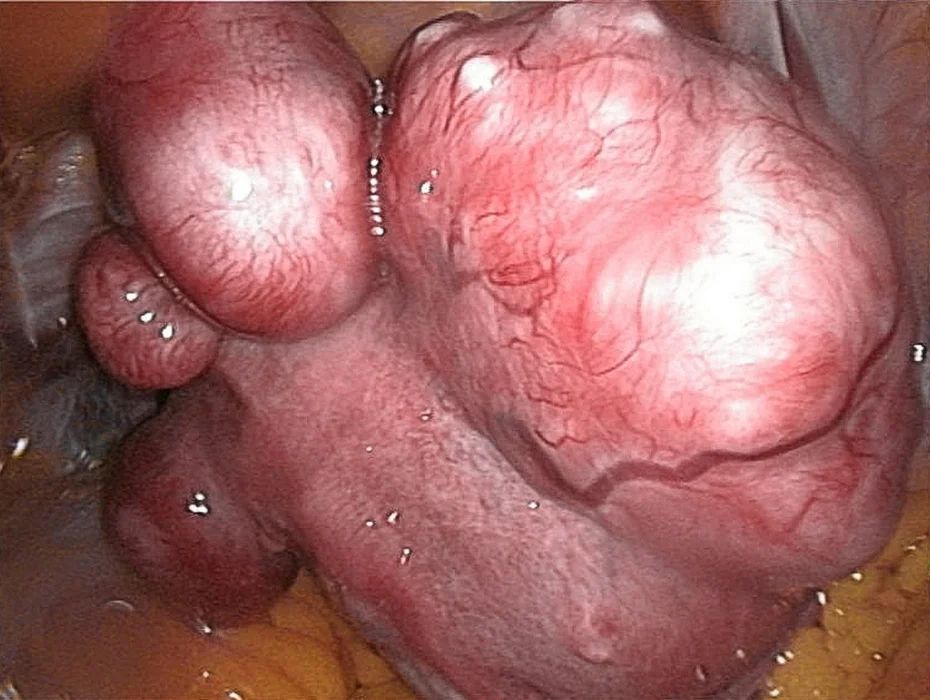
Types of Fibroids

Classification Based on Location
- Subserosal leiomyoma: located in the outer uterine wall beneath the peritoneal surface
- Intramural leiomyoma (most common): growing from within the myometrium wall
- Submucosal leiomyoma: located directly below the endometrial layer (uterine mucosa)
- Cervical leiomyoma: located in the cervix
- Diffuse uterine leiomyomatosis: The uterus is grossly enlarged due to the presence of numerous fibroids.
History
Demographic Data
- Name, Age (common in 30-50 years), Marital status, work.
Presenting Complaints
- Menstrual symptoms
- Heavy/prolonged bleeding
- Pressure symptoms
- Urinary frequency, urgency, retention (pressure on bladder).
- Constipation
- Abdominal lump or heaviness.
- Infertility, recurrent miscarriage, preterm labor.
- Pain
- Chronic pelvic pain
- Acute pain (red degeneration, torsion of pedunculated fibroid).
Past History
- Previous similar complaints.
- History of anemia, blood transfusions.
Obstetric & Gynecological History
- Menstrual history
- Obstetric history (number of pregnancies, outcomes).
- Contraceptive history.
Medical & Drug History
- Previous surgeries for fibroid or uterus.
- Diseases
- Medication
Family & Social History
- Family history of fibroids.
- Impact on quality of life (fatigue, social/sexual issues).
- Smoking, Alcohol
Examination
General Examination
- General appearance – pallor (anemia).
- Vital signs
- BMI/obesity.
- Signs of thyroid disease or other comorbidities.
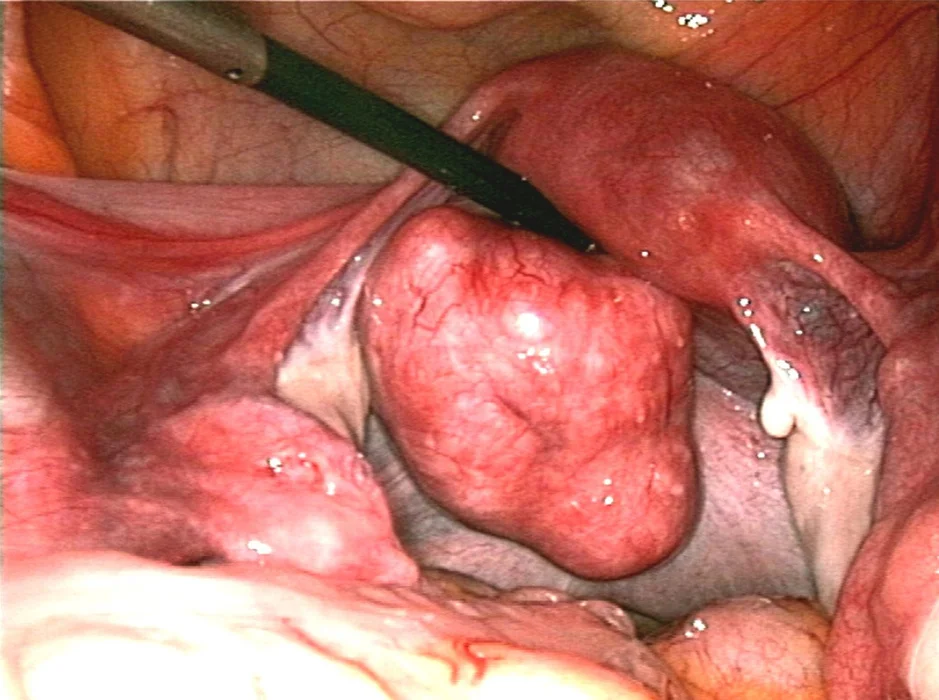
Abdominal Examination
- Inspection – lower abdominal swelling.
- Palpation
- Lump arising from pelvis, firm, irregular, nodular.
- Non-tender unless degeneration present.
- Mobile from side to side, but restricted mobility vertically.
- Cannot be pushed below pubic symphysis (uterine origin).
- Percussion – dull over lump, resonant around.
- Auscultation – usually silent (unless pregnancy).
Pelvic Examination
- Speculum: Cervix may be pulled up, irregular, or distorted.
- Bimanual palpation:
- Uterus enlarged, firm, irregular surface.
- Mass continuous with uterus.
- Mobility: mass moves with cervix.
Rectovaginal Examination
- To assess posterior fibroids and rectal involvement.
Differential Diagnosis of Uterine Leiomyoma
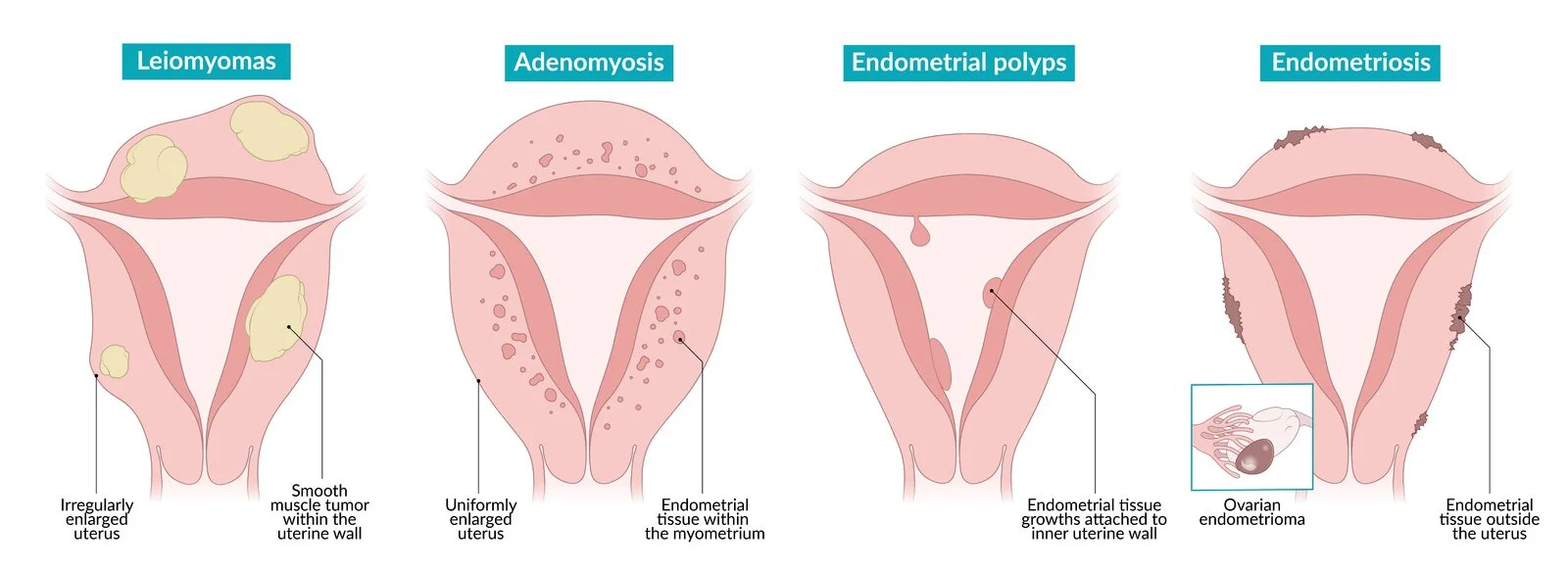
Related Conditions
Adenomyosis
- Definition: Benign condition where endometrial tissue is found within the myometrium.
- Risk factor: Early menarche, Nullipara
- Clinical features:
- Dysmenorrhea
- Abnormal bleeding
- Infertility (difficulty conceiving and increased risk of pregnancy loss)
- Uterine findings: Irregularly enlarged, firm
- Pathology:
- Endometrial glands and stroma within the myometrium.
Endometriosis
- Definition: Presence of endometrial tissue outside the uterus.
- Risk factor: Early menarche, Increased parity, Previous uterine surgery
- Clinical features:
- Dysmenorrhea
- Abnormal bleeding
- Menorrhagia
- Chronic pelvic pain
- Uterine findings: Typically, not enlarged
- Pathology:
- Endometrial glands and stroma outside the uterus.
Endometrial Polyps CC?
- Definition:
- Overgrowth of localized endometrial tissue attached to the inner wall of the uterus, usually benign
- Risk factor:
- Menopause, Obesity, Hypertension, Tamoxifen therapy, Lynch syndrome
- Clinical features:
- Abnormal bleeding
- Menorrhagia
- Postmenopausal bleeding
- Infertility/difficulty conceive
- Uterine findings: Typically, not enlarged
- Pathology:
- Pedunculated or sessile
- Single or multiple
- Length varies (up to many centimeters in size)
Uterine Leiomyosarcoma
- Definition:
- Rare malignant tumor arising from the smooth muscle cells of the myometrium
- Risk factor: Menopause & Tamoxifen use
- Clinical features:
- Symptoms similar to uterine fibroids
- Menstrual irregularities
- Postmenopausal bleeding
- Pelvic pain
- Uterine findings: Rapidly enlarging
- Pathology:
- Single lesions with areas of coagulative necrosis and/or hemorrhage
- Cords of polygonal cells with eosinophilic cytoplasm, abundant mitoses, and cellular atypia are common.
Pharmacotherapy for Uterine Leiomyoma
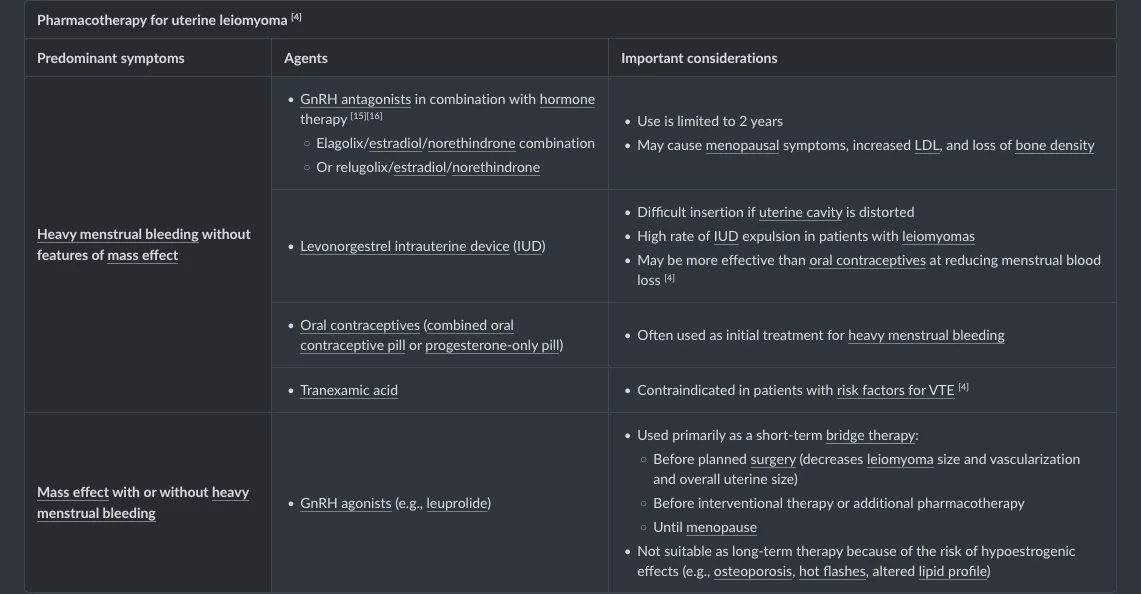
Uterine Fibroids