Complications of Prolonged Labour
Maternal Complications
- Maternal exhaustion and dehydration.
- Rupture of uterus.
- Increased operative intervention.
- Maternal injury.
- Shock.
- Postpartum haemorrhage.
- Puerperal sepsis
- Maternal death
Late Maternal Complications
- Fistula.
- Infertility.;
infection - fibrosis

Fetal Complications
- Birth asphyxia.
- Acidosis.
- Intracranial haemorrhage.
- Meconium aspiration.
- Fetal trauma.
- Death.
- Neonatal infection.
Late Fetal Complications
- Cerebral palsy.
hypoxia
- Mental retardation.

Fetal Compromise in Labour
Presentation
Fetal compromise (hypoxia) may present as:
- Fresh meconium staining to the amniotic fluid a (dark green , containing mucus, bile and epithelial cells) Or
- Abnormal CTG. What are causes of physiological meconium (old meconium)?
- Fetal maturity(post date).
- Breech presentation.
Indications for Continuous EFM
- Significant meconium staining of the amniotic fluid.
- Abnormal FHR detected by intermittent auscultation.
- Maternal pyrexia (temperature →38.0°C).
- Fresh vaginal bleeding.
- Augmentation of contractions with an oxytocin.
- Maternal request.

Risk Factors for Fetal Compromise in Labour
- Placental insufficiency - FGR and pre-eclampsia.
- Prematurity.
- Post maturity.
- Multiple pregnancy.
- Prolonged labour.
- Augmentation with oxytocin/hyperstimulation.
- Precipitate labour.
- Intrapartum abruption.
- Cord prolapse.
- Uterine rupture/dehiscence.
- Maternal diabetes.
- Cholestasis of pregnancy.
- Maternal pyrexia/chorioamnionitis.
- Oligohydramnios.
Management of Possible Fetal Compromise
- Suspicious CTG:
- Repositioning of the mother.
- Intravenous fluids.
- Stopping the oxytocin infusion.
- If a CTG becomes ‘pathological:’ Vaginal examination to exclude : a. Malpresentation b. Cord prolapse c. To assess the progress of the labour.
- If the cervix is fully dilated…instrumental delivery.
- if the cervix is not fully dilated… a Fetal blood sampling with abnormal result… immediate C/S.
Resuscitating in Labour
- Maternal dehydration … intravenous fluids.
- Maternal hypotension … fluid bolus…drugs rarely needed.
- Uterine hyperstimulation …stop oxytocin & tocolytic drugs.
- Venocaval compression …turning the woman into a left lateral position.

High-Risk Obstetrics
Fetal Malpresentation
Occipitoposterior
Options of Delivery
- C-section
- Vaginal delivery (direct OP or rotate into OA)
- Forceps delivery
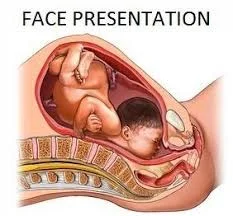
Face Presentation
- Face presentation is due to complete extension of the fetal head.
- Rarely, extension may be due to a Fetal anomaly such as a thyroid tumour.
- The presenting diameter is the submento-bregmatic( measures 9.5 cm )
- Engagement of the Fetal head is late and progress in labour is slow.
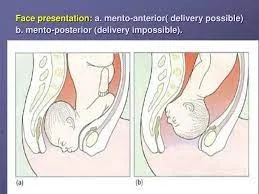
Face presentation: a. mento-anterior( delivery possible) b. mento-posterior (delivery impossible).
FACE PRESENTATION

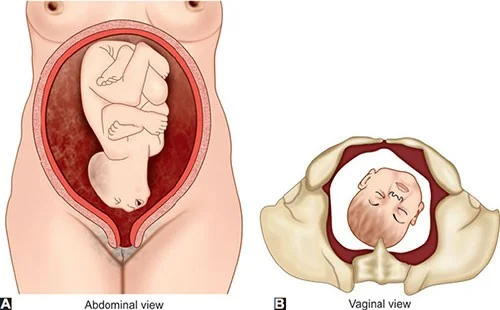
Brow Presentation
Brow presentation arises when there is less extreme extension of the Fetal neck than that with a face presentation. It can be considered a midway position between vertex and face. It is the least common malpresentation.
The causes are similar to those of face presentation.
The presenting diameter is the mento-vertical (measuring 13.5 cm). This is incompatible with a vaginal delivery.
It is diagnosed in labour by palpating the anterior fontanelle, supraorbital ridges and nose on vaginal examination. If this presentation persists, delivery by caesarean section
Breech Presentation
The incidence of breech presentation is 4% of all deliveries.
Before 28 weeks, approximately 25% of fetuses are breech presentation.
By 34 weeks’ gestation, most fetuses have assumed the vertex presentation position.
Classification
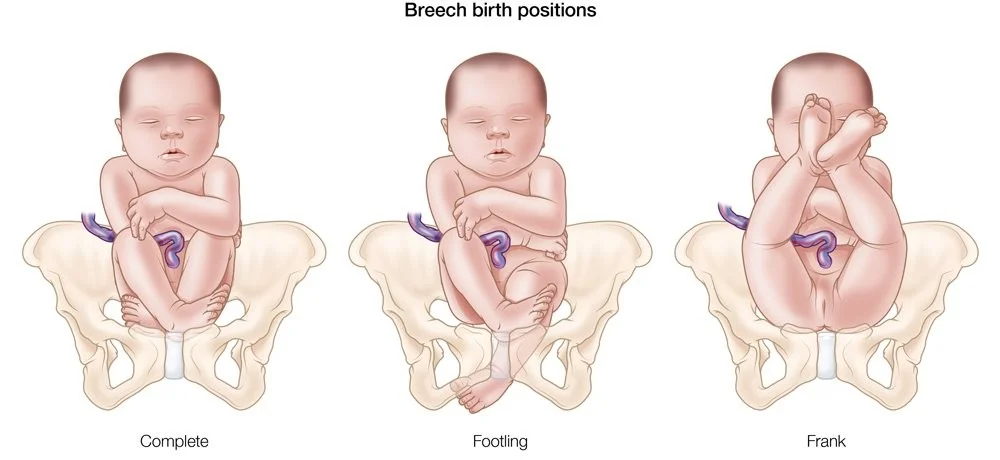
-
Types of breech presentation:
- ✓ Frank
- ✓ Complete.
- ✓ Incomplete or footling.
-
At term
- ✓ 65% of breech fetuses are frank.
- ✓ 25% are complete.
- ✓ 10% are incomplete.
Breech Birth Positions
- Complete
- Footling
- Frank
Etiology
The major factor is prematurity. Approximately 20-30% of all singleton breeches are of low birth weight (<2500 g).
Fetal structural anomalies (e.g., hydrocephalus). In breech presentations, the incidence of structural anomalies is greater than 6%, or two to three times that of a vertex.
Other etiologic factors include uterine anomalies (e.g., bicornuate uterus),
- multiple gestation,
- placenta previa,
- Polyhydramnios,
- contracted maternal pelvis,
- and pelvic tumors that obstruct the birth canal
Vaginal Delivery for Breech Presentation
Until the publication of randomized trials demonstrating that vaginal breech delivery was associated with increased perinatal mortality compared with planned cesarean, vaginal breech deliveries were performed in selected centres in patients who met strict criteria(next slide)
The standard of care now in most practices is to deliver all breeches by cesarean to avoid the potential morbidities of umbilical cord prolapse, head entrapment, birth asphyxia, and birth trauma.
Criteria for Vaginal Delivery of a Breech Presentation
- Fetus must be in a frank or complete breech presentation.
- Gestational age should be at least 36 weeks.
- Estimated fetal weight should be between 2500 and 3800 g.
- Fetal head must be flexed.
- Maternal pelvis must be adequately large, as assessed by x-ray pelvimetry* or tested by prior delivery of a reasonably large baby.
- There must be no other maternal or fetal indication for cesarean delivery.
- Anesthesiologist must be in attendance.
Factors Favouring Cesarean Delivery of the Breech Fetus
- Lack of operator experience
- Patient request for cesarean delivery
- Large fetus: > 3800 to 4000 g
- Preterm fetus either with active labor or with indicated delivery
- Severe fetal-growth restriction
- Fetal anomaly incompatible with vaginal delivery
- Prior perinatal death or neonatal birth trauma
- Incomplete or footling breech presentation
- Hyperextended head
- Pelvic contraction or unfavourable pelvic.
- Prior cesarean delivery
Complications of a Breech
- Increased risk of cord prolapse: particularly with footling breech.
- Increased risk of CTG abnormalities as cord compression is common.
- Mechanical difficulties with the delivery of the shoulders and/or after-coming head, leading to damage of the visceral organs or the brachial plexus.
- Delay in the delivery of the head lead to hypoxia.
- Uncontrolled rapid delivery of the head may occur with a smaller fetus and predisposes to tentorial tears and intracranial bleeding.
- A small or preterm fetus may deliver through an incompletely dilated cervix, resulting in head entrapment.