Wilson’s Disease
Dr. Nada By the end of this lecture, the students should be able to:
- Define Wilson’s disease, its etiology & pathophysiology based on copper metabolism.
- Recognize and interpret symptoms & signs of Wilson’s disease.
- Enumerate and analyze the appropriate investigations for the workup of Wilson’s disease.
- Outline the management of Wilson’s disease.
Definition
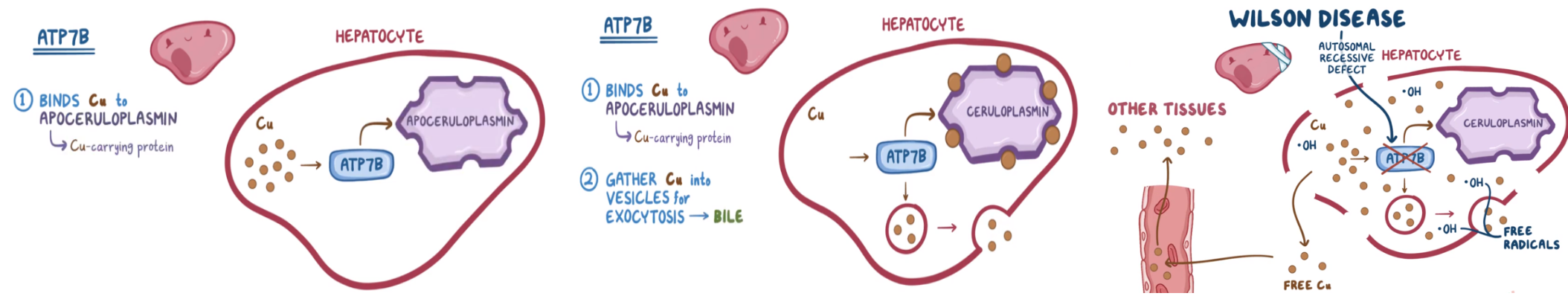
Wilson disease (WD) or (hepatolenticular degeneration) is an autosomal recessive disorder of impaired formation of ceruloplasmin, leading to copper accumulation in the liver, brain, kidney, and cornea.
Rare: approximately 15–30/100,000 per year
Copper Metabolism
Functions of copper
Copper is a cofactor for many proteins and copper containing enzymes involved in:
- Cellular respiration
- Antioxidant defense
- Pigment production
- Neurotransmitter formation
- Connective tissue synthesis
- Iron homeostasis
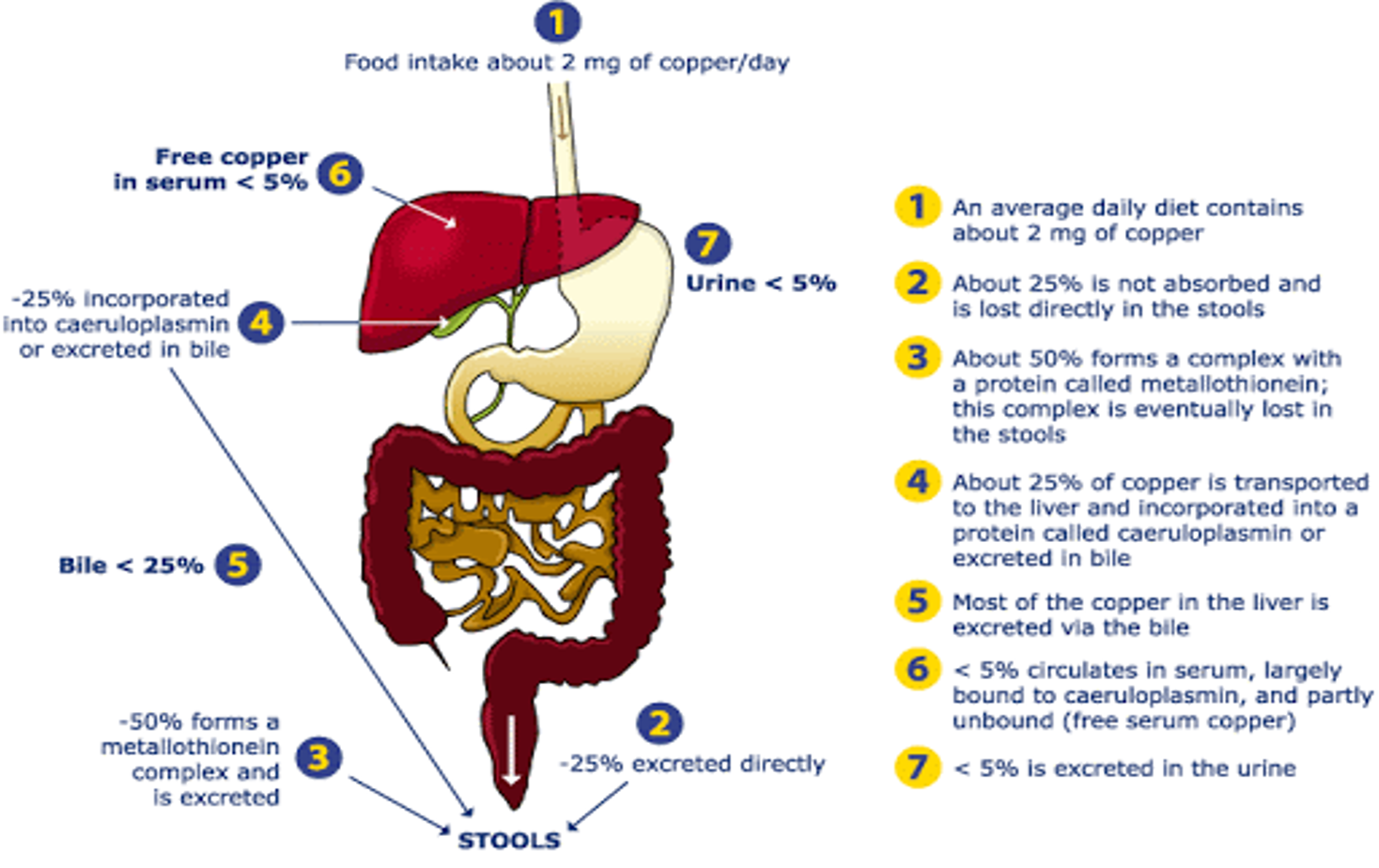 Metallothionein is a transport protein that facilitates copper absorption. Copper
Copper is used for pipes and roofing materials, in alloys, and as a pigment.
It is a component of several endogenous enzymes, including
tyrosinase and cytochrome oxidase and is essential for the utilization
of iron. Copper sulfate is used as a fungicide, an algicide, and
in some fertilizers.
Following ingestion, copper transport across the intestinal mucosa
is facilitated by cytosolic metallothionein. In blood, copper is initially
albumin-bound and transported via the hepatic portal circulation
to the liver where it is incorporated into caeruloplasmin. Ninety-eight
(98%) percent of copper in the systemic circulation is bound
to caeruloplasmin, and free copper is excreted via a lysosome-to-bile
pathway. This process is essential to normal copper homeostasis
and provides a protective mechanism in acute copper poisoning.
An impaired or overloaded biliary copper excretion system results
in hepatic copper accumulation, as occurs in Wilson’s disease (see
Chapter 12.7.2) and copper poisoning.
Free reduced Cu(I) can bind to sulfhydryl groups and inactivates
enzymes such as glucose-6-phosphate dehydrogenase and glutathione
reductase. In addition, copper may interact with oxygen species
(e.g., superoxide anions and hydrogen peroxide) and catalyze the
production of reactive toxic hydroxyl radicals. Copper(II) ions can
oxidize haem iron to form methaemoglobin.
Metallothionein is a transport protein that facilitates copper absorption. Copper
Copper is used for pipes and roofing materials, in alloys, and as a pigment.
It is a component of several endogenous enzymes, including
tyrosinase and cytochrome oxidase and is essential for the utilization
of iron. Copper sulfate is used as a fungicide, an algicide, and
in some fertilizers.
Following ingestion, copper transport across the intestinal mucosa
is facilitated by cytosolic metallothionein. In blood, copper is initially
albumin-bound and transported via the hepatic portal circulation
to the liver where it is incorporated into caeruloplasmin. Ninety-eight
(98%) percent of copper in the systemic circulation is bound
to caeruloplasmin, and free copper is excreted via a lysosome-to-bile
pathway. This process is essential to normal copper homeostasis
and provides a protective mechanism in acute copper poisoning.
An impaired or overloaded biliary copper excretion system results
in hepatic copper accumulation, as occurs in Wilson’s disease (see
Chapter 12.7.2) and copper poisoning.
Free reduced Cu(I) can bind to sulfhydryl groups and inactivates
enzymes such as glucose-6-phosphate dehydrogenase and glutathione
reductase. In addition, copper may interact with oxygen species
(e.g., superoxide anions and hydrogen peroxide) and catalyze the
production of reactive toxic hydroxyl radicals. Copper(II) ions can
oxidize haem iron to form methaemoglobin.
Aetiology
It is caused by mutations in the ATP7B gene on chromosome 13q14.3, which encodes a copper-transporting ATPase.
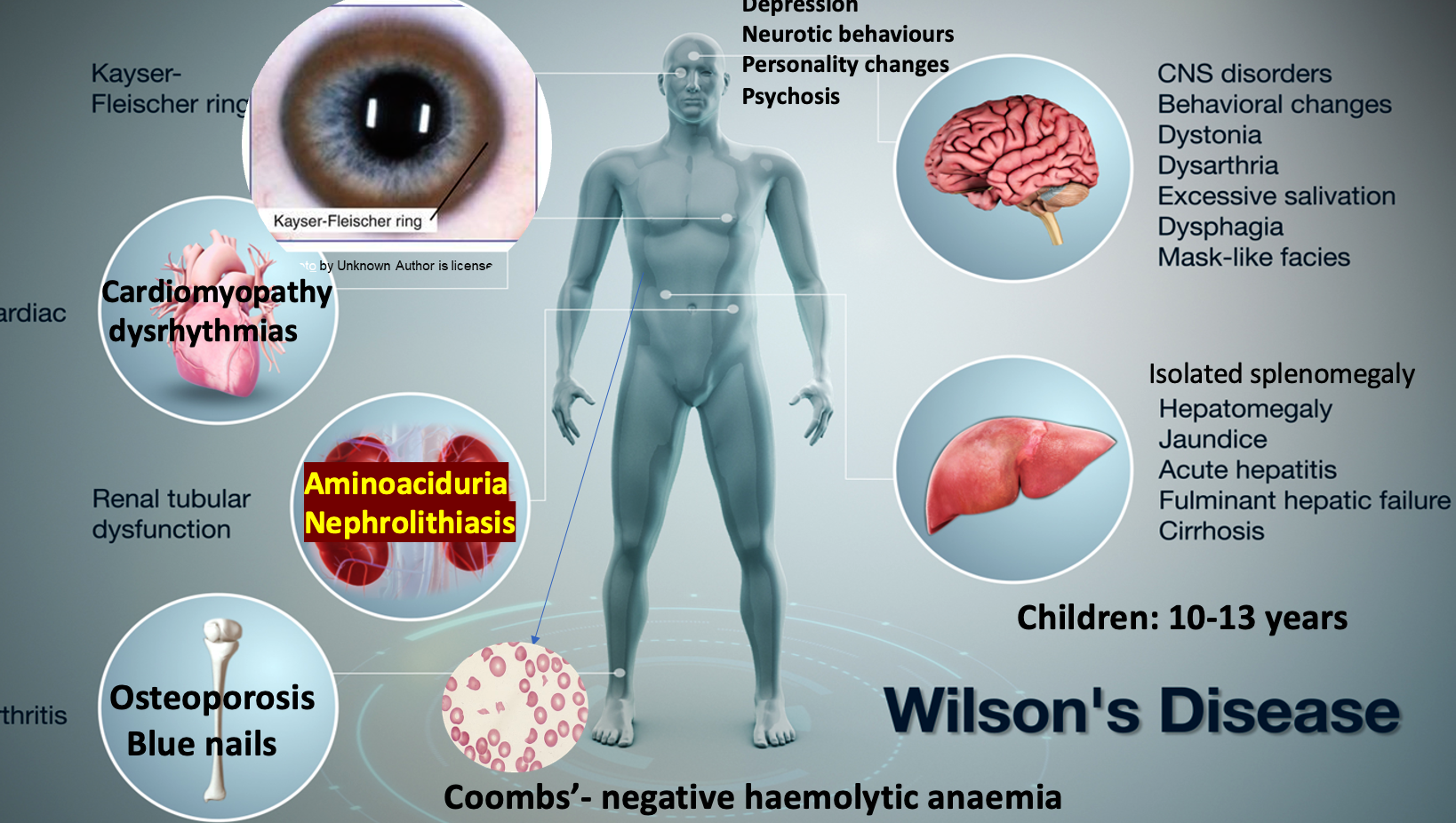
- Isolated splenomegaly
- Children: 10-13 years
- Coombs’-negative haemolytic anaemiaZ
- Depression
- Neurotic behaviours
- Personality changes
- Psychosis
- Aminoaciduria
- Nephrolithiasis
- Osteoporosis
- Blue nails
- Cardiomyopathy
- Dysrhythmias
- Movement disorders (tremor, involuntary movements)
- Pseudobulbar palsy
- Dysautonomia
- Migraine headaches
- Insomnia
- Seizures
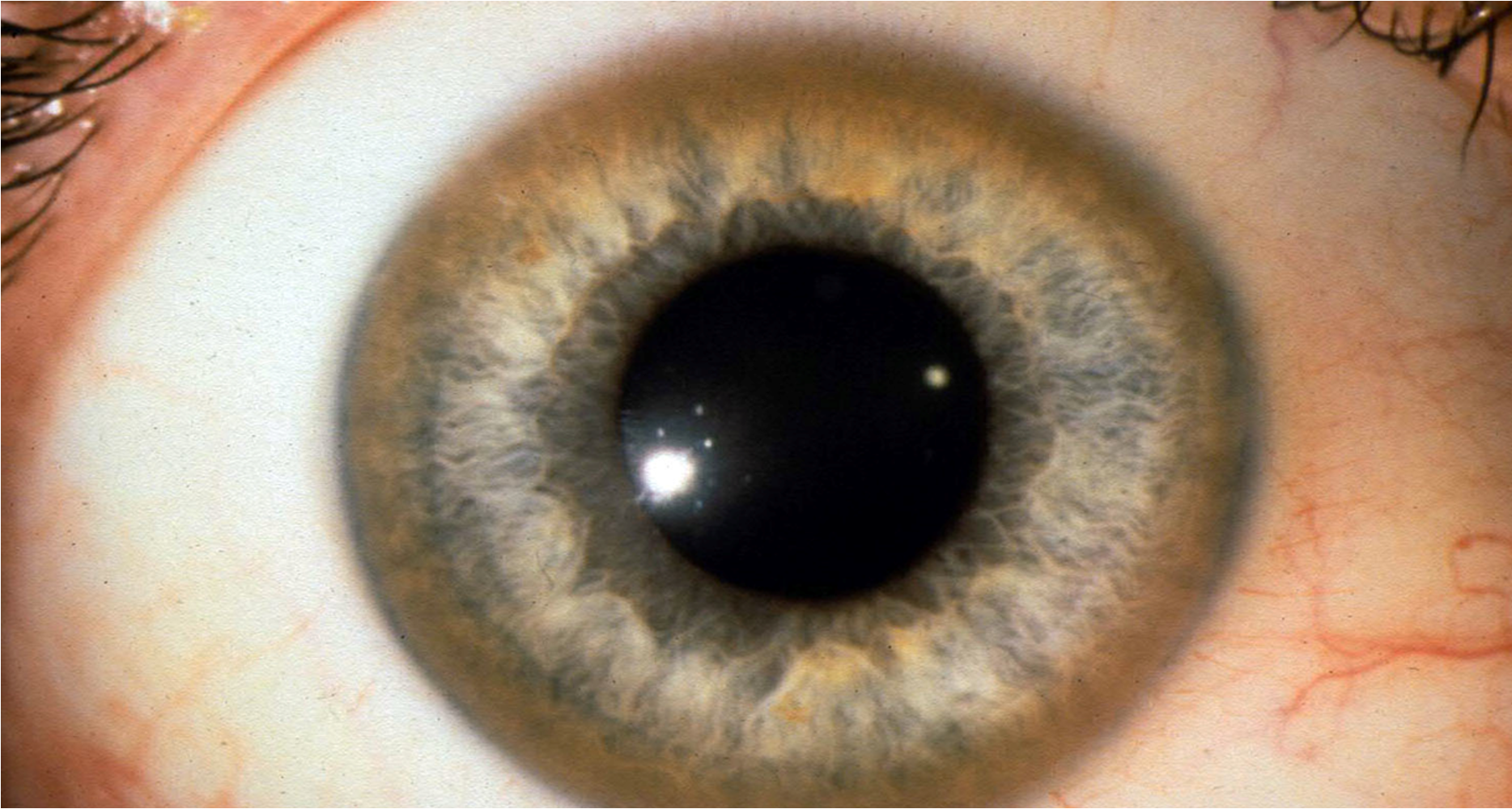
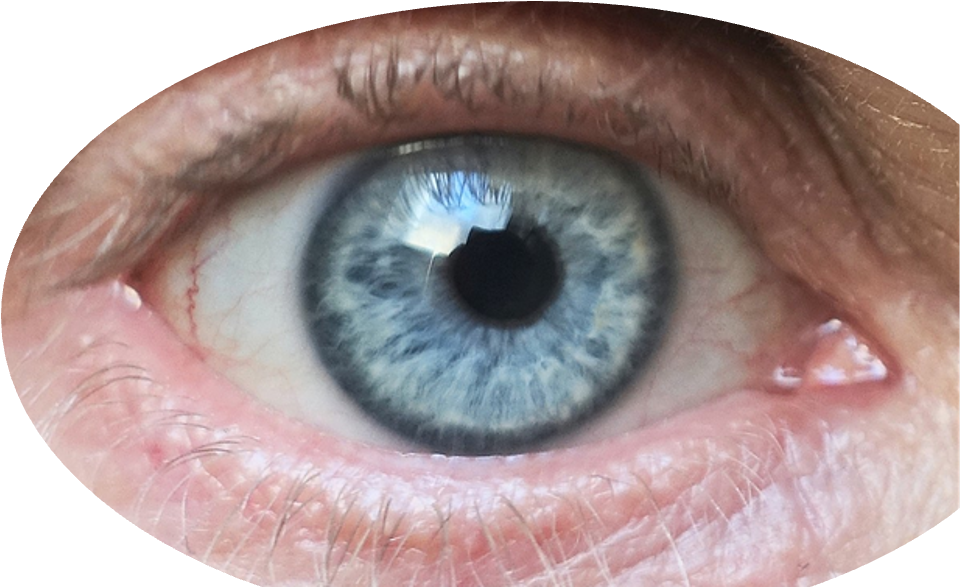
Kayser–Fleischer rings are present in approximately 95% of patients with a neurological presentation but in only approximately 40 to 50% of patients with predominant hepatic disease at the time of diagnosis.
Liver disease
Occur: 10 and 13 years
- Asymptomatic hepatomegaly
- Isolated splenomegaly
- Persistently elevated liver enzymes
- Fatty liver
- Acute hepatitis - autoimmune hepatitis
- Cirrhosis—compensated or decompensated
- Fulminant hepatic failure
Movement disorders (tremor, involuntary movements)
- Drooling, dysarthria
- Rigid dystonia
- Pseudobulbar palsy
- Dysautonomia
- Migraine headaches
- Insomnia
- Seizures
Investigations
- Haemolysis and anaemia
- Liver biopsy
- Liver copper concentration: measurement of the amount of copper in the liver (>250 μg/g dry weight).
- Genetic analysis
- Brain MRI
- Rhodanine staining of the cytoplasmic granules of the liver.
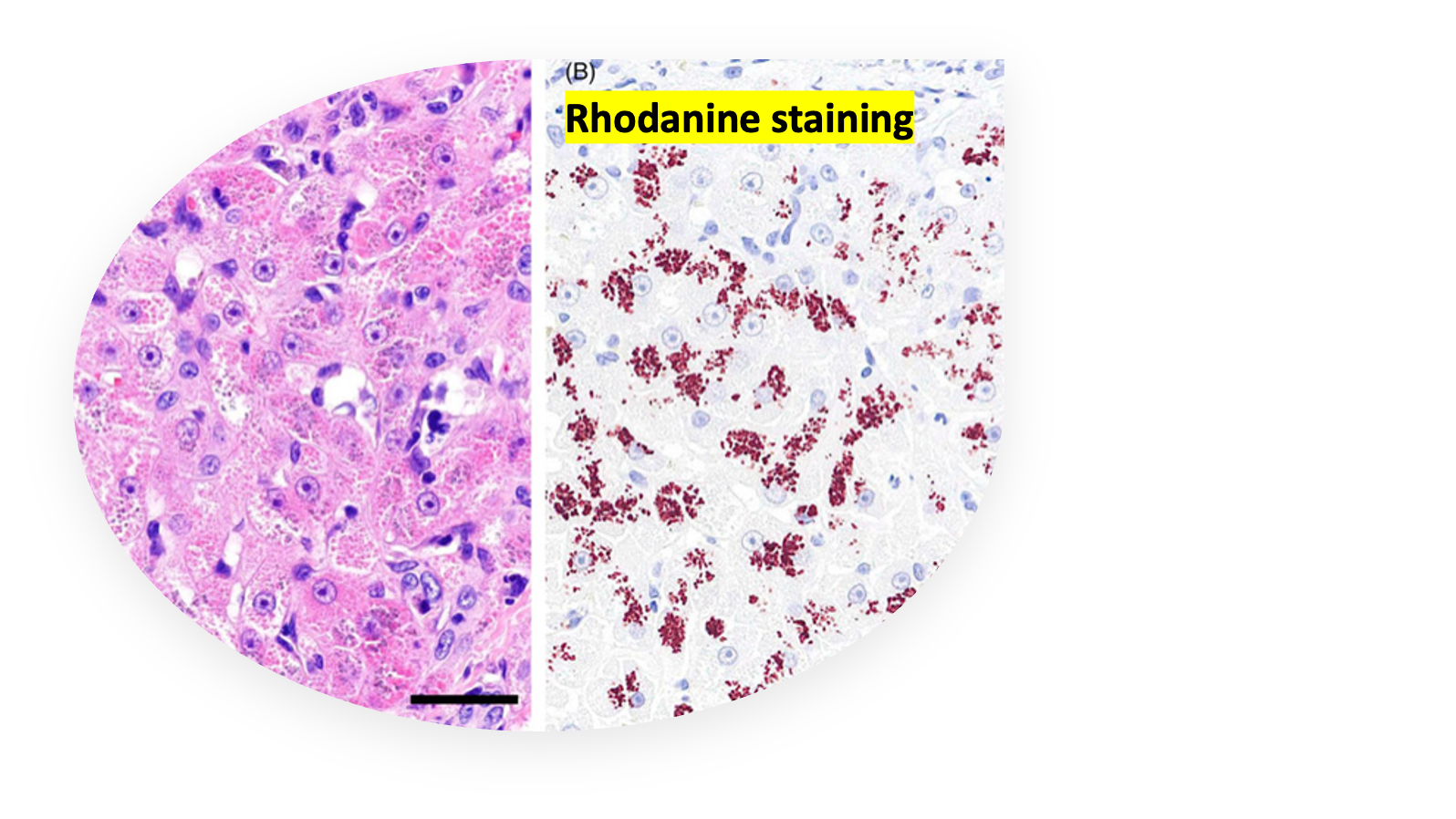 Rhodanine staining
A, The hepatocytes were swollen, and several eosinophilic cytoplasmic granules were observed. B, The granules were stained red to brown on rhodanine staining.
Rhodanine staining
A, The hepatocytes were swollen, and several eosinophilic cytoplasmic granules were observed. B, The granules were stained red to brown on rhodanine staining.
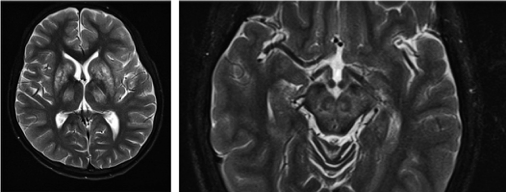 Bilateral abnormal signal in the striatum and thalamus in Wilson’s disease (left) and ‘face of the giant panda’ (right) on T2 weighted MRI sequences in Wilson’s disease.
Bilateral abnormal signal in the striatum and thalamus in Wilson’s disease (left) and ‘face of the giant panda’ (right) on T2 weighted MRI sequences in Wilson’s disease.
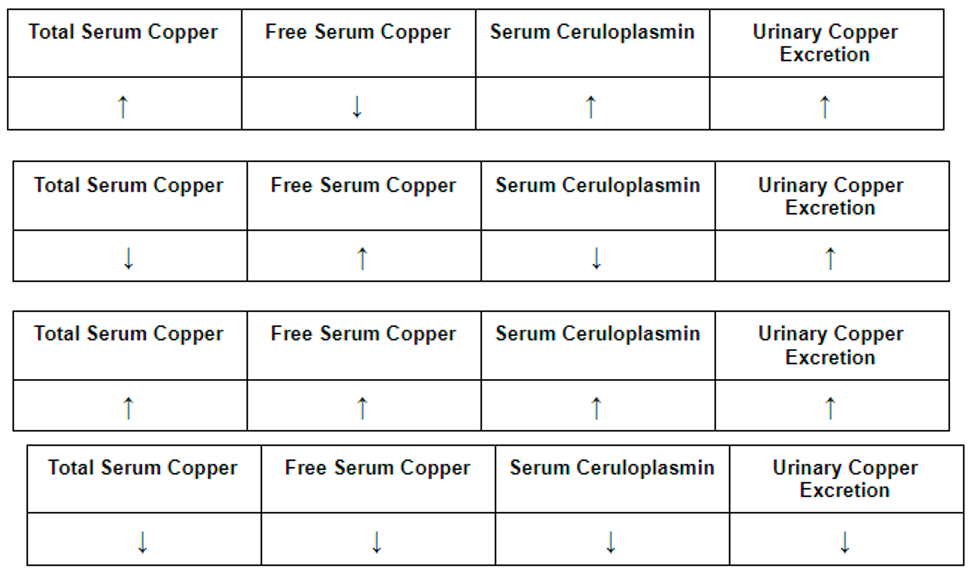
Diagnostic Investigations
| Wilson disease | |
|---|---|
| Serum aminotransferase | ↑↑ |
| Caeruloplasmin level | ↓↓ |
| Serum Copper | ↓↓ |
| Urinary copper | ↑↑ (100–1000 μg/day) normal < 40 |
Management & Prognosis
felong treating with copper chelating Agent
-
Trientine hydrochloride:
-
Zinc acetate (Children)
-
↓ Dietary copper: chocolate & peanuts
-
Penicillamine
- Dose: 1–1.5 g daily
- Monitor: Urinary copper levels
- Side/effects:
- Proteinuria
- Skin rashes
- Leukopenia
- Myasthenia Gravis
-
Liver cirrhosis/acute failure: Liver transplant
Good prognosis: Early diagnosis and effective treatment.
Neurological: permanent.
Case scenario
A 30-year-old man admitted for the evaluation of personality changes. At work, he has recently gotten into several heated arguments with colleagues and has missed several deadlines.” He does not consume alcohol, tobacco, or illicit substances. Family history is notable for “liver disease” in his maternal uncle and grandfather, but he is unaware of additional details. Physical examination reveals greenish-brown rings around the iris. The liver is palpated 4 cm below the right costal margin. Resting tremors are present in the bilateral hands. Which of the following sets of laboratory values would most likely be seen in this patient?
second image
Case scenario
26 years hx speech behavioral problem lethargy, jaundiced sclera, most likely
A) Wiskott-Aldrich Syndrome B) Haemochromatosis C) Friedreich’s ataxia D) Wilson’s disease E) Acute intermittent Porphyria; no skin manifestations - diff of acute abdominal pain; DKA, IM - lead poisoning, SCDZ Diff Abd Pain OSCE surgical vs non-surgical differentiation
17 yrs man admitted w/ personality change, diff speaking, impaired balance, bitals normal, loss coordination, dysarthric speech, slit lamp showed KF ring - which
atrophy brain
insulin resistance, hypogonadism, tumor in adrenal medulla, basal ganglia atrophy on brain imaging
22 yrs woman presented tremor, clumsy gait, worsened 4 months - non contributory, vital normal, flat effect; depression - liver palpated 4 cm below costal margin mildly tender. no palmar erythema, spider angiomata, ascites
green brown rengs in prepihry of…