IM
H M ABDELRAHIM
Cushing’s Syndrome
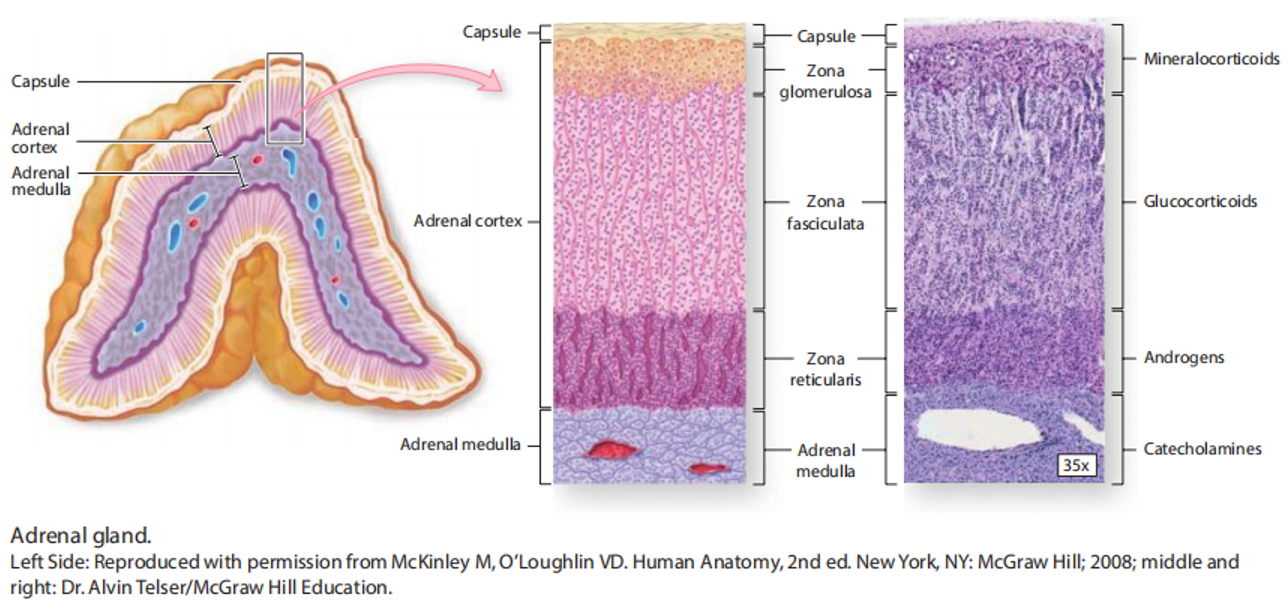
Adrenal Gland
The adrenal cortex secretes three main categories of steroids: * Mineralocorticoids (Salt): Primarily Aldosterone, regulated by the renin-angiotensin-aldosterone system. * Glucocorticoids (Sugar): Primarily Cortisol, regulated by the hypothalamic-pituitary-adrenal (HPA) axis. * Androgens (Sex Hormones): Contribute to the development of secondary sexual characteristics.
The adrenal cortex is divided into three zones:
-
Zona Glomerulosa (G): Outermost layer, produces Aldosterone.
-
Zona Fasciculata (F): Middle layer, produces Cortisol.
-
Zona Reticularis (R): Innermost layer, produces Androgens.
The adrenal medulla secretes catecholamines (epinephrine and norepinephrine), which are involved in the “fight-or-flight” response.
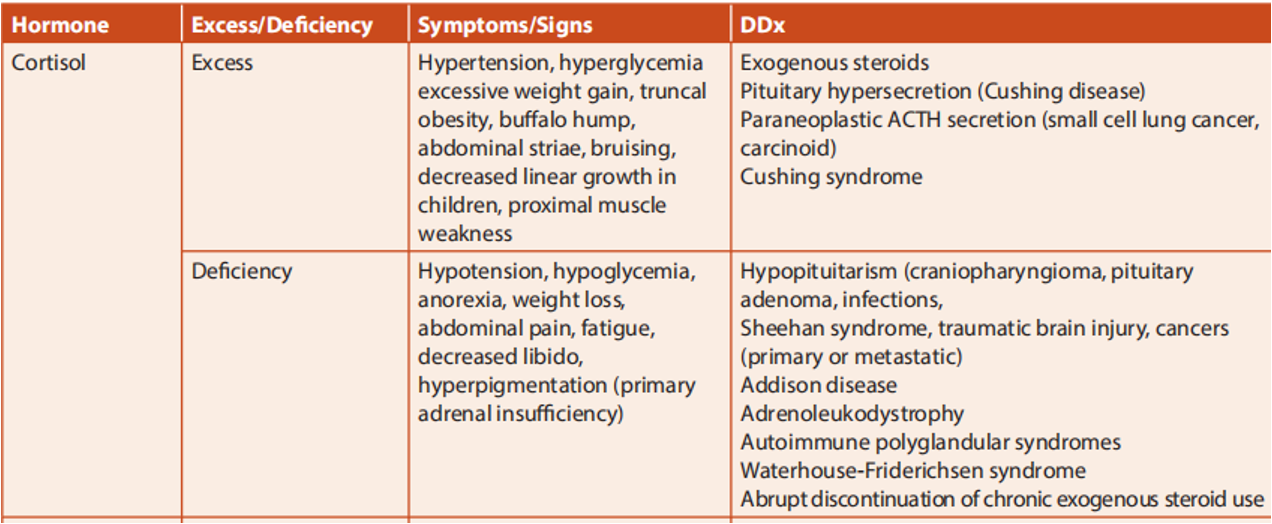
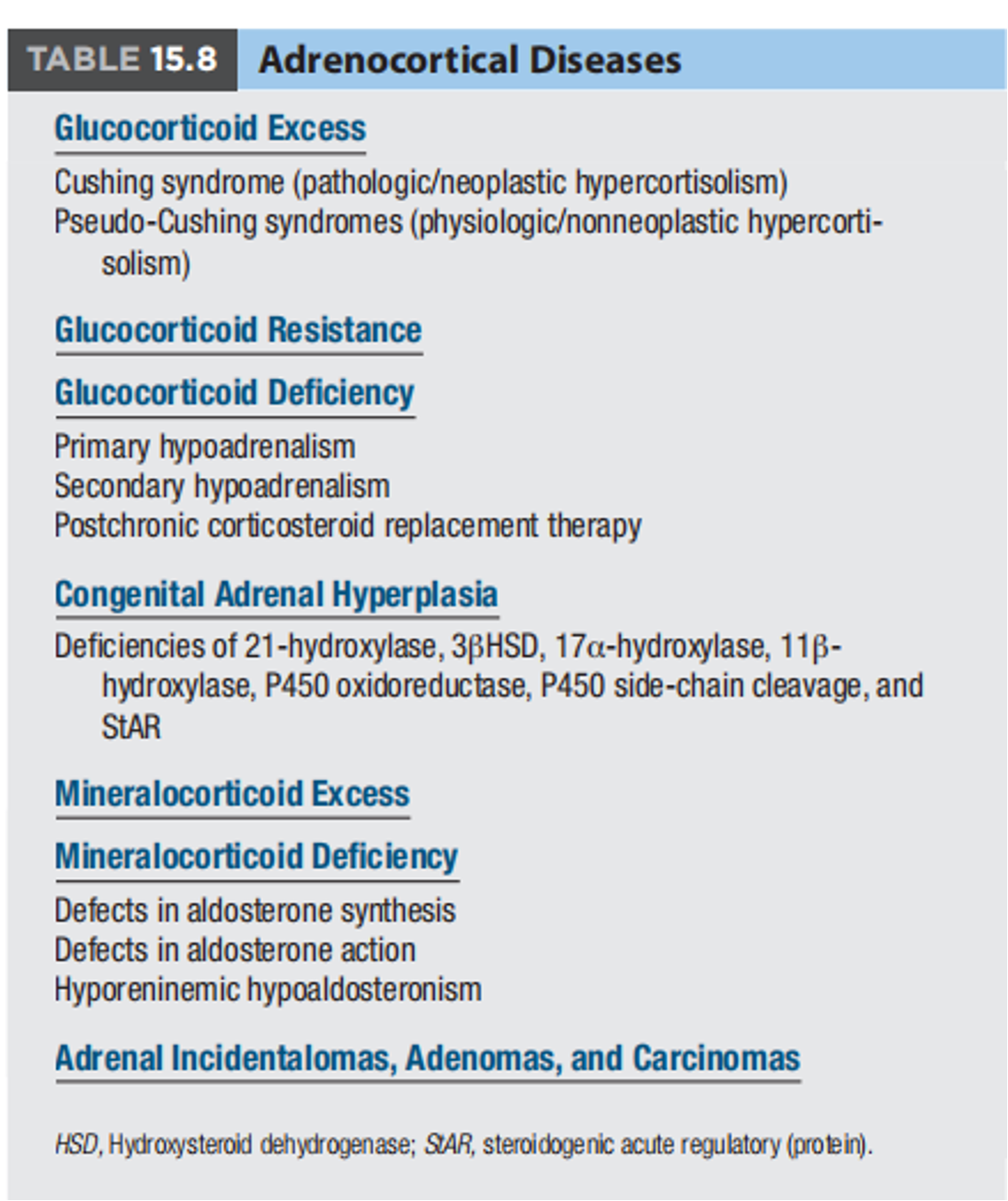
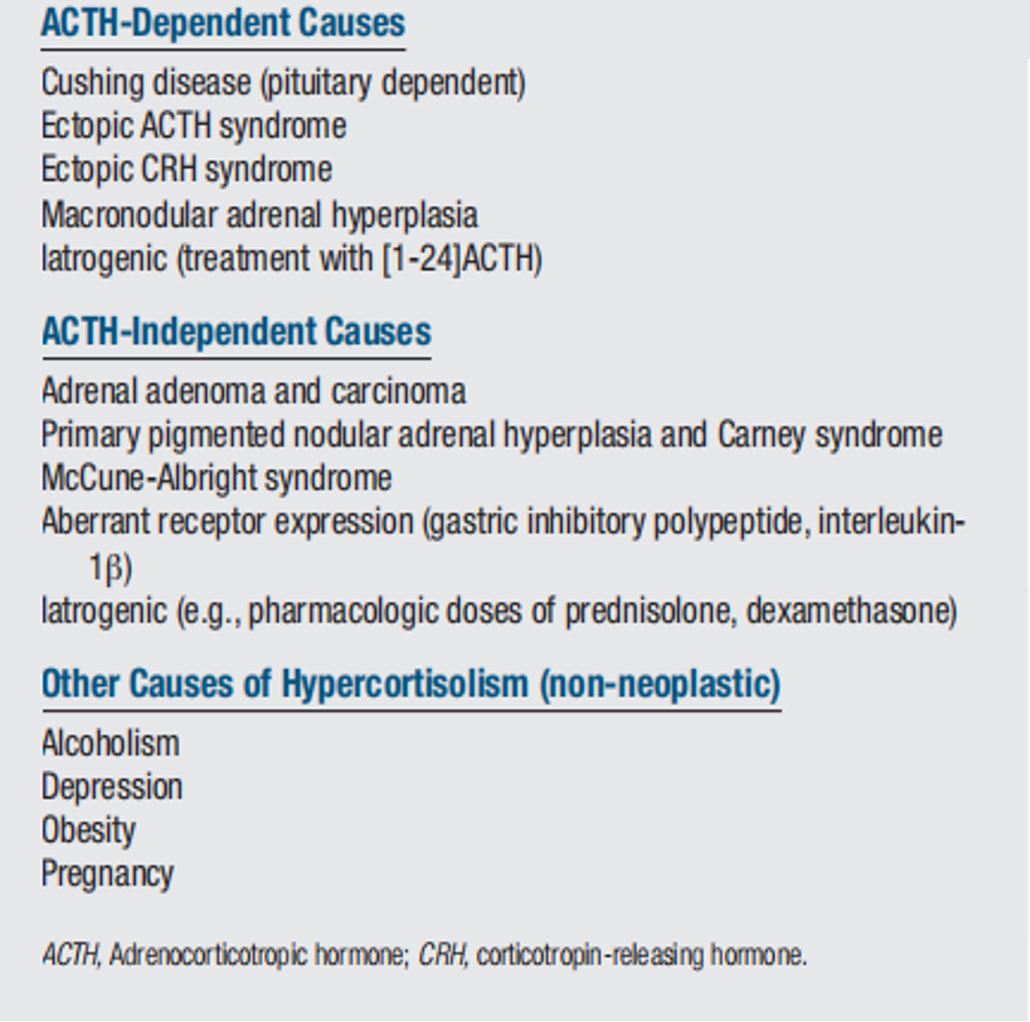
Hypercortisolism
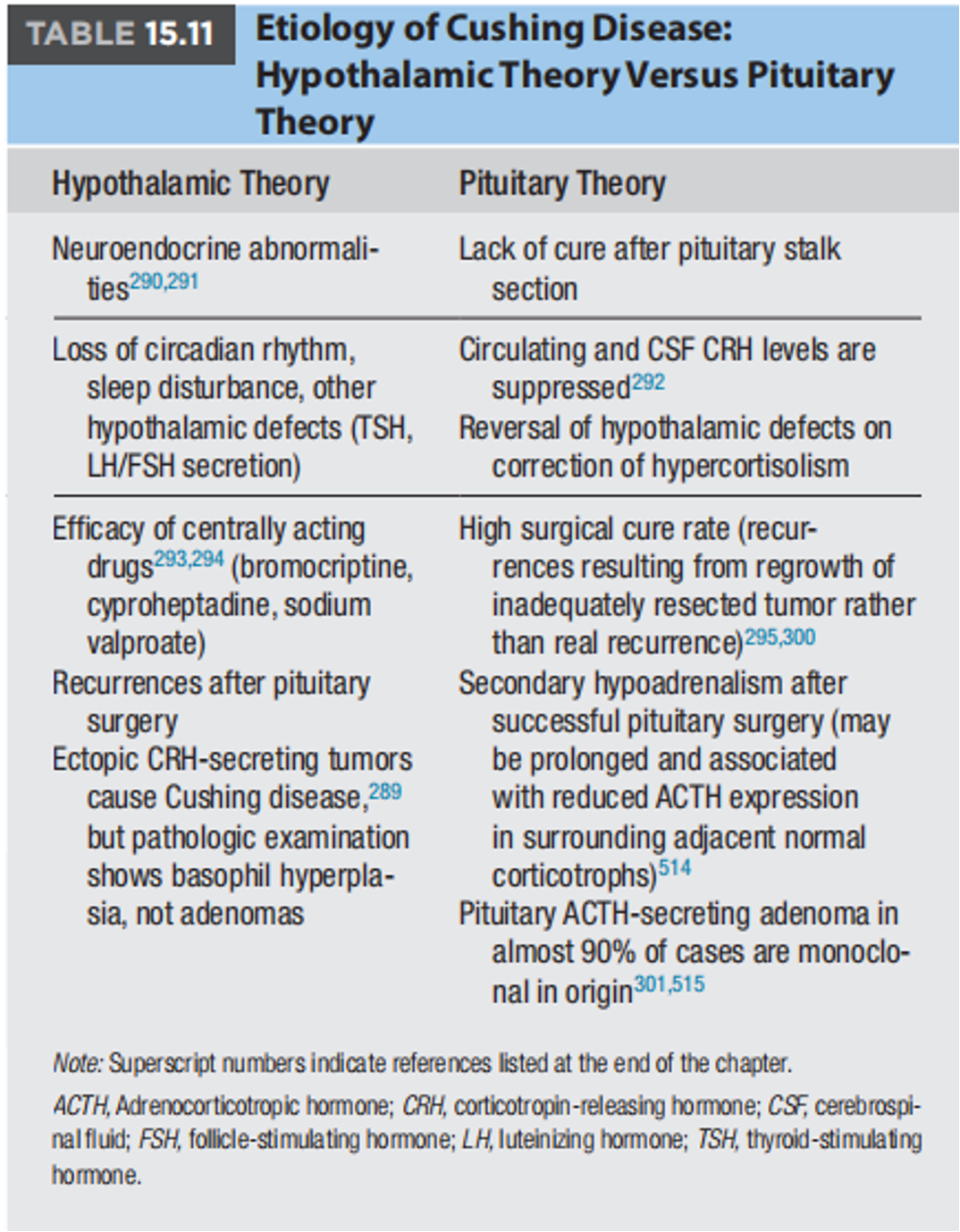
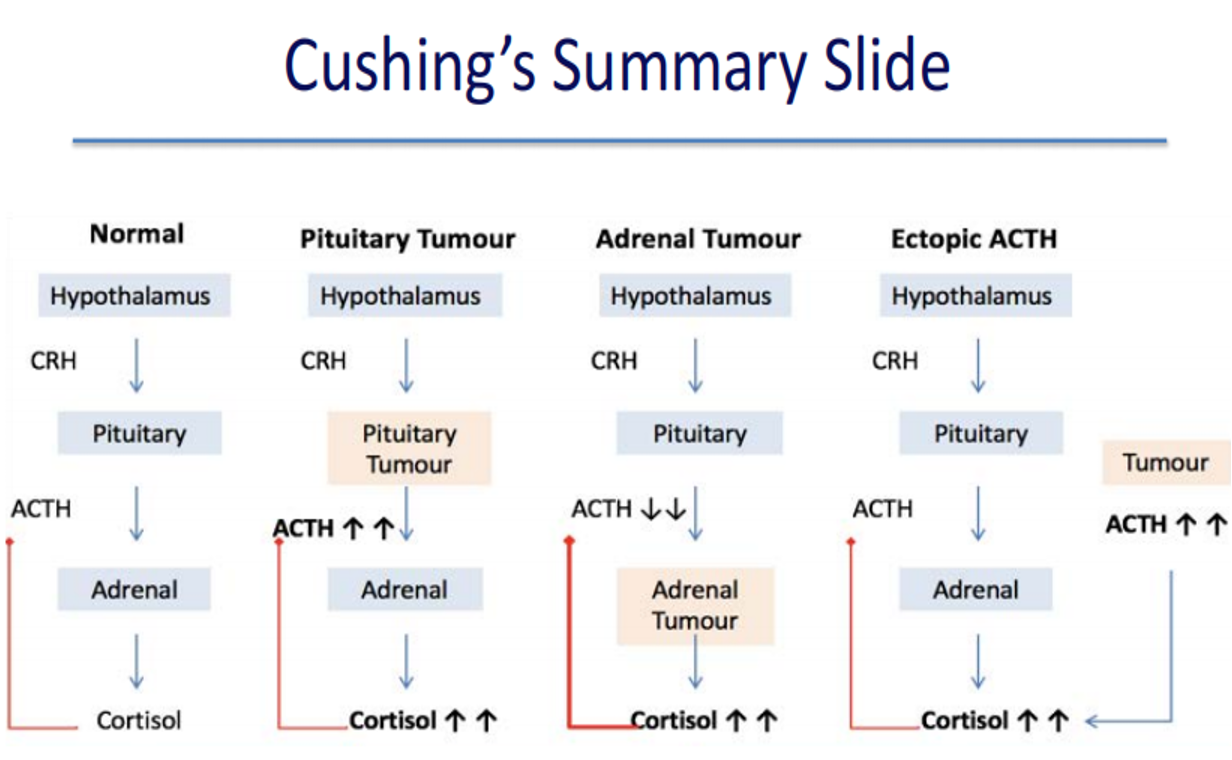
Cushing’s Disease: Hypercortisolism specifically caused by an ACTH-producing pituitary adenoma.
Cushing’s Syndrome: A broader term encompassing hypercortisolism from any cause, including:
- Pituitary adenoma (Cushing’s Disease)
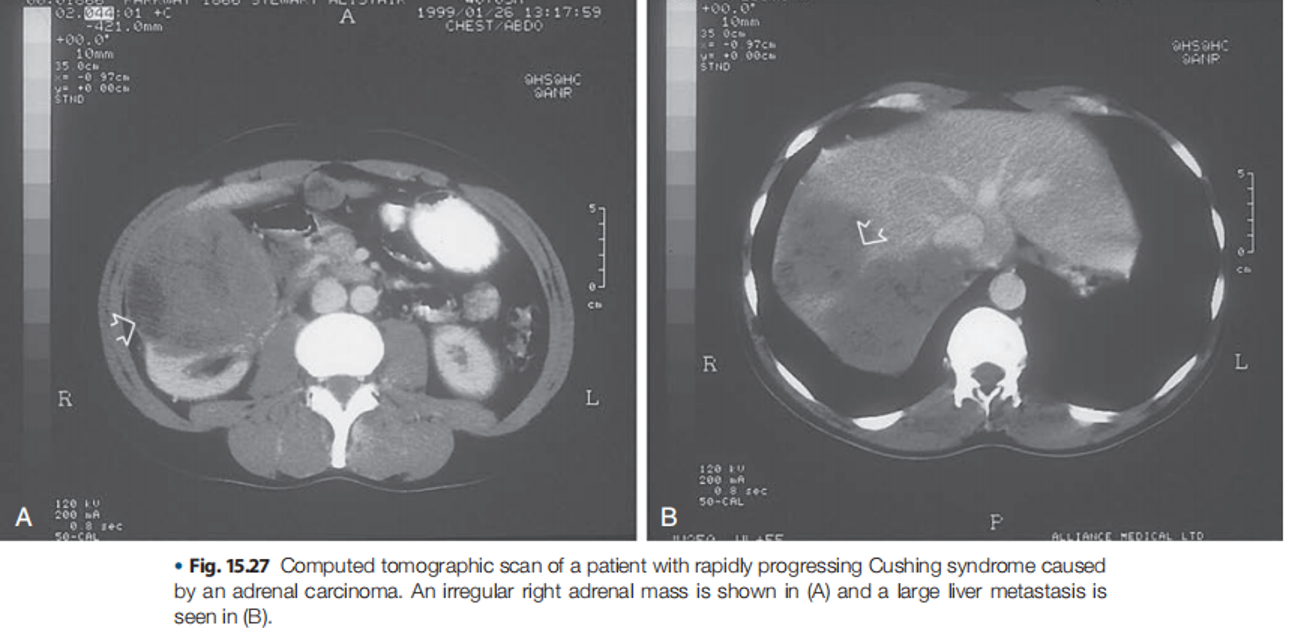
- Adrenal adenoma or carcinoma
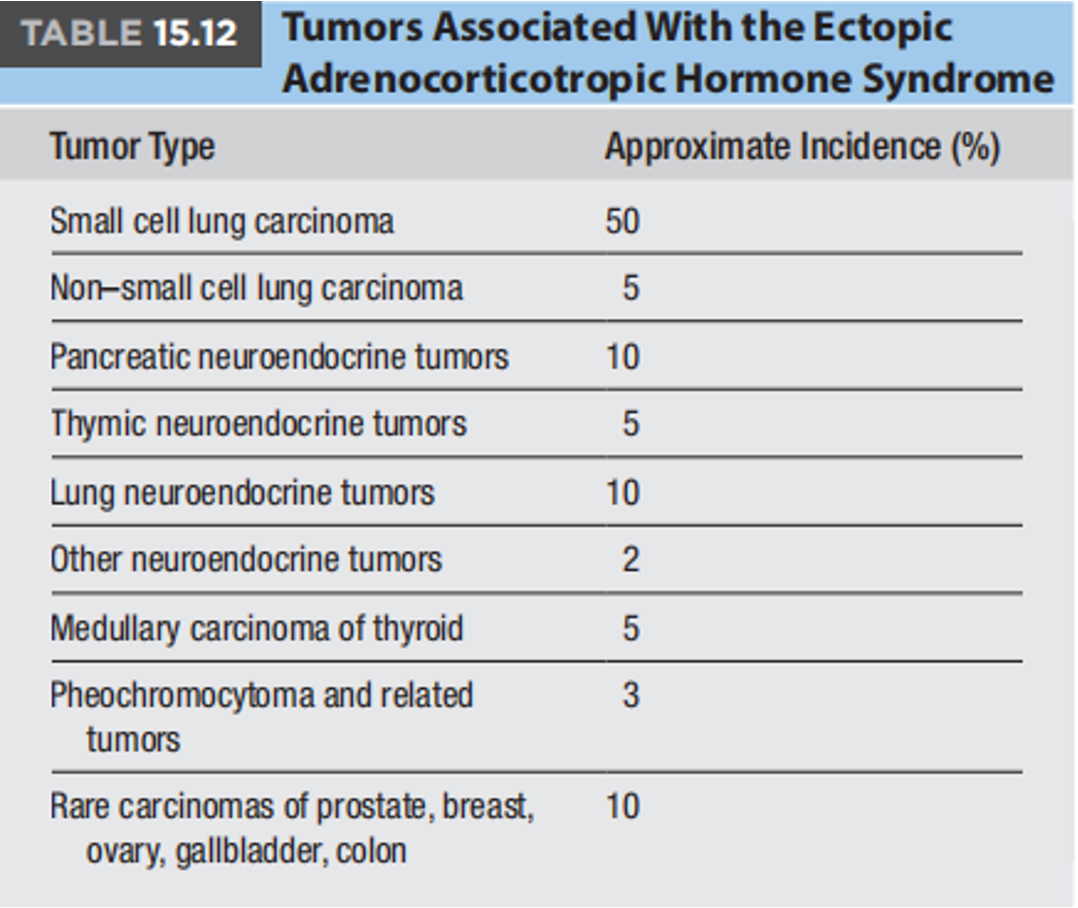
- Ectopic ACTH production (e.g., from a lung tumor)
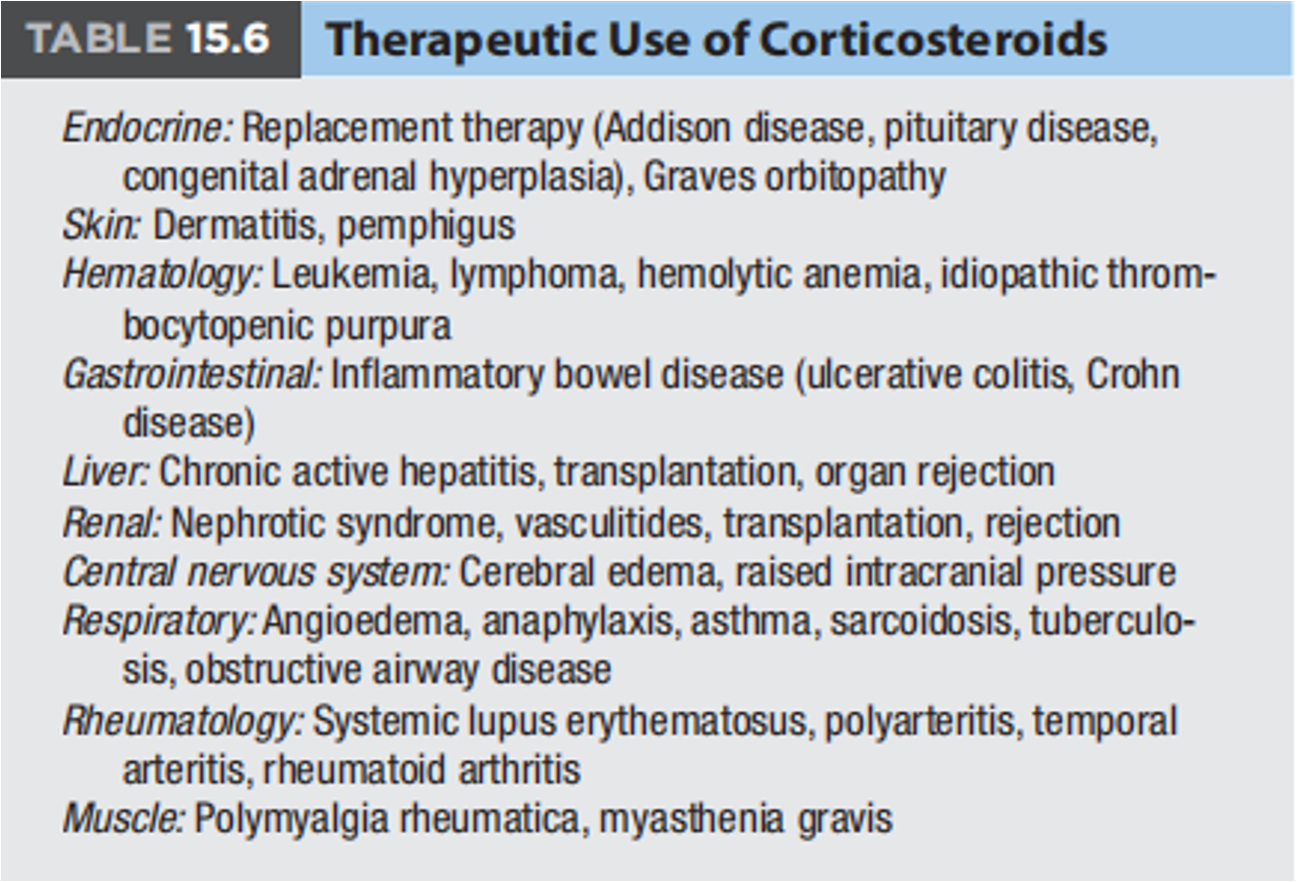
- Administration of exogenous glucocorticoids (e.g., prednisone)
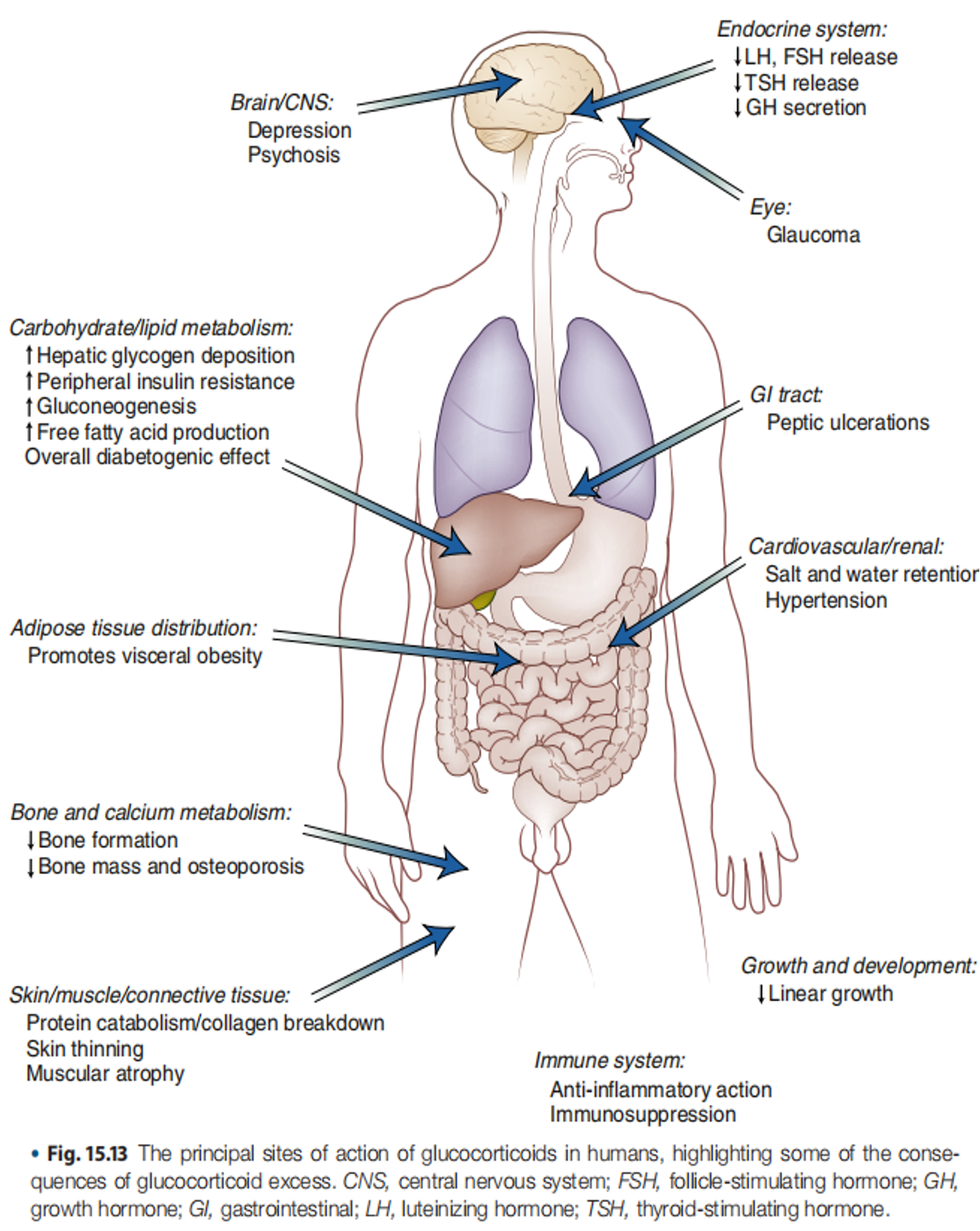
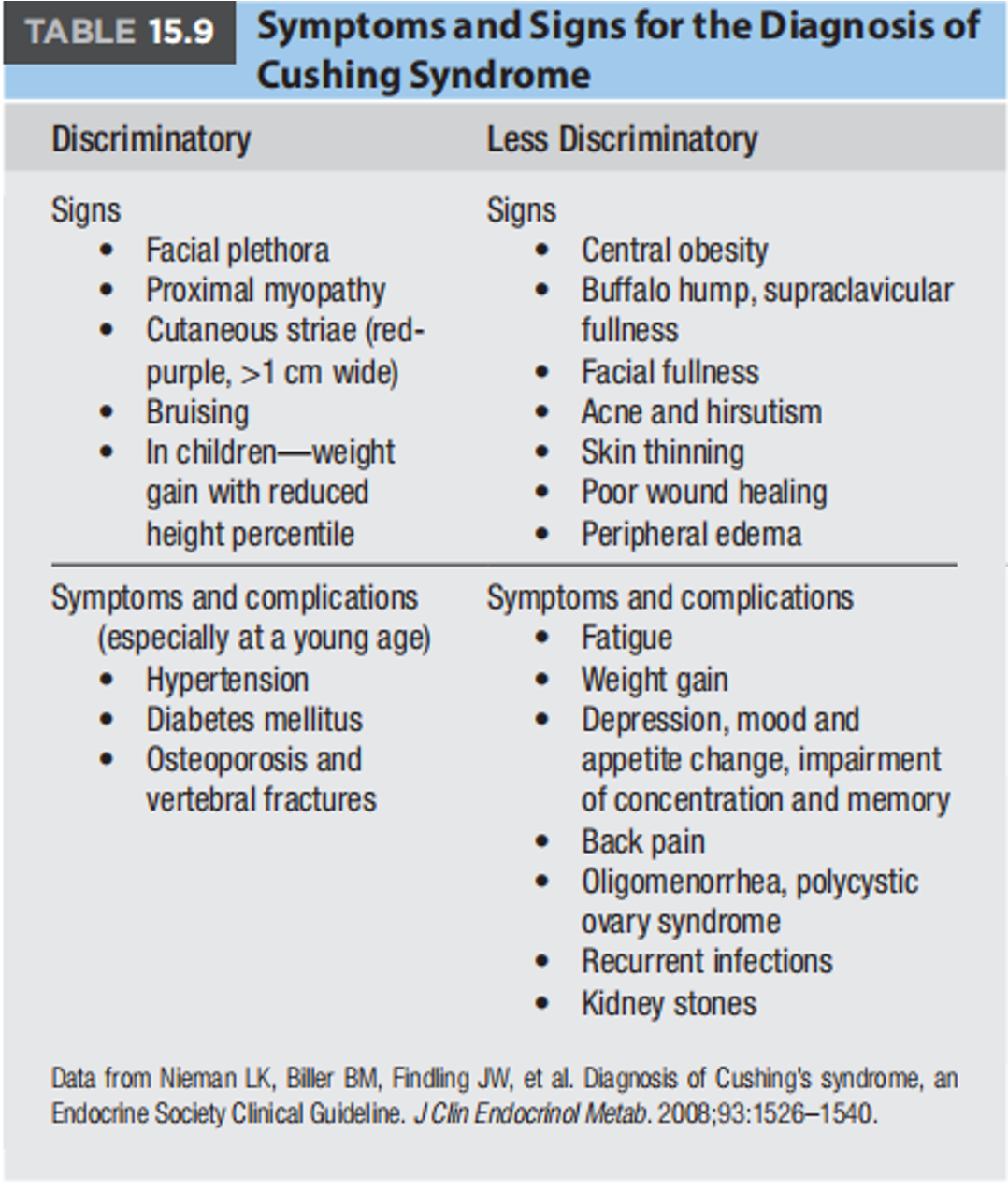
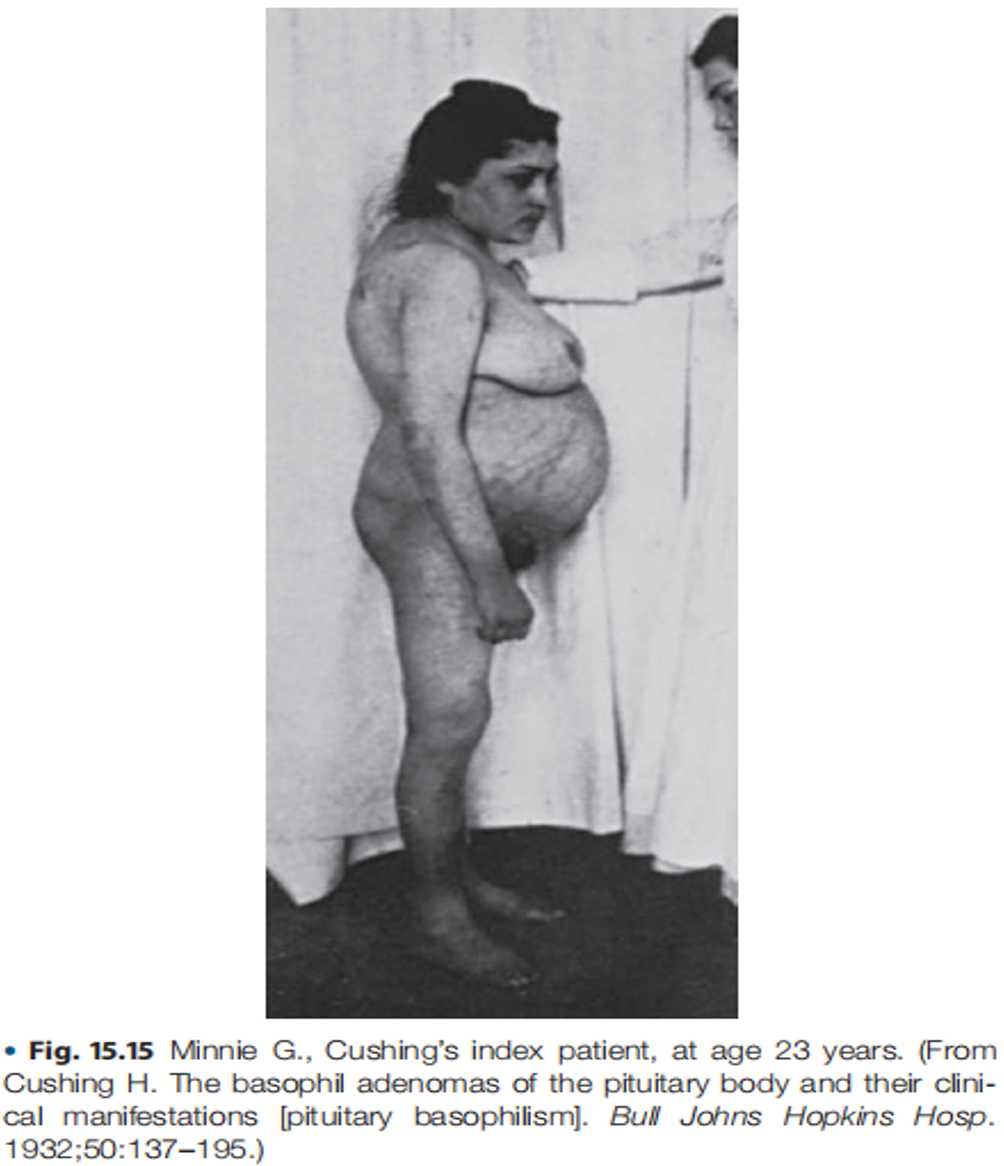
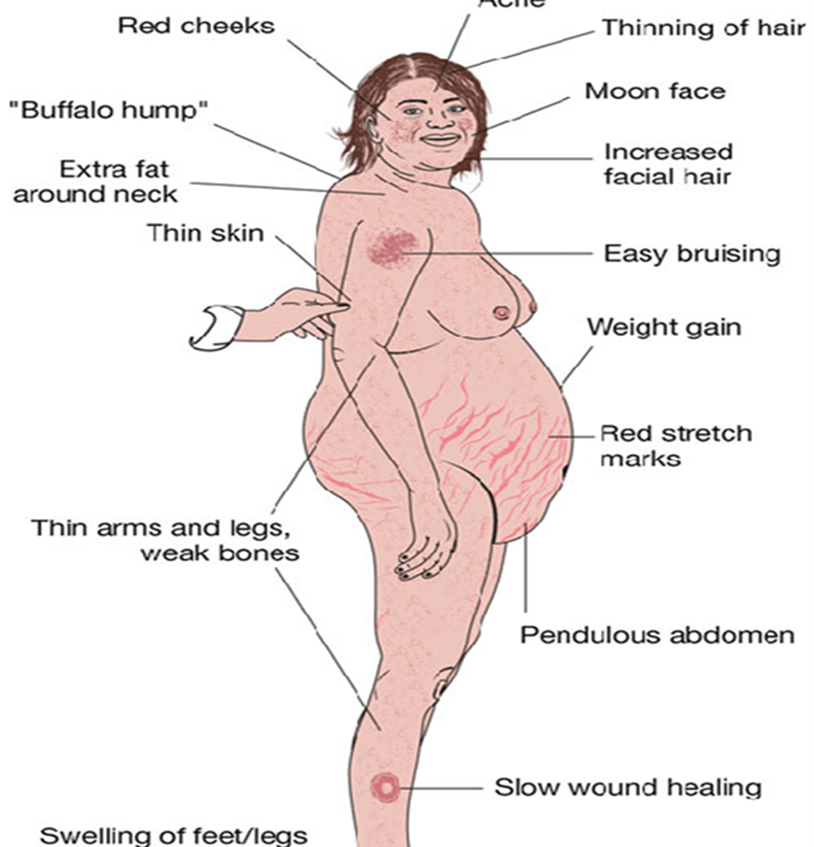
Clinical Presentation
-
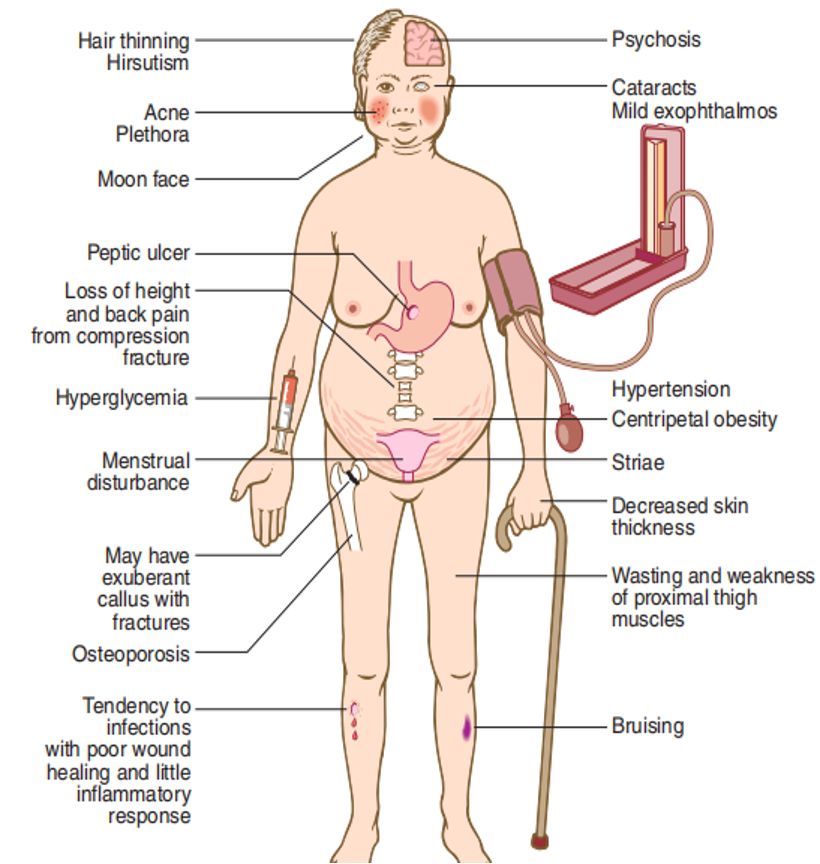
Hypertension: High blood pressure.
-
Central Obesity: Accumulation of fat around the abdomen and trunk.
-
Moon Facies: Round, full face.
-
Dorsal Fat Pad (Buffalo Hump): Fat accumulation between the shoulders.
-
Purple Striae: Stretch marks on the skin, often purplish or reddish.
-
Muscle Weakness: Proximal myopathy; muscle weakness, making it difficult to climb stairs or rise from a chair.
-
Other Symptoms:
- Psychiatric symptoms (e.g., depression, anxiety)
- Secondary amenorrhea (absence of menstrual periods) in women
- Hirsutism (excess hair growth) or other signs of masculinization in women
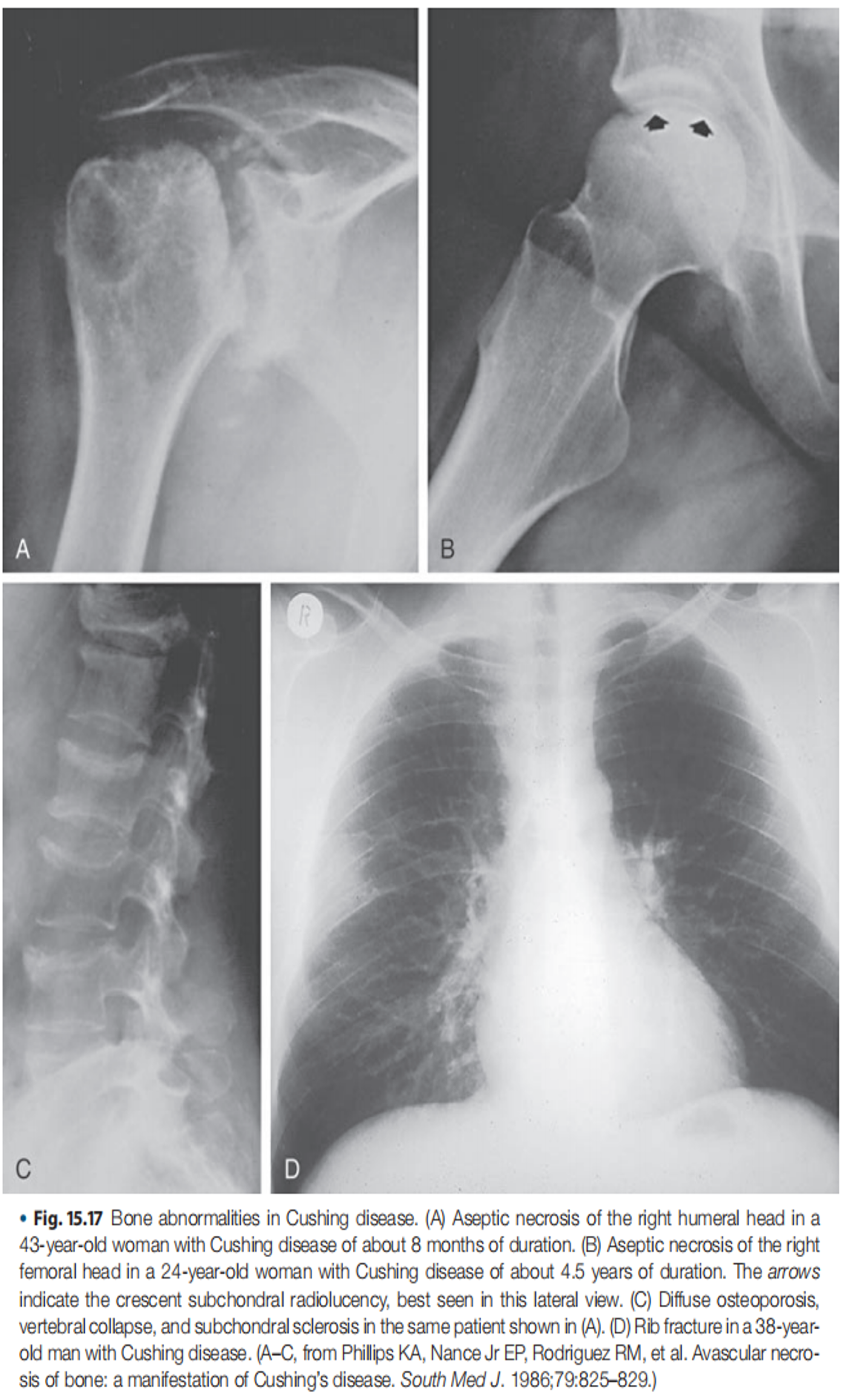
- Osteoporosis (weakened bones) in both men and women
- Glucose intolerance or diabetes
- Metabolic alkalosis with hypokalemia (in severe cases)

Diagnosis
-
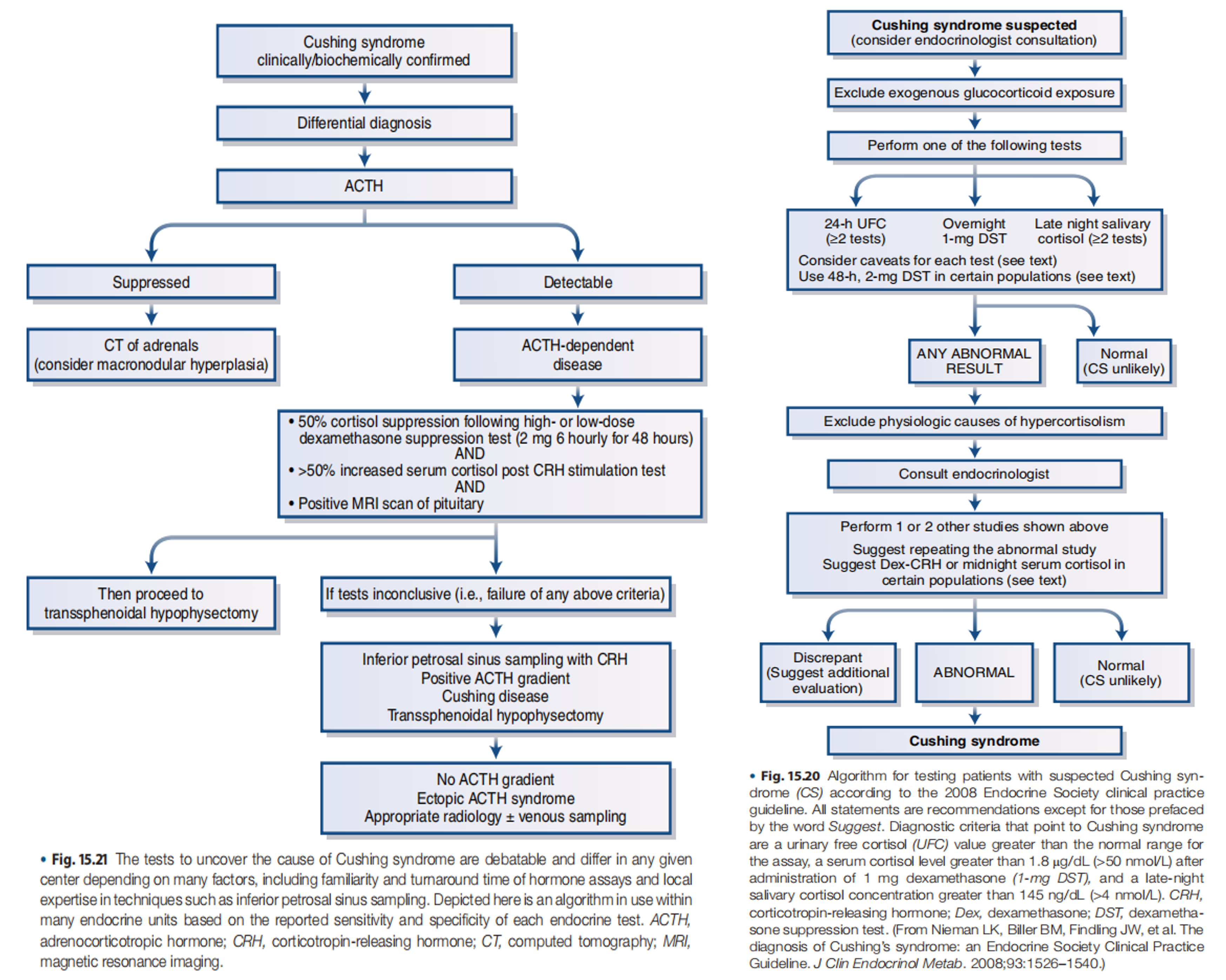
Initial Screening:
- 24-hour Urine Free Cortisol (UFC): Measures the amount of cortisol excreted in the urine over a 24-hour period.
- Bedtime Salivary Cortisol: Measures cortisol levels in saliva collected at bedtime.
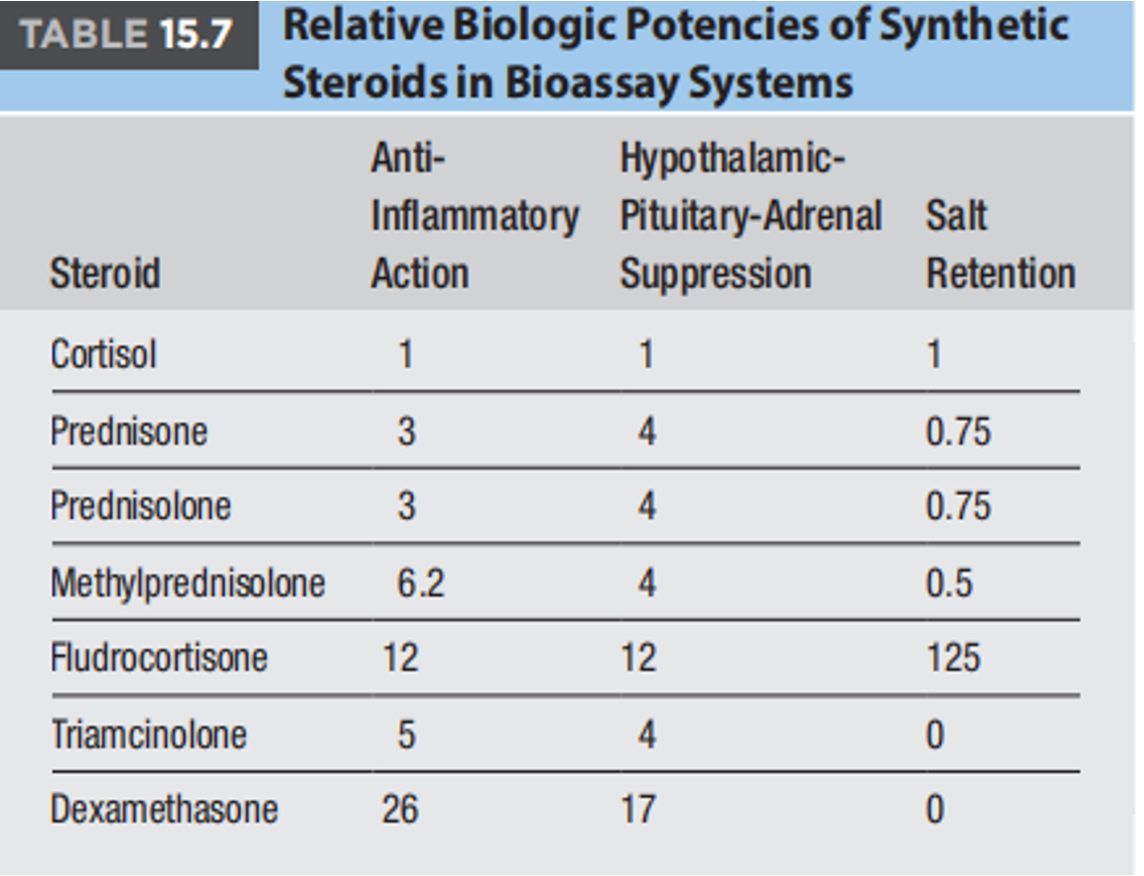
- 1-mg Overnight Dexamethasone Suppression Test: A low dose of dexamethasone is given at night, and cortisol levels are measured in the morning. Suppression of cortisol indicates a normal response.
-
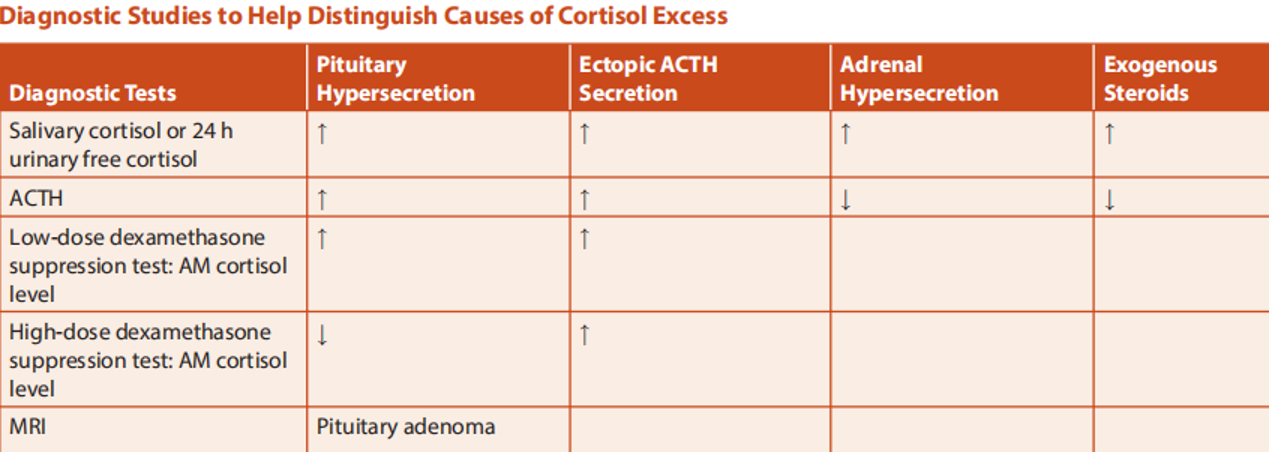
Differentiating the Cause:
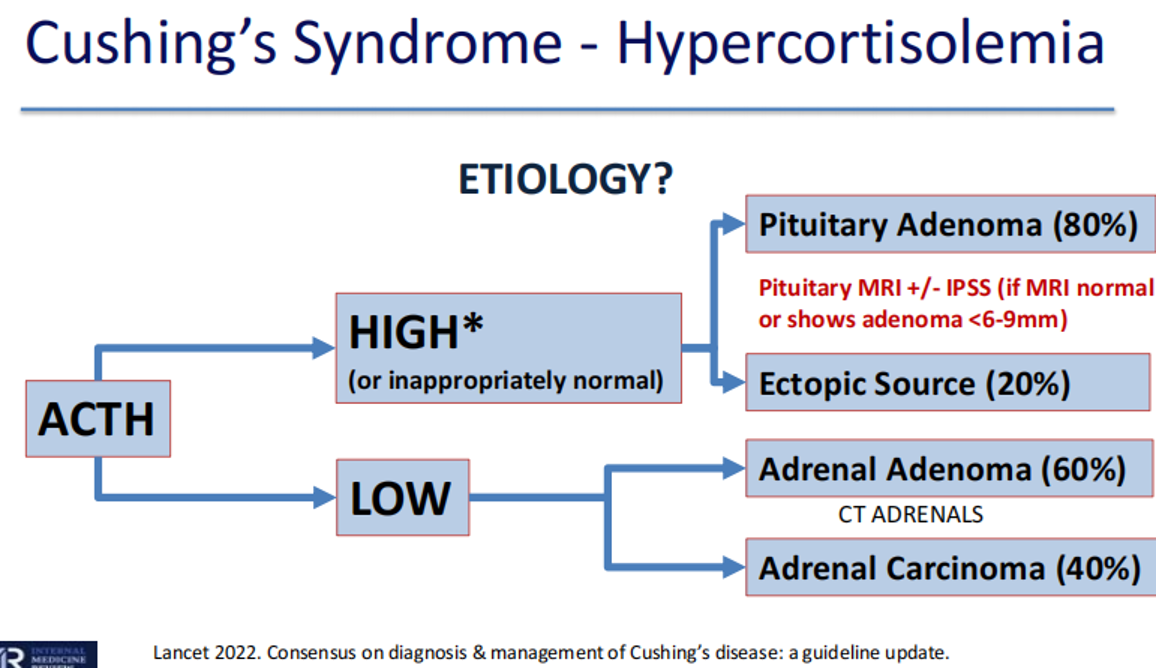
- Plasma ACTH Levels:
- High or Normal ACTH: Suggests ACTH-dependent Cushing’s Syndrome (e.g., pituitary adenoma, ectopic ACTH production).
- Low ACTH (less than 10 pg/mL): Suggests ACTH-independent Cushing’s Syndrome (e.g., adrenal adenoma).
- Plasma ACTH Levels:
-
Further Investigations:
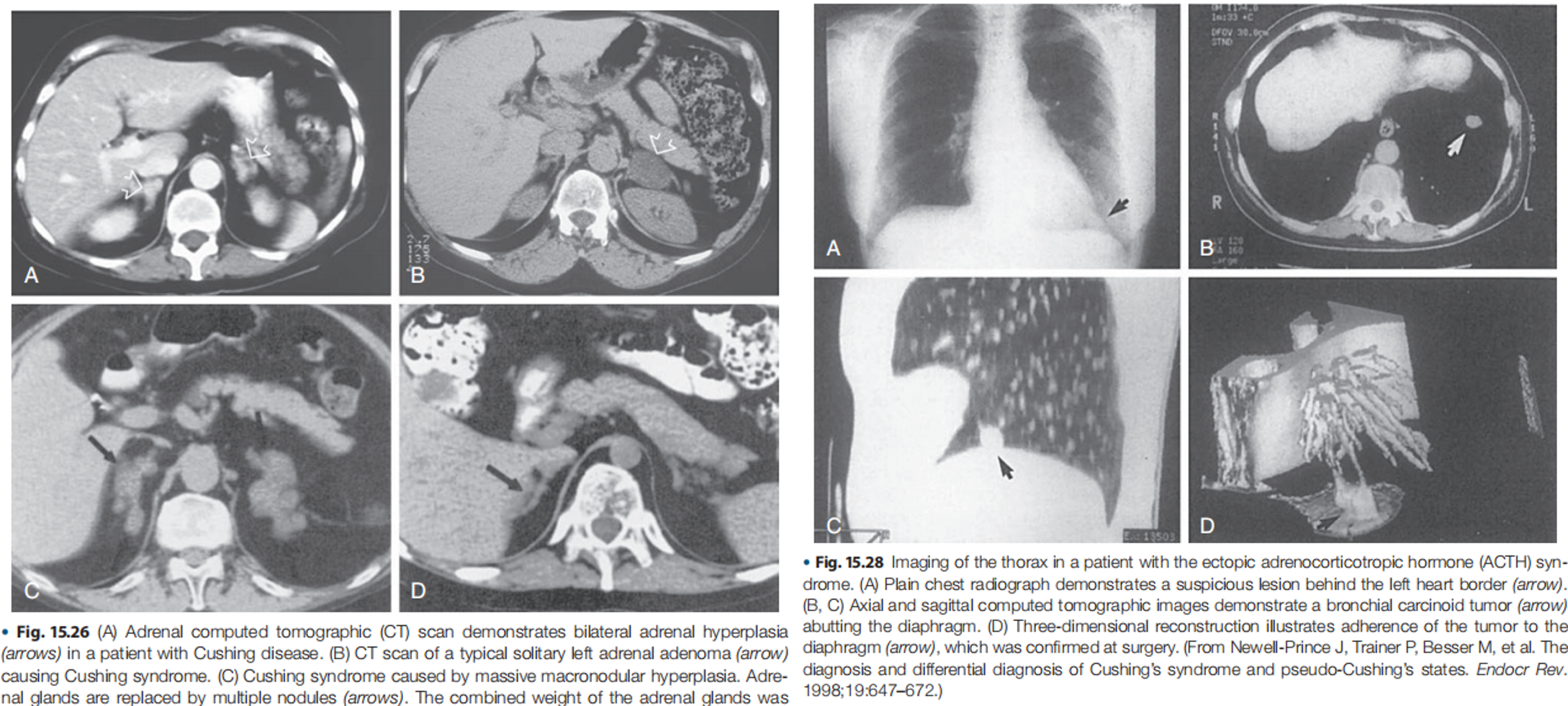
- ACTH-Independent: Adrenal imaging (CT or MRI) is necessary to locate the source of excess cortisol production.
- ACTH-Dependent: Further testing is required to differentiate between pituitary and ectopic ACTH production:
- High-Dose Dexamethasone Suppression Test (8mg): Less commonly used now due to poor test characteristics.
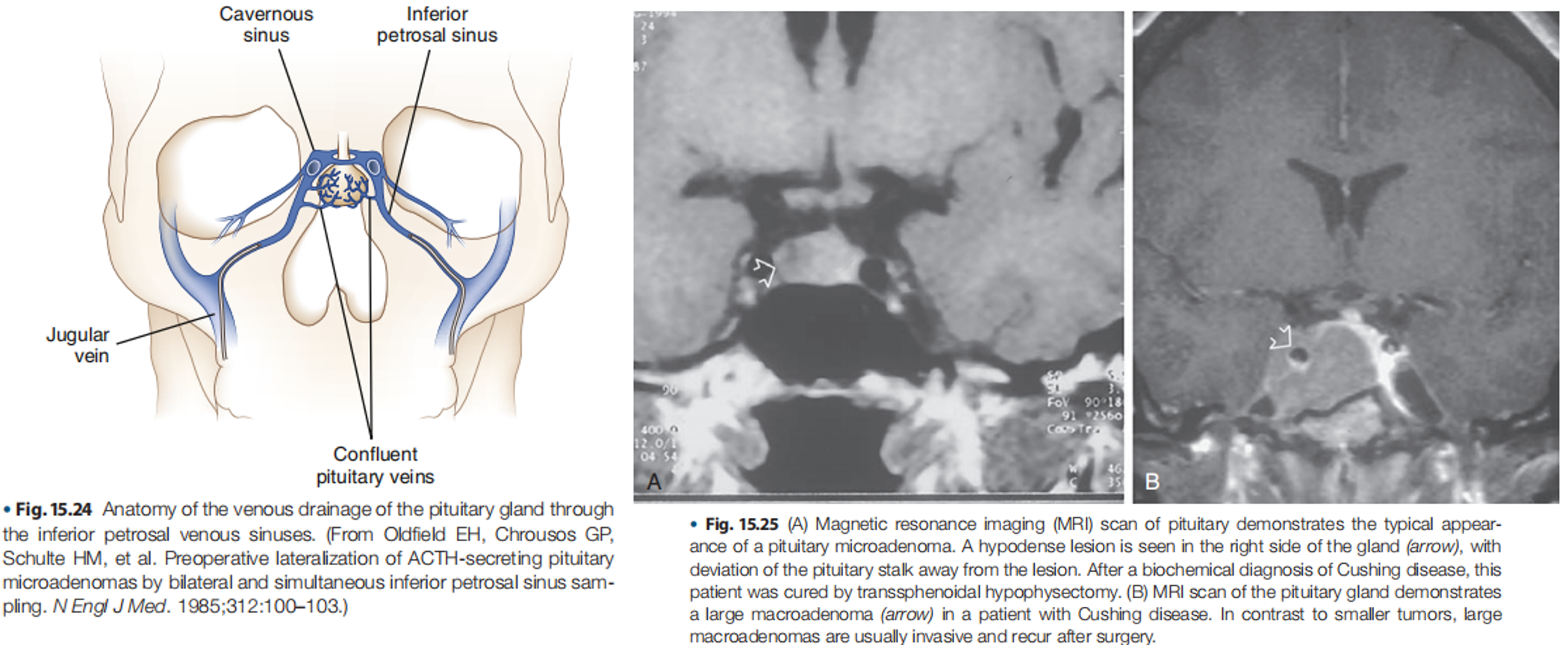
- Inferior Petrosal Sinus Sampling (IPSS): The gold standard for differentiating pituitary from ectopic ACTH secretion.
- MRI of the Pituitary: To visualize the pituitary gland and identify potential adenomas.
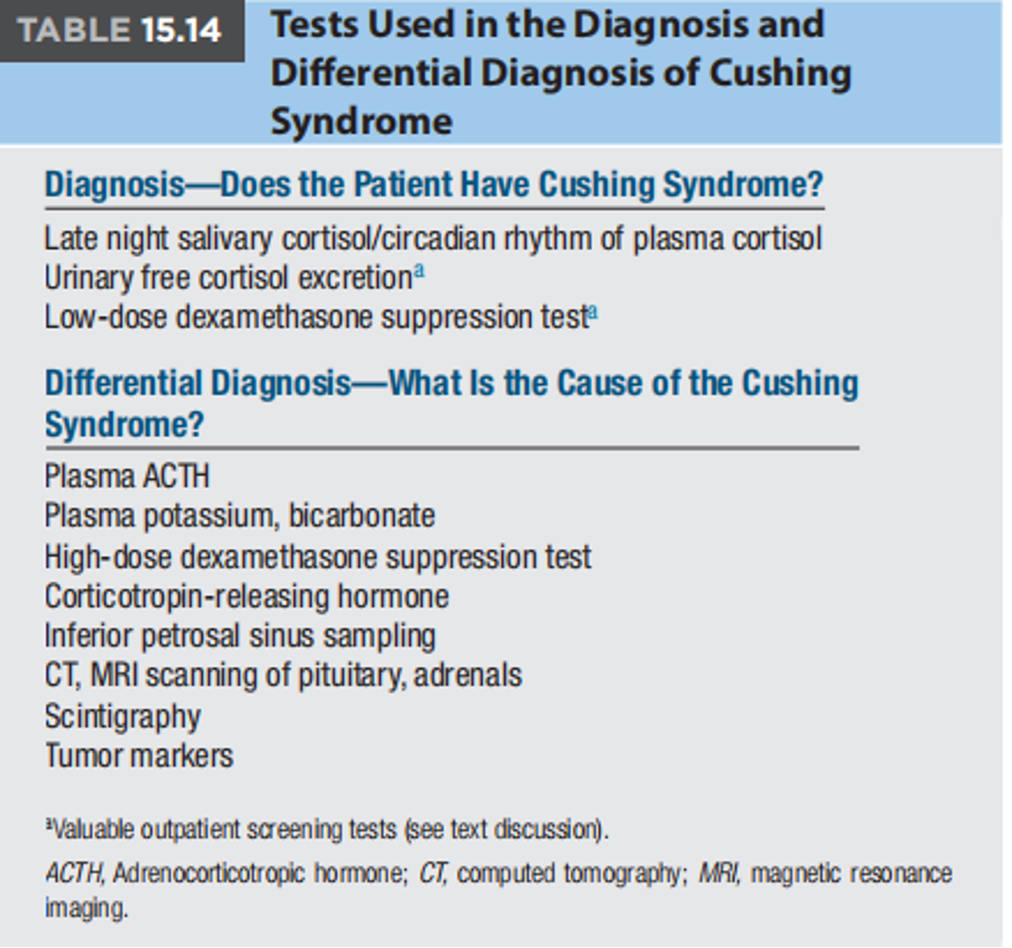
Inferior Petrosal Sinus Sampling (IPSS)
- Gold Standard: For differentiating pituitary (Cushing’s Disease) from ectopic ACTH secretion.
- Procedure: Catheters are placed in the inferior petrosal sinuses (which drain the pituitary gland) and a peripheral vein. ACTH levels are measured in both locations after administering corticotropin-releasing factor (CRF).
- Interpretation: A central-to-peripheral ACTH ratio helps determine the source of ACTH.
- Invasive: Only performed at specialized centers.
Screening Tests for Hypercortisolism
- Confirmation of Cushing’s Syndrome requires 2 out of 3 positive screening tests:
- 1-mg Dexamethasone Suppression Test: Cortisol >140 nmol/L after dexamethasone administration is considered positive.
- 24-hour Urine Free Cortisol (UFC): Abnormal on two separate collections.
- Late-Night Salivary Cortisol: Abnormal on two separate collections.
Cushing’s Syndrome – Don’t pick 8mg Dex! *A note on the high dose (8mg Dex) suppression test: Classic teaching *
High-Dose Dexamethasone Suppression Test (8mg) - Important Note
-
Outdated: While historically used, the 8mg dexamethasone suppression test is no longer recommended due to its poor sensitivity and specificity.
-
Current Practice: MRI of the pituitary and/or IPSS are preferred for differentiating pituitary from ectopic ACTH secretion.
- If 8mg Dexametazone HS suppresses am cortisol =
Cushing’s disease due to pituitary cause ⇒ Order MRI Sella - If 8mg Dex does not suppress cortisol ⇒ Ectopic ACTH (e.g. neuroendocrine carcinoma) ⇒ CT the chest for malignancy
- If 8mg Dexametazone HS suppresses am cortisol =
Poor test characteristics, thus 8mg Dex no longer recommended by newer guidelines; MRI +/- IPSS is used instead
Treatment
- Pituitary Source (Cushing’s Disease): Transsphenoidal surgery to remove the pituitary adenoma.
- Adrenal Source: Laparoscopic Adrenalectomy (surgical removal of the affected adrenal gland). best treatment
When Surgical Cure is Not Possible (or in the interim):
-
Medical Therapy: Medications can be used to:
- Inhibit ACTH secretion (e.g., pasireotide)
- Inhibit cortisol secretion by the adrenal glands (e.g., ketoconazole, metyrapone, mitotane)
- Block cortisol effects (e.g., mifepristone)
-
Other Options:
- Pituitary radiation
- Bilateral adrenalectomy (in severe cases)
Summary
- Cushing’s Syndrome is a serious condition caused by prolonged exposure to high levels of cortisol.
- Early diagnosis and treatment are essential to prevent complications.
- Treatment options depend on the underlying cause of the hypercortisolism.
Surgery
Cushing’s syndrome
Secretion of cortisol from adrenal cortex
- 4 times more frequent in females
- Usually occurs at 35-50 years of age
Causes:
- Endogenous
- Adrenal tumor
- Tumor of the anterior pituitary gland (Cushing’s disease)
- Hyperplasia (NAH)
- Ectopic ACTH
- Secreting tumor (e.g., lung, pancreas)
- Exogenous
- Excessive cortisone intake
DIAGNOSIS:
- High Serum cortisol levels
- URINARY LEVELS OF STEROID METABOLITES
- 17-OHCS (hydroxycorticosteroid) (High)
- 17-KS (ketosteroid) (High)
Hematology:
- WBCs (Decreased)
- Lymphocytes (Increased)
- Eosinophils (Decreased
TREATMENT:
- Primary:
- Adrenalectomy (unilateral or bilateral)
- if bilateral, need hormone replacement for life
- Secondary
- Trans-sphenoidal removal of pituitary tumor
- Ectopic:
- Try to remove the source of ACTH secretion
- Radiation to tumors
- Palliative drugs:
- MITOTANE (destroys tissue in the adrenal cortex)
Clinical Medicine
- Mental retardation; Stunted growth
- Moon Face
- Inter scapular pad of fat
- Stretch marks
- Thin extremities, central Obesity
- Risk of infections