Pediatrics-2
SYSTEMIC LUPUS ERYTHEMATOSUS (SLE)
Childhood-Onset Systemic Lupus Erythematosus (cSLE)
- Definition: Chronic, multisystemic, autoimmune disease characterized by widespread inflammation of blood vessels/tissues and presence of autoantibodies (esp. ANA).
- Pathophysiology:
- Genetic, hormonal, immunologic, environmental factors.
- Monogenic forms: Unique to cSLE (defects in complement, type I interferon pathway, aberrant nucleic acid repair, abnormal B cell development).
- Mediated by antibody formation and immune complexes.
- Key Points:
- ANA is not sufficient to diagnose SLE.
- Few systems may be involved for years prior to full outbreak.
Epidemiology
- Gender: cSLE affects Girls > Boys (8:1).
- Age: 10-20% of all SLE cases. Rare <5 years; common after first decade.
- Severity (cSLE vs Adult SLE):
- cSLE in young children (<10y) is more severe with poorer prognosis.
- More common in cSLE: Fever, lymphadenopathy, hematologic abnormalities, lupus nephritis (LN), pericarditis, neuropsychiatric symptoms, ocular symptoms.
- More common in aSLE: Raynaud phenomenon, pleuritis, subacute cutaneous lupus, discoid lupus, sicca symptoms.
- Demographics: More frequent/severe in Asian, African, and Hispanic children.
Clinical Presentation
- Onset: Usually gradual (low grade fever, weight loss, myalgia, fatigue, arthralgia, LAD) over months.
- Acute Onset: May present with MAS, severe kidney disease, neuropsychiatric manifestations, thromboembolic disease, or TTP.
- Delays: Diagnosis may be delayed by overlooking signs like nonpainful small joint arthritis, kidney disease, or classic malar rash (in darker skin).
- Organ Involvement: Major organs typically involved within first 2-3 years.
Frequency of Manifestations
- Constitutional (20-90%): Fever, fatigue, anorexia, weight loss, lymphadenopathy.
- Mucocutaneous (60-80%): Malar rash, alopecia, photosensitivity, ulcers, discoid rash.
- Musculoskeletal (61-64%): Arthritis, arthralgia, myositis.
- Hematologic (55-77%): Anemia, lymphopenia, leukopenia, thrombocytopenia.
- Renal (27-59%): Proteinuria, hematuria, casts, LN, nephrotic syndrome.
- Serositis (20-30%): Pleural/pericardial effusion, symptomatic pleuritis/pericarditis, peritonitis.
- Neuropsychiatric (5-30%): Headache, psychosis, cognitive dysfunction, seizure, acute confusional state.
1. Mucocutaneous Involvement (60-80%)
- Malar Rash (Butterfly): Crosses nasal bridge, spares nasolabial folds. Often affects chin/ears. May be hypopigmented in darker skin.
- Discoid Lupus Erythematosus (DLE): (See image)
- Other: Photosensitivity, diffuse maculopapular rash, cutaneous vasculitis, oral/nasal ulcers.
- Alopecia: Nonscarring thinning (esp. frontotemporal). Diffuse alopecia less frequent.

 (Left: Discoid Lupus Rash. Right: Malar Rash)
(Left: Discoid Lupus Rash. Right: Malar Rash)


2. Hematologic Abnormalities (55-77%)
- Anemia (HB <12g): 50-75%. Types: IDA, Coombs-positive AIHA, anemia of chronic disease.
- Leukopenia (WBC <4,000): 70%. Mainly lymphocytopenia. Neutropenia is uncommon.
- Thrombocytopenia: 10-50% (Usually mild).
- ITP: May precede cSLE diagnosis by months/years.
- TTP: Rare pentad (Fever, thrombocytopenia, neurologic, renal, microangiopathic hemolytic anemia). Antibody to vWF-cleaving protease.
- Antiphospholipid Antibodies (aPLs): Assoc. with thrombocytopenia, prolonged PTT, menorrhagia, thrombosis, stroke.
3. Musculoskeletal Findings (61-64%)
- Arthritis/Arthralgia: Most common findings. Affects large and small joints, not always painful.
- Myositis: Muscle pain or weakness (Proximal > Distal).
- Bone: Osteopenia, osteoporosis, osteonecrosis (avascular necrosis). Low BMD frequent at diagnosis, does not improve even when steroids stopped.
4. Renal Involvement (27-59%)
- Significance: Determines prognosis. More frequent/early in children.
- Presentation:
- Mostly asymptomatic hematuria, proteinuria (70%).
- Lupus nephritis (LN) and nephrotic syndrome (30-40%).
- Can range from routine findings to Acute Kidney Injury (AKI).
- Associations: Low complement levels, anti-dsDNA antibodies. Z
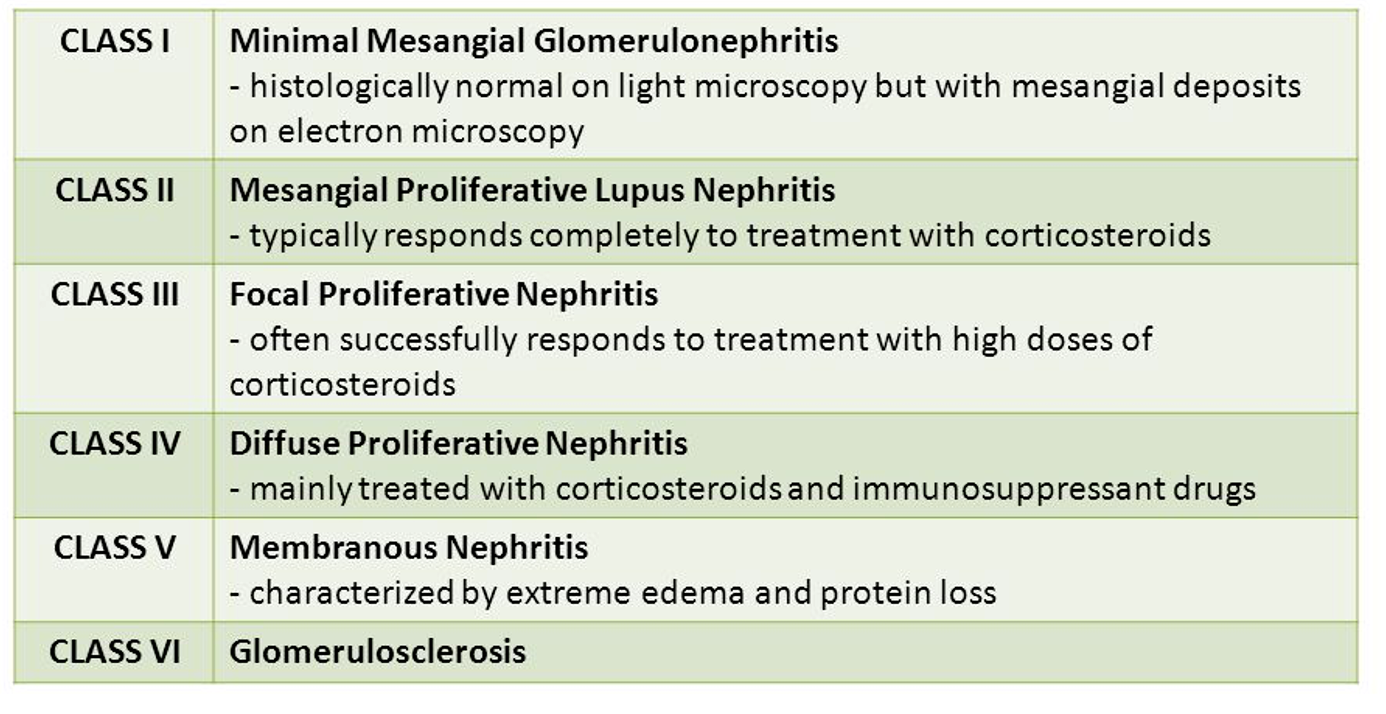
- Classification: Based on histopathology.
5. Neuropsychiatric Manifestations (5-30%)
- Can present subacutely over weeks to months.
- Most Common: Intractable migraine headaches, Cognitive disturbances (school deterioration), Seizures, Stroke, Mood/anxiety disorders, Psychosis, depression, social isolation.
- Less Common: Acute confusional state, Peripheral neuropathy, Cranial nerve palsy, Chorea (movement disorders), Cerebritis, dementia, coma, Transverse myelitis, Aseptic meningitis.
- Note: Must rule out infection, metabolic, primary psych, medication side effect.
6. Pulmonary Complications (30-50%)
- Pleuritis (35%): Sharp (“stabbing”) chest pain, severe, localized, exacerbated by deep inspiration. SOB rare. CXR shows fluid. Elevated CRP.
- Subclinical: Restrictive disease/reduced diffusion capacity on PFTs (60-70%).
- Pulmonary Hemorrhage (<5%): Fever, cough, pallor, tachypnea, epistaxis, hemoptysis.
- Pulmonary Hypertension (<2%): Severe, multiple thromboses, multifactorial.
7. Cardiac and Vascular (12-54%)
- Pericarditis: Most common cardiac abnormality (esp. first 6 months).
- Myopericardial: 4-fold higher in cSLE than aSLE.
- Rare: Myocarditis, valvular disease (endocarditis), Coronary Artery Disease (CAD).
- Heart Failure: Usually result of kidney or pulmonary compromise.
- Vasculitis: Small-vessel (petechial rash, digital ulcerations, urticarial vasculitis). In organs (lungs, CNS, retina, GIT, kidneys) leads to hemorrhage/damage.
- Thromboembolic: 10%. Assoc. with aPLs.
- Raynaud phenomenon: Rare.
8. Gastrointestinal (20%)
- Peritonitis: Distinguish from peritonitis 2° to nephrotic syndrome/pancreatitis.
- Pancreatitis: Acute is uncommon.
- Liver:
- Asymptomatic mild hepatitis (Enzymes 2-3x normal) frequent at onset.
- Autoimmune Hepatitis (AIH): May precede cSLE. ASMA+. Hepatomegaly may differentiate.
9. Ophthalmologic
- Common: Asymptomatic cotton-wool spots (microangiopathic retinopathy), often in LN patients.
- Rare: Keratoconjunctivitis sicca (dry eyes), Vaso-occlusive retinopathy/retinal vasculitis (acute vision loss), Episcleritis, scleritis, symptomatic uveitis.
- Steroid Effects: Subcapsular cataracts, glaucoma.
Major Laboratory Findings & Autoantibodies
- General: High ESR/CRP, Cytopenias, Hematuria/Proteinuria/Casts, Low C3/C4, Vitamin D deficiency.
- Autoantibodies:
- ANA (Antinuclear Antibodies): 100%, including extractable nuclear antigens antibodies ( ENAs) , double-stranded deoxyribonucleic acid (dsDNA) antibodies, and antiphospholipid antibodies (aPLs).
- Anti-dsDNA: High specificity. Monitor disease activity. Assoc. with renal disease, drug-induced lupus. Rare in other disorders. Z
- Anti-Sm (Smith): High specificity. Not uniformly present. Assoc. with Chronic active disease.
- Anti-Ro (SSA) / Anti-La (SSB): 30%. Assoc. with Photosensitivity, Neonatal Lupus, Sjogren’s. (dry mouth, dry eyes, parotitis )
- Antiribosomal P antibodies: antibodies are associated with active disease, particularly neuropsychiatric, renal, or hepatic involvement and more frequently cSLE.
- Antiphospholipid (aPLs): Lupus Anticoagulant – Anticardiolipin and anti-beta2GPI . are associated with thrombocytopenia, menorrhagia, Prolonged aPTT , thrombosis, and stroke
- Histone: Drug-induced lupus.
All of these autoantibodies may also be found in children who do not fulfill classification criteria for SLE. Some of these children will go on to develop SLE, others will develop other rheumatic diseases, and some will remain asymptomatic
Diagnosis & Differential
- Diagnosis:
- Based on clinical judgment after excluding alternatives.
- Suspect in any child with gradual onset fever, anorexia, weight loss, fatigue + persistent symptoms.
- Suggestive: Malar rash, polyarthritis, serositis, nephritis, discoid rash, alopecia, LAD, edema, neuro symptoms.
- Labs: Persistent thrombocytopenia, hemolytic anemia, lymphopenia, leukopenia. Serology supports.
- Differential Diagnosis:
- Viral: EBV, CMV.
- Malignancy: Acute lymphoblastic leukemia(ALL).
- Rheumatic: MCTD, Dermatomyositis, Scleroderma, Polyarteritis nodosa, RA (if anti-dsDNA present).
- Other: Autoimmune thyroid disease (hashimotos_, Celiac, Myasthenia gravis, Antiphospholipid syndrome.
Treatment & Management
Goals
- Ensure long-term survival.
- Achieve lowest possible disease activity.
- Prevent organ damage.
- Minimize drug toxicity.
- Improve quality of life.
- Patient/Family education.
Psychosocial Aspects
- Care of children/adolescents is distinct.
- Steroids: High doses impact growth and appearance (short stature, osteonecrosis), causing psychological devastation.
- Suicide: Attempts (eg, surreptitious refusal to take necessary medications) are well recognized
Pharmacotherapy
- Mild SLE (No life-threatening organ involvement):
- NSAIDs: Arthritis, pleuritis.
- Hydroxychloroquine: Skin, arthritis, prevent flares (may decrease mortality).
- Prednisone: Low-dose.
- Moderate and Severe SLE:
- Steroids: Intermittent IV high-dose methylprednisolone (Pulse) / High dose alternate-day oral.
- Hydroxychloroquine.
- Immunosuppressants: Mycophenolate mofetil, Azathioprine.
- Cyclophosphamide (IV).
- Biologics: Rituximab.
Supportive Therapy
- Sun protection: SPF 30 or greater.
- Cardiovascular: Manage Hypertension, Hyperlipidemia, Preventive cardiology.
- Bone: Osteoporosis prevention.
- Immunization: Influenza, Pneumococcus.
Course & Prognosis
- Pattern: Exacerbations and remissions or chronic active disease.
- Survival: 10-year survival rate is 90% (Mortality <10%).
- Causes of Death:
- Early: Active disease (Renal, CNS, Vasculitis), Infection.
- Late: Coronary artery disease.
- Morbidity: Organ/tissue damage in 60%. Growth failure in 30% (Poor in black, male).
- Causes of Unsatisfactory Outcome: Poor adherence, Neuro complications (encephalopathy), Intercurrent infections, Renal disease (diffuse proliferative GN), CV disease, Failure to refer to experienced center.
NEONATAL LUPUS (NL)
Definition
- Passively acquired autoimmune disease occurring in offspring of mothers with anti-Ro (SSA) and/or anti-La (SSB) or RNP antibodies.
Clinical Manifestations
1. Cardiac (Most Serious)
- Heart Block (HB): Congenital Heart Block (CHB). 1st, 2nd, and 3rd degree.
- Diagnosed in utero/neonatal period.
- Risk: 2% for first pregnancies.
- Timing: Commonly 18-24 weeks gestation.
- Presentation: Fetal bradycardia (Advanced 2nd/3rd degree).
- Sinus Bradycardia (<100 bpm): 3%. Not permanent, good prognosis if no EFE/Ventricular dysfunction.
- Cardiomyopathy: in isolation or with CHB ,associated with an increased risk of fetal/neonatal death.
- Screening: Weekly pulsed-Doppler fetal echo from the 18th -26th week of pregnancy is often advised in mothers with autoimmune disease who screen positive for anti-Ro and/or anti-La antibodies
2. Cutaneous (Rash)
- Erythematous annular lesions or macules with slight central atrophy and raised active margins.
- Location: Primarily scalp and periorbital area (“Owl-eye” appearance), sometimes palms/soles/diaper area.
- Prognosis: Self-limiting. Resolves by 6-8 months (maternal IgG half-life 25 days).
3. Other Manifestations
- Hepatic: Asymptomatic elevated enzymes, mild hepatosplenomegaly, cholestasis, hepatitis.
- Hematologic: Anemia, neutropenia, thrombocytopenia, rare aplastic anemia.
- Neurologic: Hydrocephalus, macrocephaly.
- Radiographic: Stippling of epiphyses (Chondrodysplasia punctata).
Diagnosis
Is made when the following are both present::
- The mother has anti-Ro, anti-La, or anti-ribonucleoprotein (RNP) antibodies.
- The fetus or newborn develops HB, or the newborn develops the typical rash or hepatic or hematologic manifestations in the absence of another explanation
Management
- In Utero:
- Complete HB: , is irreversible despite all therapies attempted to date, including glucocorticoids, IVIG and Hydroxychloroquine
- 2nd-degree HB: May be reversible.
- Postnatal management:
- Complete HB: Some infants require insertion of a cardiac pacemaker, if the HR at delivery is less than 55 (bpm).

 (Left: Neonatal Lupus Rash. Right: Clinical appearance)
(Left: Neonatal Lupus Rash. Right: Clinical appearance)
-1769504641356.webp)
-1769504655490.webp)
IM
Dr.waqar
Definition of autoimmune disease
Autoimmune diseases are conditions in which antibodies are formed against the person’s own body tissues In some diseases, ab. are formed against one organ only ( DM type1, Grave’s disease) while in others, ab. are formed against many tissues
DEFINITION OF SLE
SLE is an autoimmune disease in which antibodies are formed against many tissues of the body ( multisystem disease). These antibodies cause damage and inflammation in the tissues.
EPIDEMIOLOGY
- Geographics : Occurs worldwide
- Gender : F:M ratio is 9:1 ( usually young women, aged 20 to 40).
- Race : More in black Americans
ETIOLOGY
Like most autoimmune diseases, cause is unknown but some associations are observed:
- If one twin is affected, more chances in the other ( ? Genetic role)
- More chances in 1st degree relatives
- More chances in premenopausal women ( ? may be hormonal cause)
- Some drugs can cause SLE like picture: INH; TB Hydralazine; antihypertensive; pregnancy Penicillamine
S/S
S/S of SLE are “very” varied & may be mild to severe. SLE can affect any organ BUT REMEMBER 3 MOST COMMON FEATURES Fatigue & malaise Muscle & joint pain Fever
- 1) Gen. features: Fatigue, fever, wt loss
- 2) Joint & Muscles:
*Pain in small joints of hands ( like R.A.) * Other joints may also be affected * Usually no joint swelling * Myalgias - 3) Scalp: hair fall, discoid alopecia
- 4) Brain: cerebritis, psychosis, depression
- 5) Eyes: Retinal infarcts, scleritis
- 6) Mouth: Ulcers
- 7) Skin rash: Skin is affected in 85% patients Butterfly rash Discoid rash Butterfly rash is characteristic of SLE SLE rash gets worse in sunlight (photosensitive)
Sometimes discoid skin lesions are seen

SKIN RASH IN SLE ⇒ Butterfly rash on the face a) involves the cheeks, b) crosses over the nasal bridge c) no involvement of the nasolabial fold d) May be slight pain or HAKKA
-
8) Lungs:
- pleuritis, pleural effusions
- Interstitial lung disease
-
9) Heart: * Pericarditis * Myocarditis
- Non bacterial endocarditis of the mitral valve ( Libman-Sacks endocarditis)
- Increased risk of coronary artery disease (angina, MI)
-
10) Raynaud’s phenomenon:
-
11) Kidneys( Lupus nephritis) : SLE causes various types of glomerulonephritis which present as either nephrotic syndrome or nephritic syndrome. W.H.O. has classified lupus nephritis into 6 classes based on histology of the renal lesion (class 1 to 6).
-
Class 4: Most common renal lesion in SLE & causes nephritic syndrome called diffuse proliferative (GN) or Membrano-proliferative GN (MPGN)
-
Class 5: Also called Membranous nephropathy (MN). Causes nephrotic syndrome. SLE NEPHRITIS HAS HIGH MORBIDITY & MORTALITY
-
WHO class of Lupus Nephritis
1) Routinely check urine in SLE patients. If any
blood or protein, investigate further ( biopsy)
2) Treatment of lupus nephritis depends on the
class of lesion which is present, so biopsy is
important.
- 12) GIT: Vasculitis of the intestinal vessels causing bowel infarction
- 13) Blood vessels: Vasculitis anywhere
- 14) BLOOD:
- Anemia
- Low WBC
- Low platelets (antibodies are formed against RBC, WBC & platelets)
INVESTIGATIONS
- CBC : *Anemia * Low WBC * low plts.
- Urea/creatinine :
- Raised in advanced renal disease ( lupus
nephritis)
- Raised in advanced renal disease ( lupus
- **3) Urine : ** * may show proteins & blood
- 4) ESR: Raised in acute flare
- 5) C3, C4 (complements) : reduced in acute flare & lupus nephritis
- 6) Autoantibodies : Important ones are : a) ANA (antinuclear ab.) : Present in almost all pts. Not specific for SLE but done as the first screening step. Titers should be at least 1:80 ( if ANA negative, SLE is ruled out)
Done only if ANA is positive
b) Anti double stranded DNA ( anti ds DNA) ( * v. specific for SLE - Present in 70% pts., only specially during acute flare)
c) Anti Sm ab. : most specific
d) Anti Ro, anti La
- **7) Renal Biopsy : **
- Done if nephritis is suspected ( abn. urine)
- Shows the class of renal disease, which helps us decide about drugs
WHEN TO SUSPECT SLE
- Consider SLE in a female with multisystem symptoms
- Confirm with blood tests
- Rheumatology consultation for all patients
Points about drug induced Lupus
- No CNS, renal or major organ involvement
- ANA & anti-histone ab. positive
- Can occur even years after starting the drug
- Resolves after stopping the drug
- Common symptoms -⇒ fever, arthralgias, myalgias, mild pleuritis
DIAGNOSTIC CRITERIA
American College of Rheumatology has 11 criteria, at least 4 of which should be present to diagnose SLE. BUT These criteria were meant to enroll patients in clinical trials, not to diagnose individual patients.
TREATMENT
THERE IS NO CURE FOR SLE Drugs used:
- Hydroxychloroquin; rheumatology, protective, malaria
- NSAIDs; as needed
- Glucocorticoids;
- Immunosuppressive drugs; ( Cyclophosphamide, Mycophenolate mofetil, Methotrexate, Azathioprine).Used for long term control of the disease.
- Belimumab (a monoclonal antibody)
Hydroxychloroquin is given long term to almost all symptomatic patients. For mild symptoms, this is enough.
In case of moderate to severe symptoms or major organ involvement, steroids, immuno-suppressives & /or monoclonal antibodies are added
-
**Fatigue, arthralgias, fever, pleuritis **
- Hydroxychloro;Can cause retinal toxicity, so regular eye checks
- NSAIDs
-
Skin rash:
- Topical steroids
- Sunscreens
- Hydroxychloroquin tabs.
- Sometimes, oral steroids may be needed
-
Avoid long sun exposure ( SLE gets worse in sun)
-
Periods of rest during acute flares
Treatment of Nephritis
- Steroids
- Immunosuppressives (eg Mycophenolate, azathioprine, methotrexate, cyclophosphamide)
- Sometimes, monoclonal antibodies are also added.
- Treatment may be long term
The following features in SLE also need aggressive treatment with steroids/ immunosuppressants: a) Cerebritis b) Anemia, low WBC, low platelets
COURSE OF SLE
Most patients have relapsing-remitting course
Features of an acute flare:
- Worsening of signs/symptoms
- Rise in ESR
- Fall in blood complement levels (C3, C4)
- Further rise in anti-ds-DNA ab. levels
PROGNOSIS
- Mortality has fallen dramatically in the last 50 yrs due to advanced Rx.
- 10 yr survival rate is 90%
- Causes of death :
- Coronary artery disease: No. 1 cause of death
- Renal disease
- CNS disease
- Autoimmune hemolytic anemia
PREGNANCY & SLE
- Fertility is normal but increased chances of miscarriage and fetal death
- SLE is not a contraindication to pregnancy but tell the patient about the risks
- Exacerbations can occur during pregnancy & even after delivery
- Corticosteroids, azathioprine & hydroxychloroquine are safe in preg.
There is no increased risk of neonatal lupus related to breastfeeding. However, some medications enter breast milk: Nonsteroidal antiinflammatory drugs (NSAIDs) can be used, but high-dose aspirin should be avoided. Prednisone can be taken.
RAPID FIRE QUESTIONS
-
Most common symptoms of SLE?
- Fatigue
- Joint pain
- Skin rashes
- Fever
-
Most common rash?
- Malar rash (butterfly rash)
-
Features of the most common rash?
- Erythematous
- Involves the cheeks and bridge of the nose
- Spares the nasolabial folds
-
Treatment of the rash?
- Topical corticosteroids
- Sun protection
-
Features in the heart?
- Pericarditis
- Libman-Sacks endocarditis
-
Which antibiotic to use in SLE endocarditis?
- Typically, antibiotics are not used; treatment focuses on managing SLE with immunosuppressants.
-
Features in the brain & lungs?
- Brain: Seizures, psychosis
- Lungs: Pleuritis, interstitial lung disease
-
What happens during pregnancy?
- Increased risk of complications such as preeclampsia, preterm birth, and fetal loss
-
Commonest cause of death in SLE?
- Cardiovascular disease
- Infections
-
Treatment of renal SLE?
- Immunosuppressants (e.g., corticosteroids, cyclophosphamide)
- ACE inhibitors or ARBs for proteinuria
-
Which drug to be given to all SLE patients?
- Hydroxychloroquine
-
Which drugs can cause SLE?
- Procainamide
- Hydralazine
- Isoniazid
-
Any 2 features of acute flare?
- Fever
- Worsening of rash or joint pain
CASE 1
A 35 year old lady presents with pain and swelling in the right lower leg since 2 days. Past history of recurrent abortions Had a stroke 2 years ago Also had popliteal artery thrombosis few years ago
APA Syndrome
Some patients with SLE have a condition called Antiphospholipid antibody syndrome ( APA syndrome, APLS)
It is an autoimmune condition where there are some abnormal antibodies in the blood, which cause thrombosis in blood vessels. Thrombosis can occur anywhere in the body (arteries or veins)
Dermatology
The “butterfly” rash
Butterfly rash: think rosacea or seborrheic dermatitis first
- Many facial rashes are described as “malar” or “butterfly” rashes
- Most “butterfly” rashes are seborrheic dermatitis or rosacea, not lupus, which is classically described as “malar” or “butterfly”

The “butterfly rash” of lupus




Key elements of facial lupus rash
-
Four SLE criteria are dermatologic:
- Photosensitivity
- Discoid lesions
- Oral ulcerations
- Malar rash
-
Photodistributed
-
Often scaly, scarring
-
Spares nasal creases (unlike seborrheic dermatitis)
-
May mimic rosacea
-
Refer these patients
