Managements
-
Non-pharmacological:
-
Understanding asthma — The patient and family should understand the characteristics of asthma, the principles of effective treatment, the effects of various medications, and the resources available.
Avoid Your Triggers
- Use your air conditioner.
- Decontaminate your décor Maintain optimal humidity
- Prevent mold spores.
- Reduce pet dander
- Clean regularly.
- Cover your nose and mouth if it’s cold out
Stay Healthy
➤ Taking care of yourself and treating other conditions linked to asthma will help keep your symptoms under control. For example:
- Get regular exercise.
- Maintain a healthy weight.
- Eat fruits and vegetables.
- Control heartburn and gastroesophageal reflux disease (GERD).
The Long-term Goals of Asthma Management
- Control asthma symptoms (cough, wheezing, or shortness of breath)
- Infrequent and minimal use (≤2 days a week) of reliever therapy
- Maintain (near) normal pulmonary function
- Maintain normal exercise and physical activity levels
- Prevent recurrent exacerbations of asthma, and minimize the need for emergency room (ER) visits or hospitalizations
- Optimize asthma control with the minimal dose of medications
- Reduce mortality
- Optimize quality of life
Pharmacological Management in Adults and Adolescents
The SINA panel recommends asthma treatment to be based on the following phases:
-
Initiation of treatment
-
Adjustment of treatment
-
Maintenance of treatment.
-
At each phase, the patient is recommended to have a clinical assessment that includes symptoms assessment by ACT – Then the patient can be placed on appropriate treatment Step.
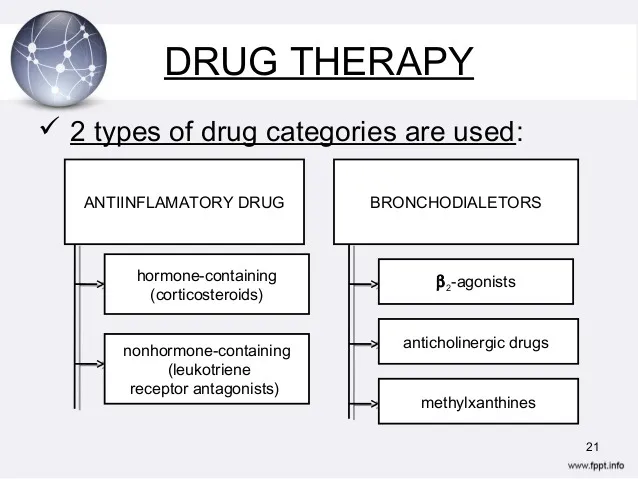
Drug Therapy
- 2 types of drug categories are used:
- Anti-inflammatory drugs
- Hormone-containing (corticosteroids)
- Non-hormone-containing (leukotriene receptor antagonists)
- Bronchodilators
- β₂-agonists
- Anticholinergic drugs
- Methylxanthines
- Anti-inflammatory drugs
Management - Pharmacological:
-
β2-Agonists
- Are the most effective bronchodilators available.
- This results in smooth muscle relaxation, mast cell membrane stabilization, and skeletal muscle stimulation.
-
Short-acting agents: Albuterol, levalbuterol or pirbuterol
-
Long-acting agents: Salmeterol, formoterol and arformoterol
Anticholinergics
- Ipratropium bromide and tiotropium bromide are competitive inhibitors of muscarinic receptors; they produce bronchodilation only in cholinergic mediated bronchoconstriction.

Corticosteroids
-
Corticosteroids increase the number of β2-adrenergic receptors and improve receptor responsiveness to β2-adrenergic stimulation, thereby reducing mucus production and hyper-secretion, reducing BHR, and reducing airway edema and exudation.
-
Systemic toxicity of inhaled corticosteroids is minimal with low to moderate inhaled doses, but the risk of systemic effects increases with high doses.
-
Local adverse effects include oropharyngeal candidiasis and hoarseness of voice.
Leukotriene Modifiers:
Zafirlukast (Accolate) and montelukast (Singulair) are oral leukotriene receptor antagonists that reduce the pro-inflammatory (increased microvascular permeability and airway edema) and bronchoconstriction effects of leukotriene D4.
- In adults and children with persistent asthma, they improve:
- Pulmonary function tests,
- Decrease nocturnal awakenings, and
- β2-agonist use,
- Improve asthma symptoms.
Omalizumab
-
Omalizumab (Xolair) is an anti-IgE antibody approved for the treatment of allergic asthma not well controlled by oral or inhaled corticosteroids.
-
Because of its high cost, it is only indicated as step 5 or 6 care for patients who have allergies and severe persistent asthma that is inadequately controlled with the combination of high-dose inhaled corticosteroids and long-acting β2-agonists.
-
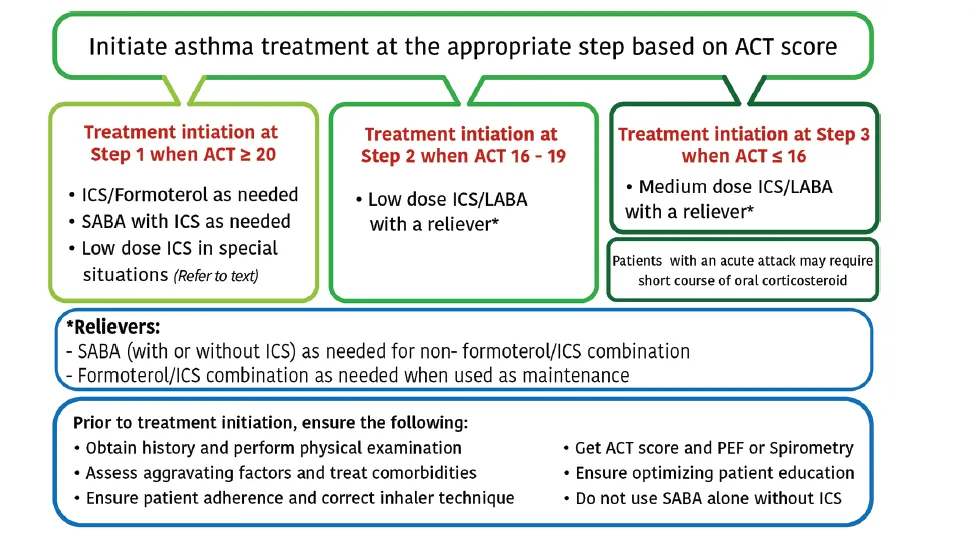
Treatment initiation at Step 1 when ACT ≥ 20
- Low Dose ICS/Formoterol as needed or LABA
- SABA with ICS as needed
- Low dose ICS in special situations (Refer to text)
-
Treatment initiation at Step 2 when ACT 16 - 19
- Low dose ICS/LABA with a reliever
-
Treatment initiation at Step 3 when ACT ≤ 16
- Medium dose ICS/LABA with a reliever
- Patients with an acute attack may require a short course of oral corticosteroid
- Medium dose ICS/LABA with a reliever
Relievers:
- SABA (with or without ICS) as needed for non-formoterol/ICS combination
- Formoterol/ICS combination as needed when used as maintenance
Prior to treatment initiation, ensure the following:
- Obtain history and perform physical examination
- Assess aggravating factors and treat comorbidities
- Ensure patient adherence and correct inhaler technique
- Get ACT score and PEF or Spirometry
- Ensure optimizing patient education
- Do not use SABA alone without ICS
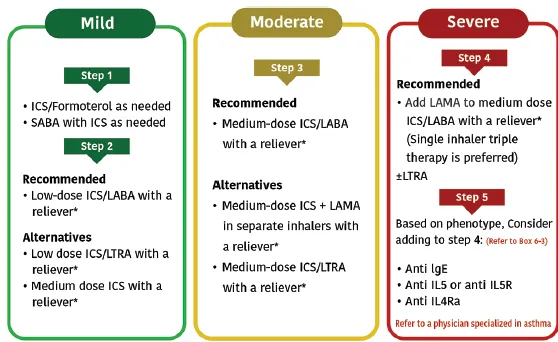
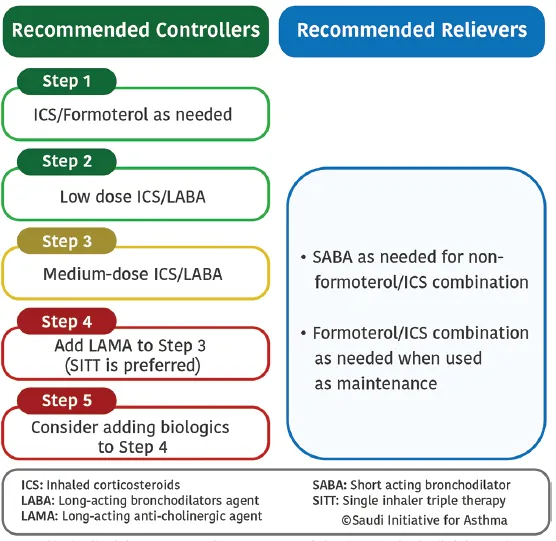
Treatment at step 1
- Symptoms are usually mild and infrequent,
- (usually < twice a week) with an ACT score of ≥20 points and no risk factors for asthma exacerbations.
- At this step, SABA alone on an as-needed basis is not anymore recommended.
- Recommended option: It is recommended to use ICS/formoterol on an as-needed basis (Evidence A).
Treatment at step 2
- Recommended options: It is recommended to use a daily fixed-dose combination of low-dose ICS/LABA with an as-needed reliever for symptom relief (Evidence A).
- Alternative options:
- The addition of LTRA to a low-dose ICS is another option, especially in patients with concomitant rhinitis (Evidence A).
Treatment at step 3
-
Recommended options: The fixed-dose combination of medium-dose ICS/LABA was found to improve asthma control and reduce asthma exacerbations for patients whose asthma is not controlled at step 2 (Evidence A).
-
Alternative options: Evidence has shown that when tiotropium is added to an ICS delivered by multiple inhalers; it improves symptoms, reduces the risk of exacerbation, and improves lung function in patients with inadequately controlled asthma.
Treatment at step 4
- Recommended options:
- Add LAMA in a single inhaler is recommended (Evidence A). This novel approach of SITT was found to be a safe and effective therapeutic approach. Moreover, when compared to multiple inhalers triple therapy (MITT), SITT usage is cost-effective and is associated with better adherence.
- Once-a-day SITT combination of fluticasone furoate/umeclidinium/vilanterol 200/62.5/25 µg (Trelegy Ellipta®) is a recommended option.
Treatment at step 5
-
Early consideration of biological therapy may lead to clinical remission and save the patient from frequent or chronic use of OCS and reduce asthma exacerbations.
-
Consultation with an asthma specialist is strongly recommended.
-
Available biological agents like:
- Anti-IgE therapy: Omalizumab
- Anti-IL 5 therapy: Mepolizumab
Criteria for Admission
-
Patients whose peak flow is ≥ 60% best or predicted one hour after initial treatment can be discharged from the emergency department.
-
Criteria for admission:
- Any feature of a life-threatening, near-fatal attack
- Any feature of a severe attack that persists after initial treatment.
- unless any of the following is present:
- Still suffering from significant symptoms
- Previous history of near-fatal or brittle asthma
- Concerns about compliance and pregnancy
Referral to a Specialist Center
- Status asthmatics
- Deteriorating PEF
- Persisting or worsening hypoxia
- Hypercapnea, respiratory acidosis (pH <7.3)
- Severe exhaustion
- Increase work of breathing
- Drowsiness
- Confusion
- Coma
- Respiratory arrest
Complications
- Airway remodeling
- Hospitalization
- Lifestyle disruption
- Sleep
- Physical activity
- Productivity
- Death
Management of Acute Asthma in Adults and Adolescents
-
Acute asthma exacerbation is a challenging clinical scenario that requires a systemic approach to rapidly diagnose the condition.
-
The first step is the early recognition to prevent the occurrence of exacerbations.
-
The most specific marker associated with increased asthma mortality would be a history of repeated hospital admissions.
Management of Asthma in Children
- Asthma represents the commonest chronic illness of childhood.
- It is also considered a leading cause for childhood morbidity as measured by school absences, ED visits, and hospitalizations.
Asthma Diagnosis in Children
-
Should be based on a careful clinical assessment that includes:
- Recurrent or chronic symptoms related to airway obstruction, such as wheezing, coughing, night symptoms, activity limitation, and shortness of breath.
- The diagnosis can be further supported by the presence of atopy, early sensitization, and a family history of atopy.
-
Whenever possible, spirometry is recommended to be performed to show reversibility of airway obstruction after bronchodilator therapy.
-
In general, spirometry can be performed in children aged ≥5 years.
Asthma in Preschool Children
- Diagnosis and management differs from that of older children and adolescents.
- In addition to the diagnosis of asthma, wheezing in preschool children can be due to unique differential diagnoses e.g.,
- Congenital defects,
- Infections especially viral bronchiolitis,
- Bronchopulmonary dysplasia, and
- Cystic fibrosis.