Dr. Nada Abdelrahman
vWD
Overview
- Most common hereditary coagulopathy: Prevalence of 1-2% in the general population.
- Can be congenital or acquired.
- Characterized by mucocutaneous bleeding (e.g., epistaxis, menorrhagia). Hemarthroses and muscle hematomas are rare.
Pathophysiology
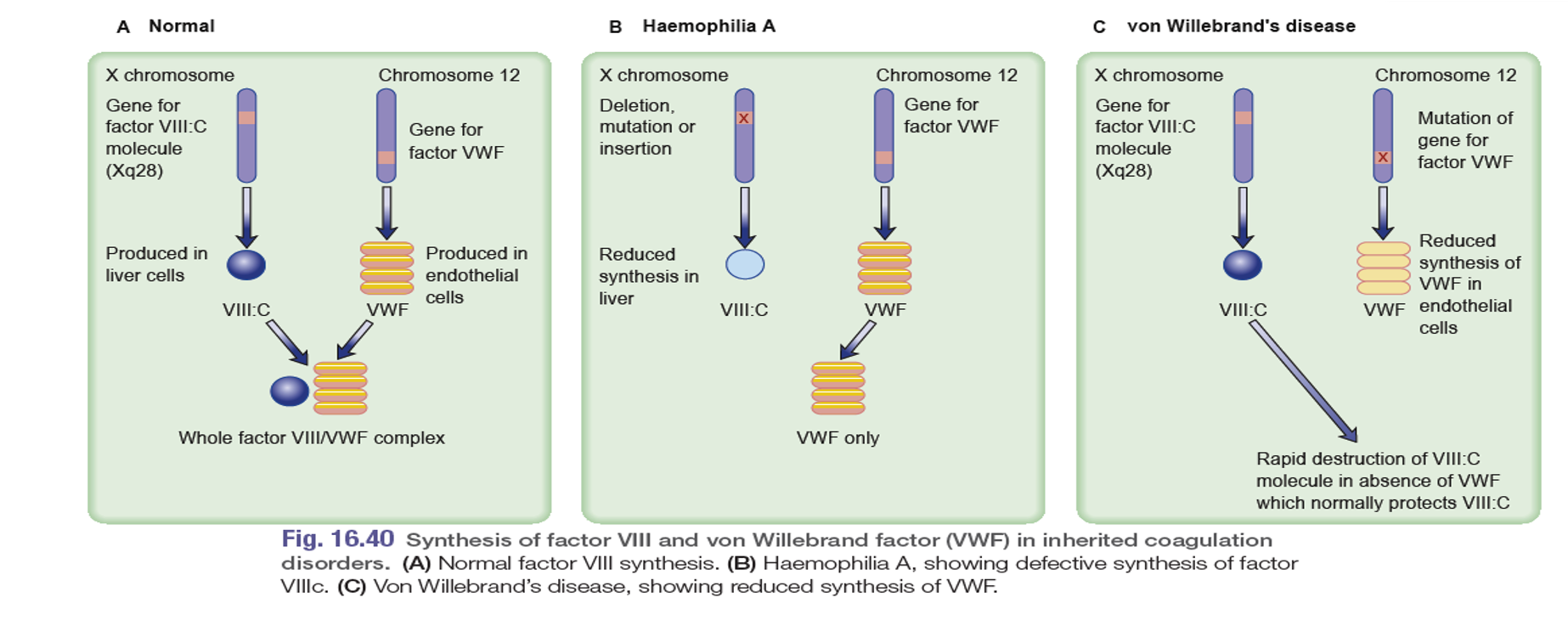
- Deficiency or dysfunction of von Willebrand factor (vWF), a multimeric glycoprotein encoded on chromosome 12.
- vWF has two main functions:
- Assists in platelet plug formation by attracting platelets to the site of damage.
- Binds to factor VIII, preventing its degradation and maintaining normal levels.
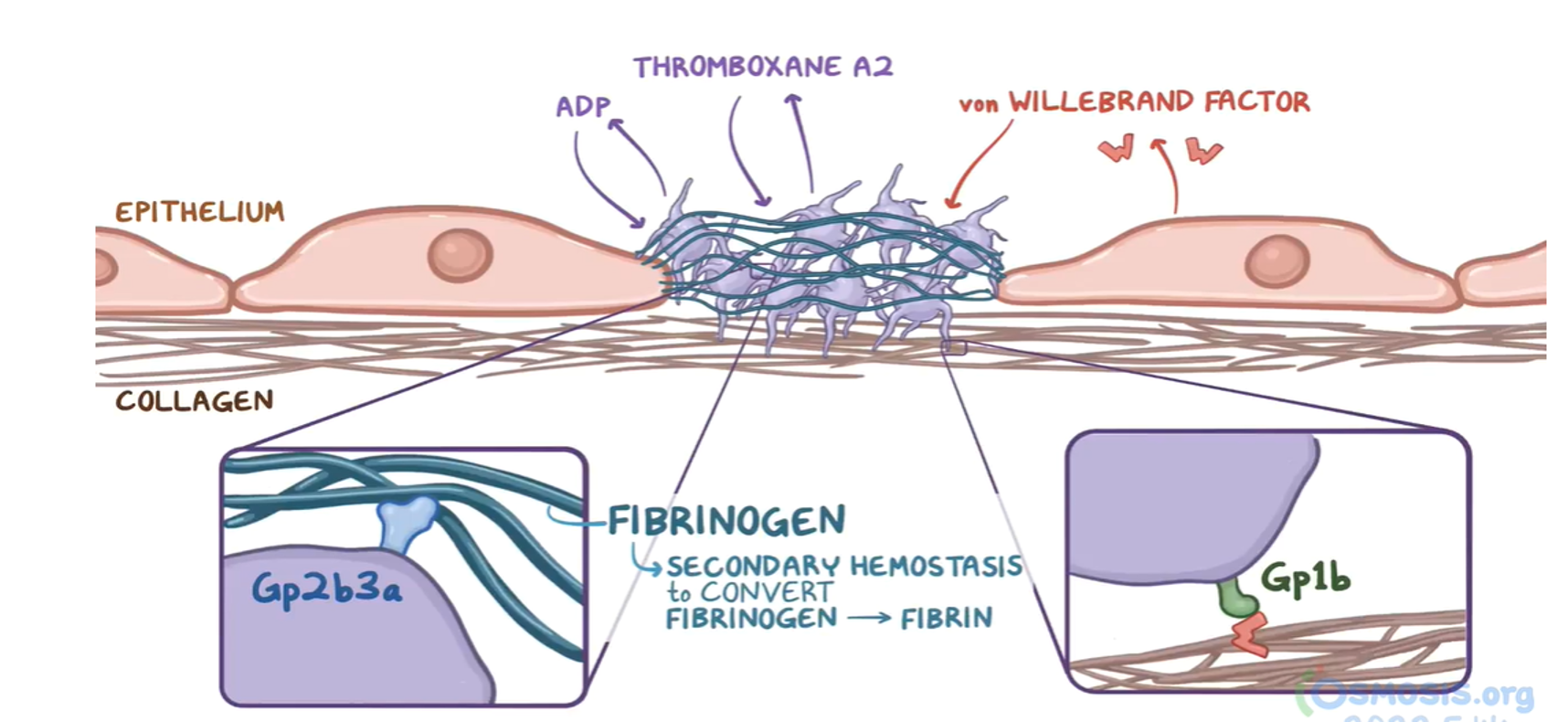 VWF: Made in the endothelium and stored in weibel-palade bodies
VWF: Made in the endothelium and stored in weibel-palade bodies
Types of vWDY
- Type 1 (80% of cases): Partial reduction in vWF. Autosomal dominant inheritance. Mildest form.
- Type 2: Abnormal form of vWF. Autosomal dominant inheritance.
- Type 2A: Defective platelet adhesion.
- Type 2B: Increased VWF-platelet interaction.
- Type 2M: Decreased VWF-platelet interaction.
- Type 2N: Abnormal binding of VWF to factor VIII.
- Type 3: Total lack of vWF. Autosomal recessive inheritance. Most severe form.
Etiology
- Hereditary: Mutations in the vWF gene.
- Acquired (Pseudo-vWD): Associated with various conditions, including:
- Lymphoproliferative and myeloproliferative disorders
- Solid tumors
- Immunological disorders
- Cardiovascular disorders (e.g., aortic stenosis)
- Wilms’ tumor
- Hypothyroidism
Clinical Features
- Highly variable.
- Type 1 and 2: Mild bleeding, epistaxis, menorrhagia. Hemarthroses are rare.
- Type 3: More severe bleeding, but joint and muscle bleeds are less common than in hemophilia A.
Diagnostic Considerations
-
History: Recurrent bleeding episodes since childhood, often with a positive family history.
-
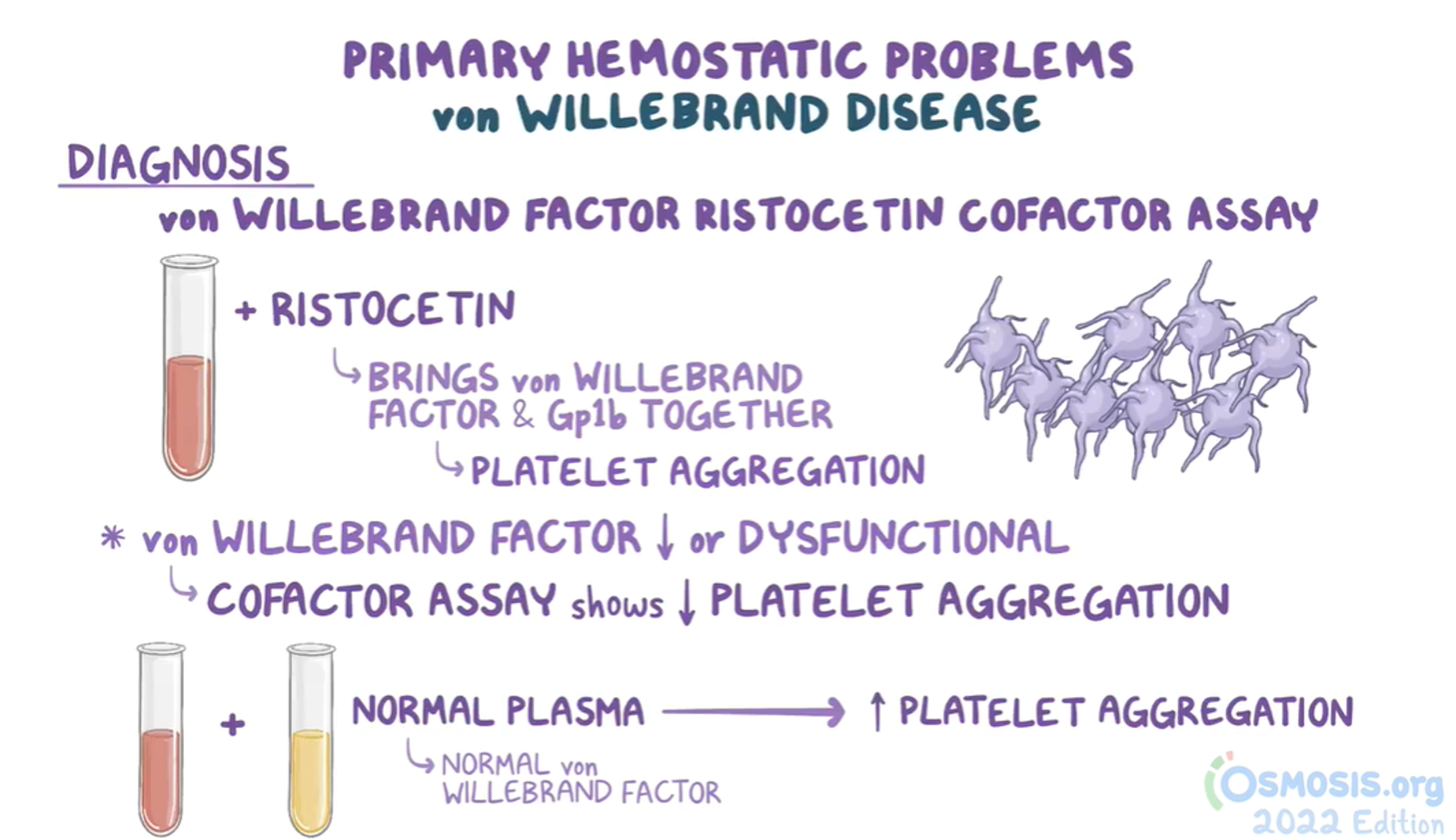
Lab Tests:
- CBC: Anemia, Normal platelet count
- Prolonged bleeding time (normal)
- Prolonged aPTT (in about 50% of cases, due to low FVIII); because one of the normal functions of vWF is to protect FVIII from degradation.
- Reduced factor VIII levels
- Decreased vWF antigen levels (Type 1)
- Normal vWF antigen levels (Type 2)
- Ristocetin cofactor assay: Failure of platelet aggregation
- Bleeding time; prolonged - Historically, diagnostic test
-
Diagnostic Consideration: Conditions to consider in the differential diagnosis of von Willebrand’s disease include the following:
- Hemophilia A, B, C
- Platelet function defects
- Antiplatelet drug ingestion
- Fibrinolytic defects
- Pseudo-vWD
Treatment & Management
-
Desmopressin (DDAVP): Stimulates vWF release. Effective for mild/moderate Type 1 and some (you can try) Type 2 cases. Not effective for Type 3.
-
Factor VIII concentrates containing vWF: Mainstay of replacement therapy for severe bleeding, prophylaxis for surgery, and in cases where DDAVP is ineffective.
-
Cryoprecipitate:
- Source of fibrinogen, factor VIII and VWF
- Only plasma fraction contains VWF multimers consistently
- indicated for severe bleeding, as prophylaxis for surgical procedures and if DDAVP treatment is ineffective
- not virus-inactivated.
Contains vWF but is less preferred due to the risk of viral transmission.
-
Antifibrinolytics (e.g., tranexamic acid): vAminocaproic acid and tranexamic acid Indication: prior to dental procedure, nose and mouth bleeds, and for menorrhagia.
- vOral contraceptives for menorrhagia
-
Oral contraceptives: May help with menorrhagia.
Increased Risk
Avoid platelet aggregation inhibitors (e.g., aspirin, NSAIDs): (e.g., aspirin, NSAIDs, clopidogrel) and intramuscular injections are contraindicated in VWD because they further increase the risk of bleeding!
Medications & bleeding
- Unfractionated heparin: antidote protamine sulfate (Intrinsic) aptt
- Low-molecular W heparin: protamine sulfate works incompletely. (Intrinsic) aptt
- Warfarin: ↑ PT, inhibits liver enzyme vitamin K epoxide reductase, (1972) + protein C and S. (Extrinsic) pt
Treatment of warfarin-related bleeding depends on the acuity of the bleed.
-
Slowly growing thigh hematoma: vitamin K and fresh frozen plasma – (higher volume and infused slowly )- taking effect over a couple of hours.
-
life-threatening intracerebral bleed, (low-volume prothrombin complex concentrates, contain (1972); rapidly and begins working within 15 minutes.
- Xa inhibitors and direct thrombin inhibitors: **prothrombin complex concentrates. **
Case :
An 18-year-old woman comes to her primary care provider because of menorrhagia over the last several years. She mentions that her menses “have always been heavy,”, and that she has experienced easy bruising for as long as she can remember. Her father has never had bleeding problems, but her mother has had similar problems with bruising easily. Initial lab studies show the following, platelet count: 205,000/ml, PT: 12 seconds, and PTT: 44 seconds. Of the following, which is the most likely cause of her symptoms?
Answer: Von Willebrand’s disease, given the family history and the characteristic bleeding pattern.
Reference: Kumar and Clark’s Clinical Medicine