IM
Adrenal Insufficiency: Addison’s Disease
H M ABDELRAHIM
Understanding Adrenal Insufficiency
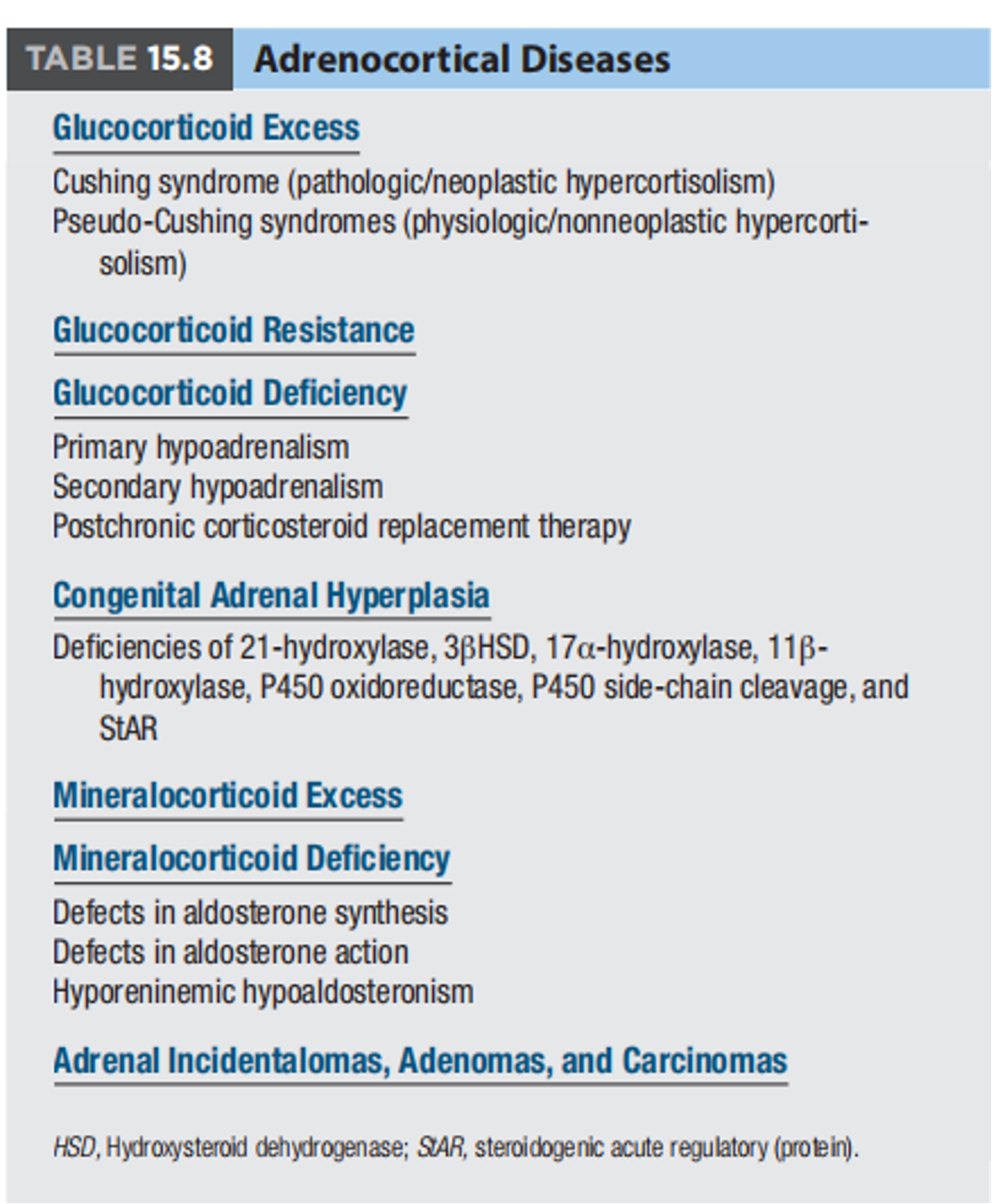
Adrenal insufficiency occurs when the adrenal glands fail to produce sufficient amounts of hormones, primarily cortisol and aldosterone.
There are two main types:
-
Primary Adrenal Insufficiency (Addison’s Disease): The adrenal glands themselves are damaged and cannot produce enough hormones.
-
Secondary Adrenal Insufficiency: The pituitary gland fails to produce enough adrenocorticotropic hormone (ACTH), which stimulates the adrenal glands. This is often due to prolonged use of exogenous steroids.
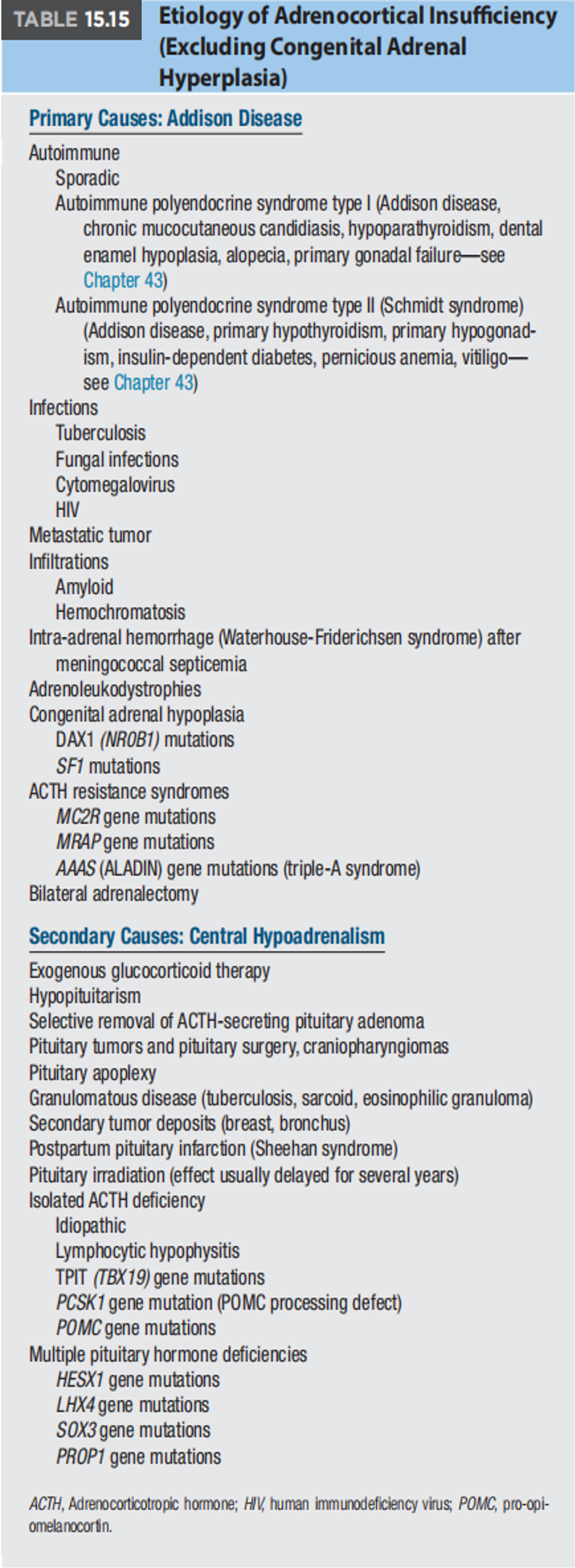
Causes of Adrenal Insufficiency
Primary Adrenal Insufficiency (Addison’s Disease)
- Autoimmune Disease: The most common cause, where the body’s immune system attacks the adrenal glands.
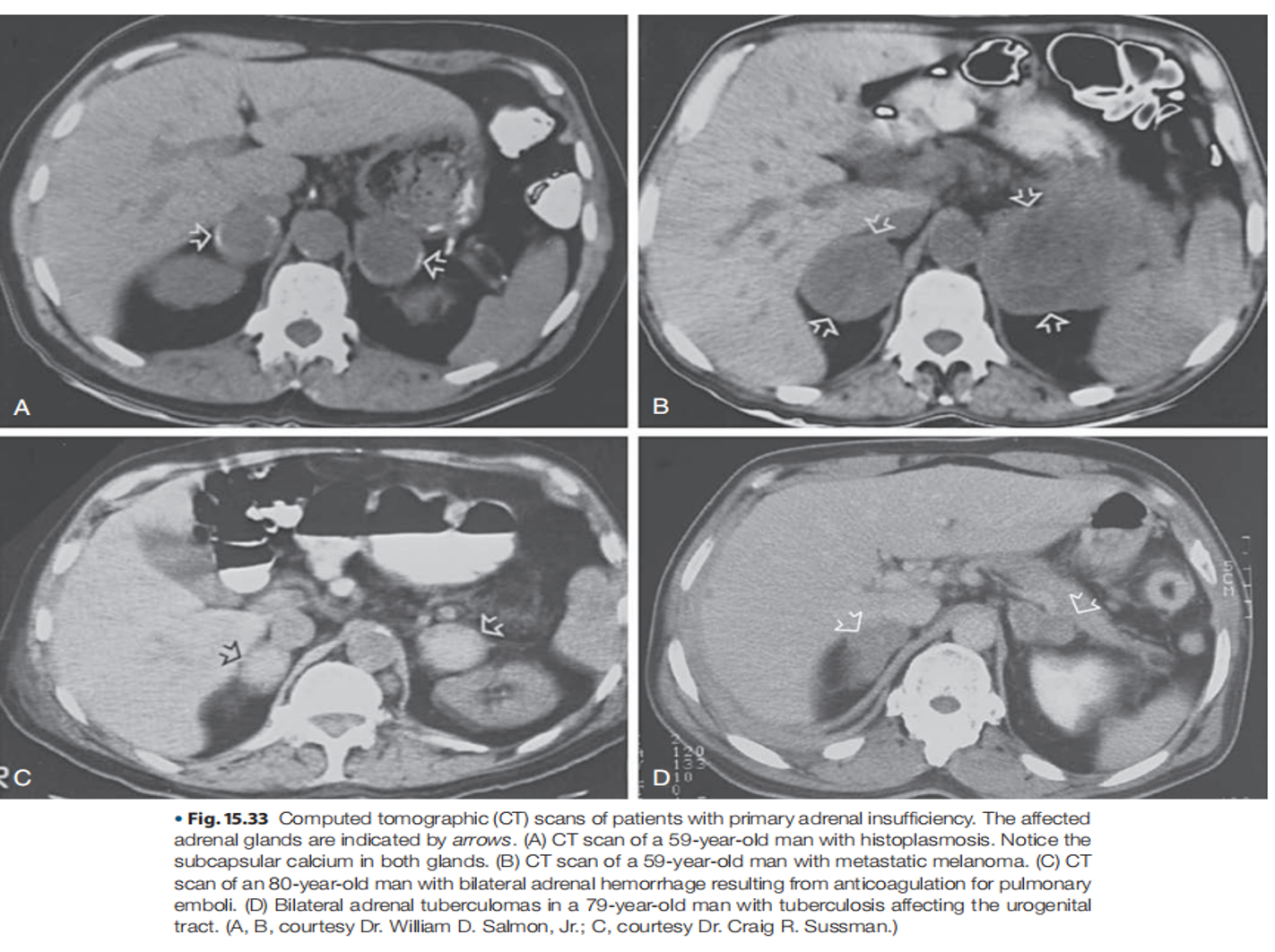
- Infections: Tuberculosis, fungal infections, and HIV can damage the adrenal glands.
- Hemorrhage: Bleeding into the adrenal glands, often seen in conditions like Waterhouse-Friderichsen syndrome (associated with meningococcal infection).
- Surgical Removal: Bilateral adrenalectomy.
- Genetic Disorders: Rare genetic conditions can affect adrenal gland function.
Secondary Adrenal Insufficiency
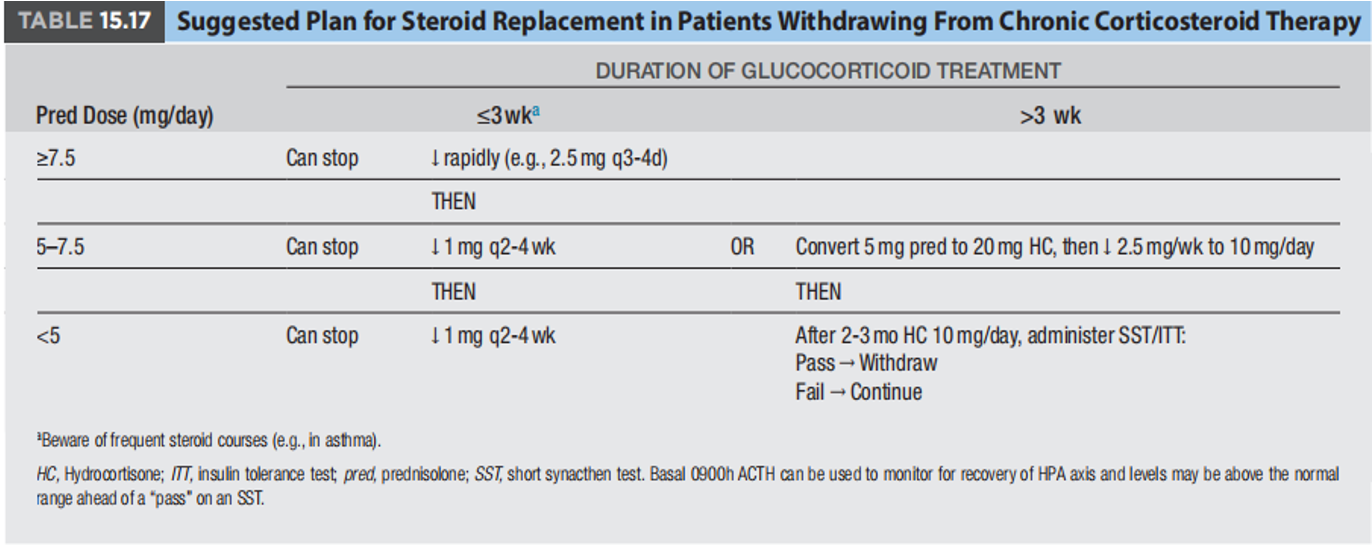
- Prolonged Use of Exogenous Steroids: Suppresses the hypothalamic-pituitary-adrenal (HPA) axis.
- Pituitary Tumors: Can interfere with ACTH production.
- Pituitary Surgery or Radiation.

Clinical Presentation
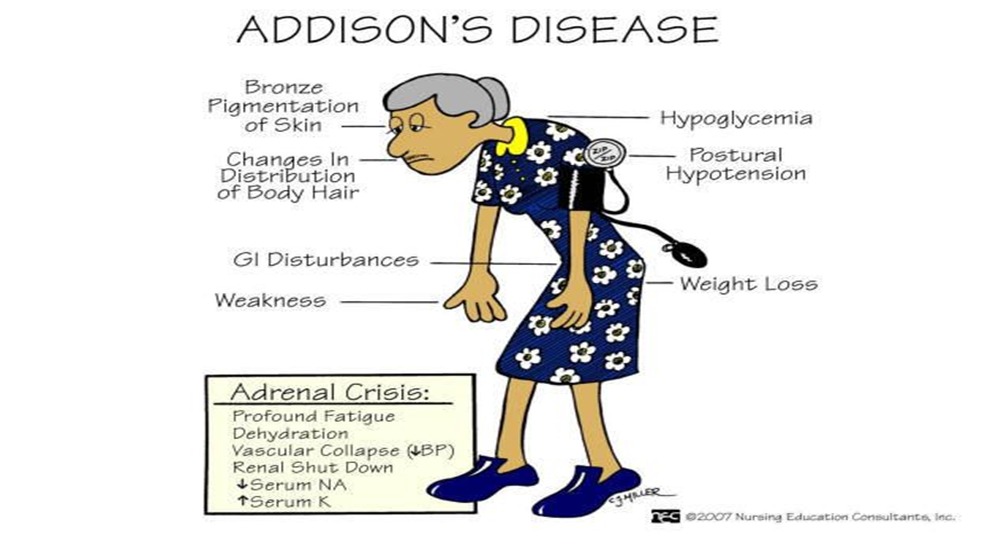
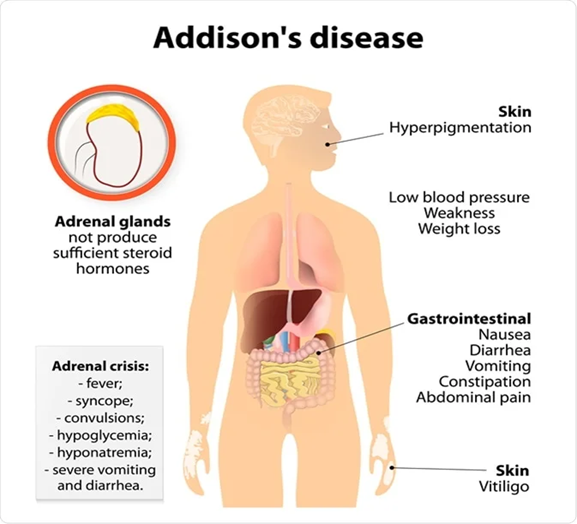
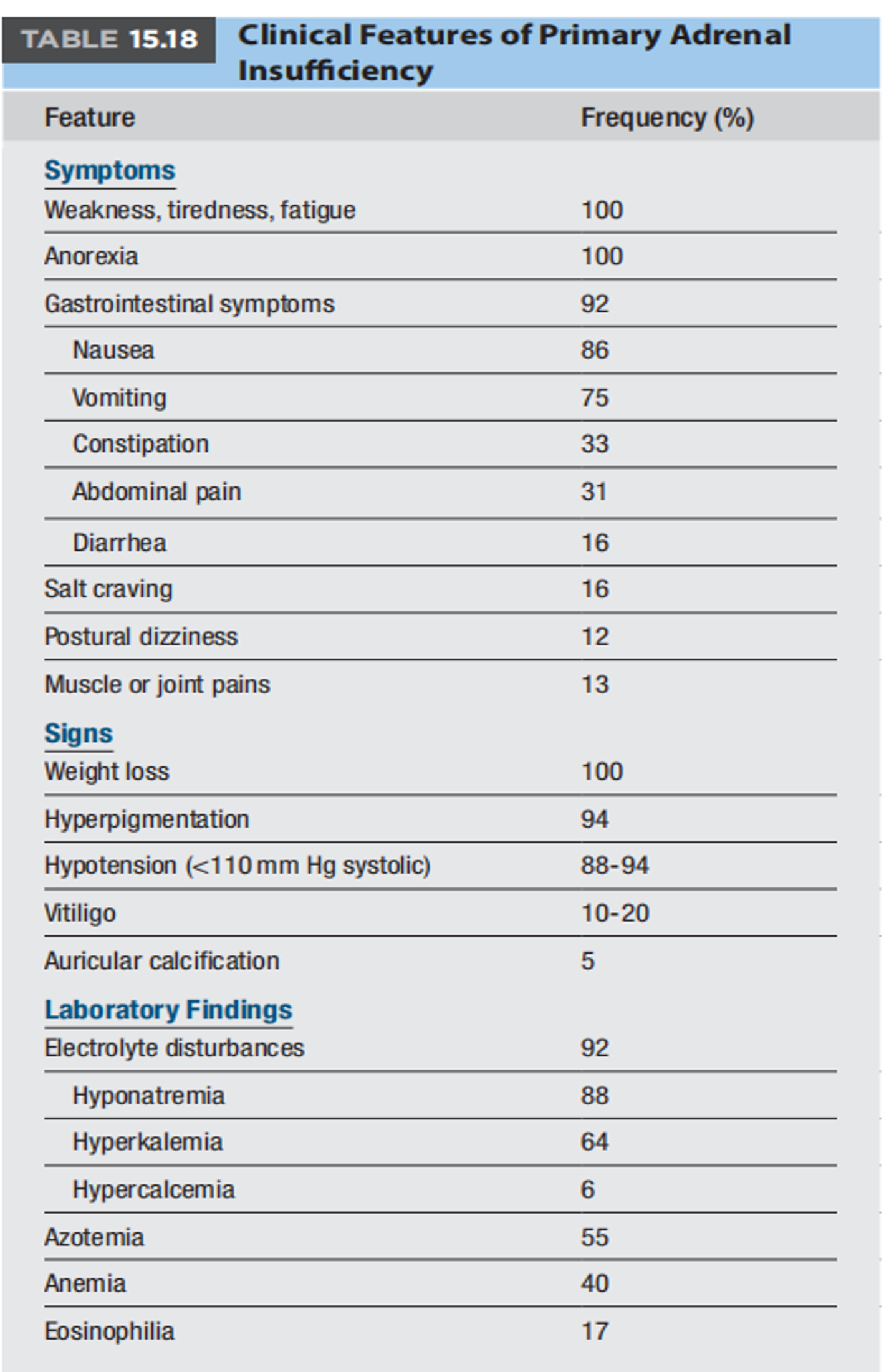
Symptoms Common to Both Primary and Secondary Adrenal Insufficiency:
- Weakness and Fatigue
- Hypotension (Low Blood Pressure)
- Nausea, Vomiting, and Diarrhea
- Weight Loss
- Hypoglycemia (Low Blood Sugar)
Clinical manifestations of adrenal insufficiency differ based on whether or not the cause is primary or secondary adrenal insufficiency
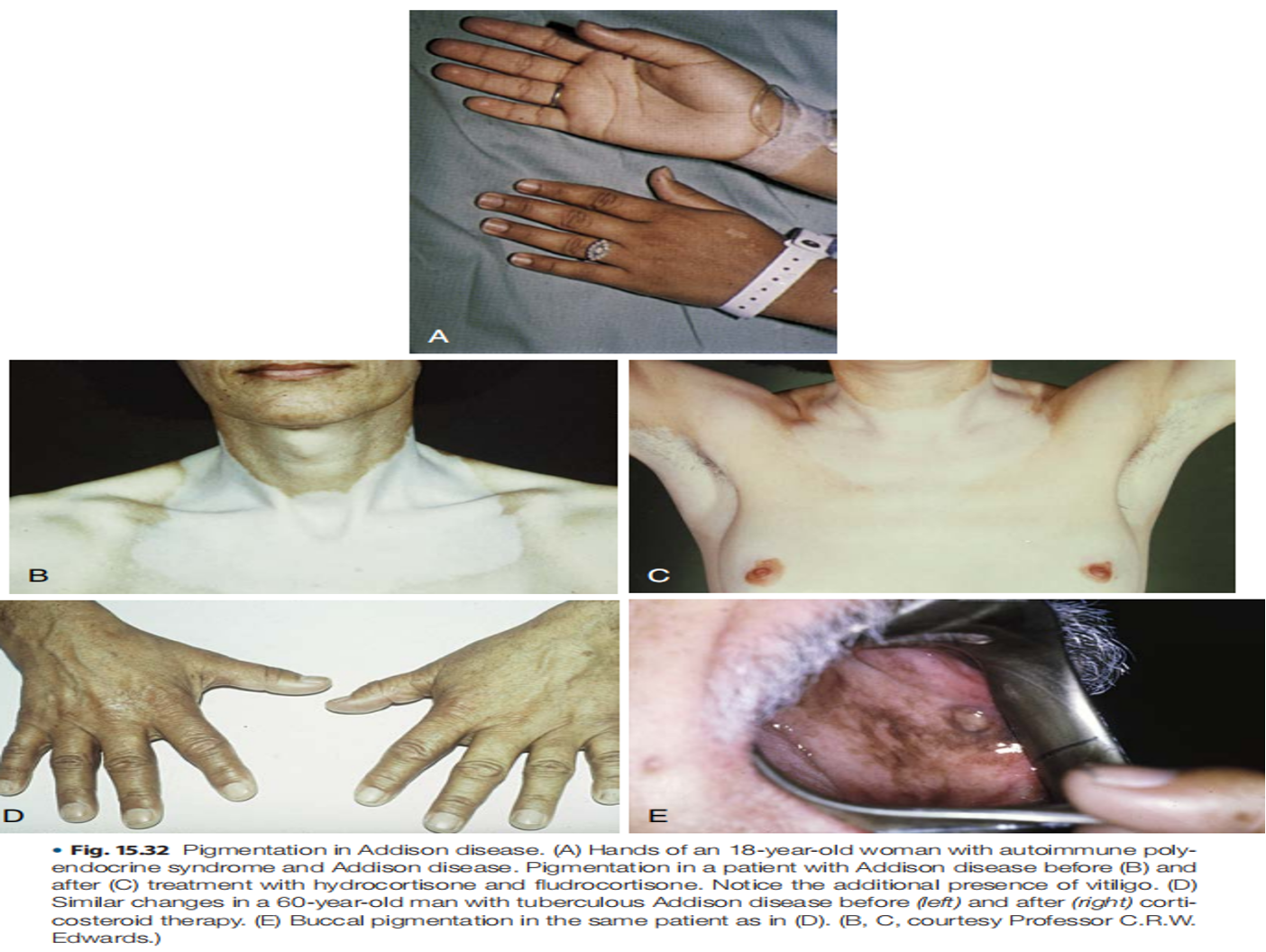
With primary adrenal insufficiency, the hypothalamus will respond by increasing CRH production, resulting in increased production of pro-opiomelanocortin (the ACTH precursor) and increased serum levels of ACTH
Clinical manifestations shared by all patients with adrenal insufficiency include weakness, hypotension, nausea, vomiting, diarrhea, and weight loss
Acute adrenal insufficiency, which is a medical emergency, can be precipitated in patients with chronic adrenal insufficiency who are exposed to stress (e.g., surgery, infection, gastroenteritis) or by rapid destruction of the adrenal glands (such as with hemorrhage) or pituitary apoplexy
Distinguishing Symptoms of Primary Adrenal Insufficiency (Addison’s Disease):
- Hyperpigmentation: Darkening of the skin and mucous membranes due to increased production of proopiomelanocortin (POMC) and melanocyte-stimulating hormone (MSH). This is a key differentiating feature.
- Hyponatremia (Low Sodium) and Hyperkalemia (High Potassium) due to mineralocorticoid deficiency (aldosterone).
Hyponatremia is less common with secondary adrenal insufficiency and is seen more often if concomitant
central hypothyroidism is present
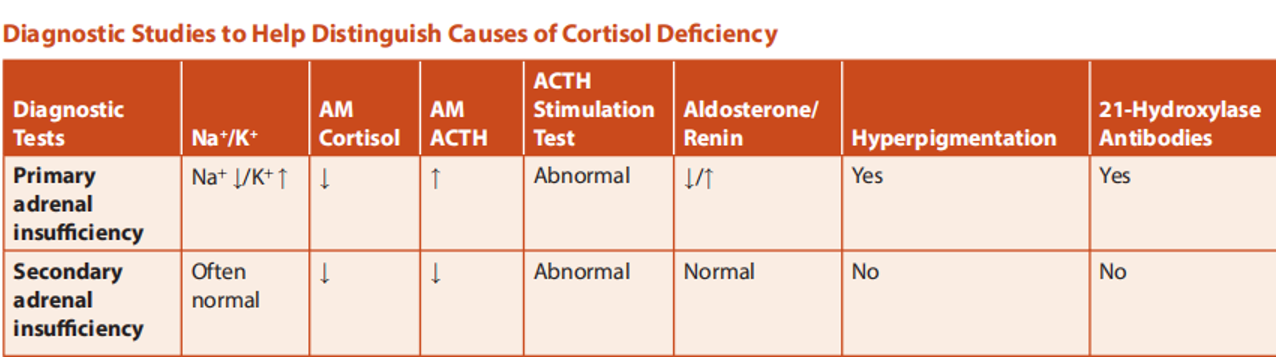
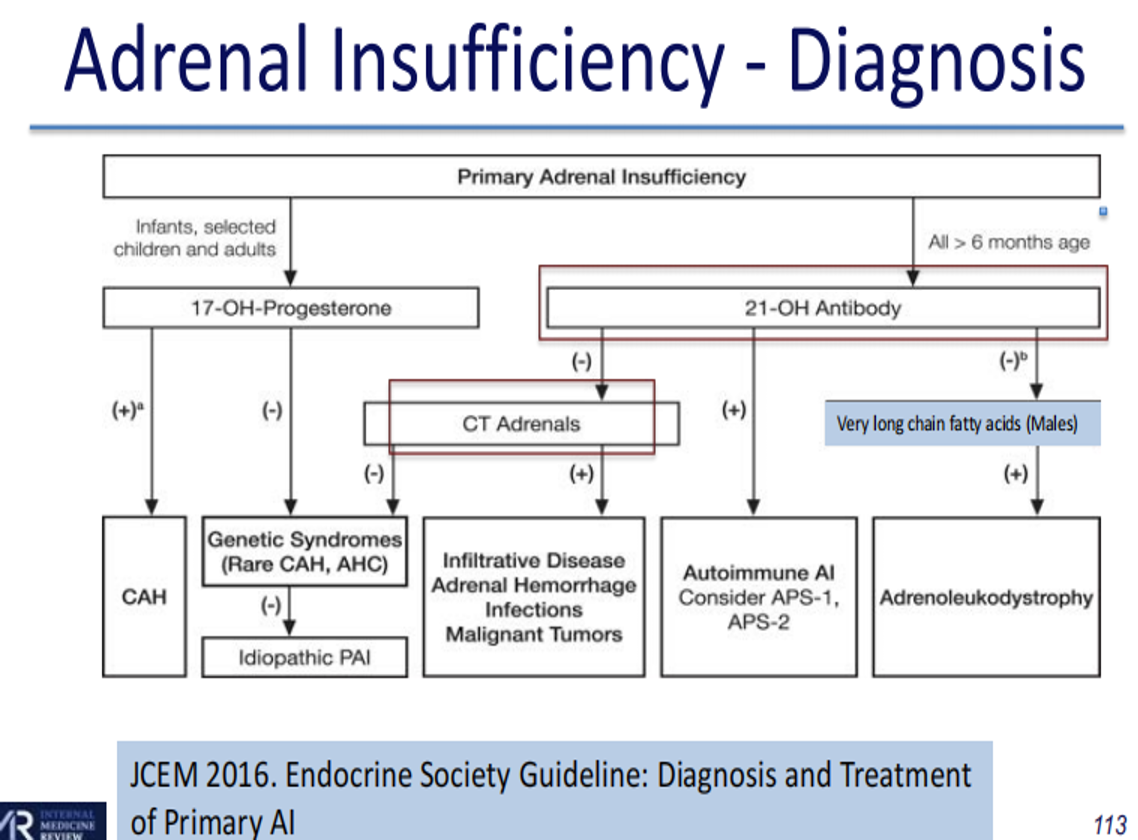
Diagnosis of Adrenal Insufficiency
Morning Cortisol Level: First start with 8 AM cortisol First start with 8 AM cortisol
- If < 80 nmol/L then AI very likely
- If > 500 nmol/L then AI unlikely When in between, usually need to do ACTH stimulation test
- Expect a rise in cortisol to > 500 at either 30 or 60 min
- If not, then diagnosis of AI is made Also measure ACTH
- If high, it is primary AI
- Check renin and aldosterone level to assess for mineralocorticoid deficiency
- If it is low or inappropriately normal, it is central AI
- ACTH Stimulation Test: The gold standard. Measures cortisol levels before and after administering synthetic ACTH (cosyntropin).
- Primary Adrenal Insufficiency: Low cortisol response with elevated ACTH levels.
- Secondary Adrenal Insufficiency: Low cortisol response with low or inappropriately normal ACTH levels.
- Insulin Tolerance Test (ITT): Measures cortisol response to induced hypoglycemia. Rarely used due to risks.
Tests: * Renin and Aldosterone Levels: To assess for mineralocorticoid deficiency in primary adrenal insufficiency. * ACTH Levels: To differentiate between primary and secondary adrenal insufficiency.
-
A random morning cortisol measurement may be insufficient to diagnose partial adrenal insufficiency because normal levels overlap with levels seen in mild adrenal insufficiency
-
However, if a patient is under significant stress (e.g., hypotensive or in the intensive care unit [ICU]) and a random cortisol (taken any time of day) is less than 15 µg/dL, the patient should be considered to be adrenally insufficient (unless serum albumin is less than 2.5 g/dL, as serum cortisol binding capacity is reduced)
-
All patients diagnosed with adrenal insufficiency based on a low serum cortisol while in the ICU should be restudied after the acute problem is solved
-
A very low serum morning cortisol level (less than 3 µg/dL) in an ambulatory patient is presumptive evidence of adrenal insufficiency
Gold-standard test of adrenal function is insulin induced hypoglycemia or insulin tolerance test
- Test performed by administering insulin (0.1 to 0.15 U/kg) intravenously (IV), with measurement of cortisol levels during symptomatic hypoglycemia
- A normal response is considered to be a peak cortisol level greater than 18 µg/dL
- ITT contraindicated in presence of coronary artery disease, seizure disorder, or age above 60 years
- Most commonly used test is ACTH stimulation test
- Administer ACTH (cosyntropin) 250 mg IV or intramuscularly
- Measure serum cortisol just before injection and 60 minutes following injection
- ***If cortisol level is 18.5 µg/dL or more at either measure, patient does not have adrenal insufficiency ***
- If cortisol levels stay below 18.5 µg/dL, adrenal insufficiency is present, and results are combined with ACTH levels, as described previously, to determine cause
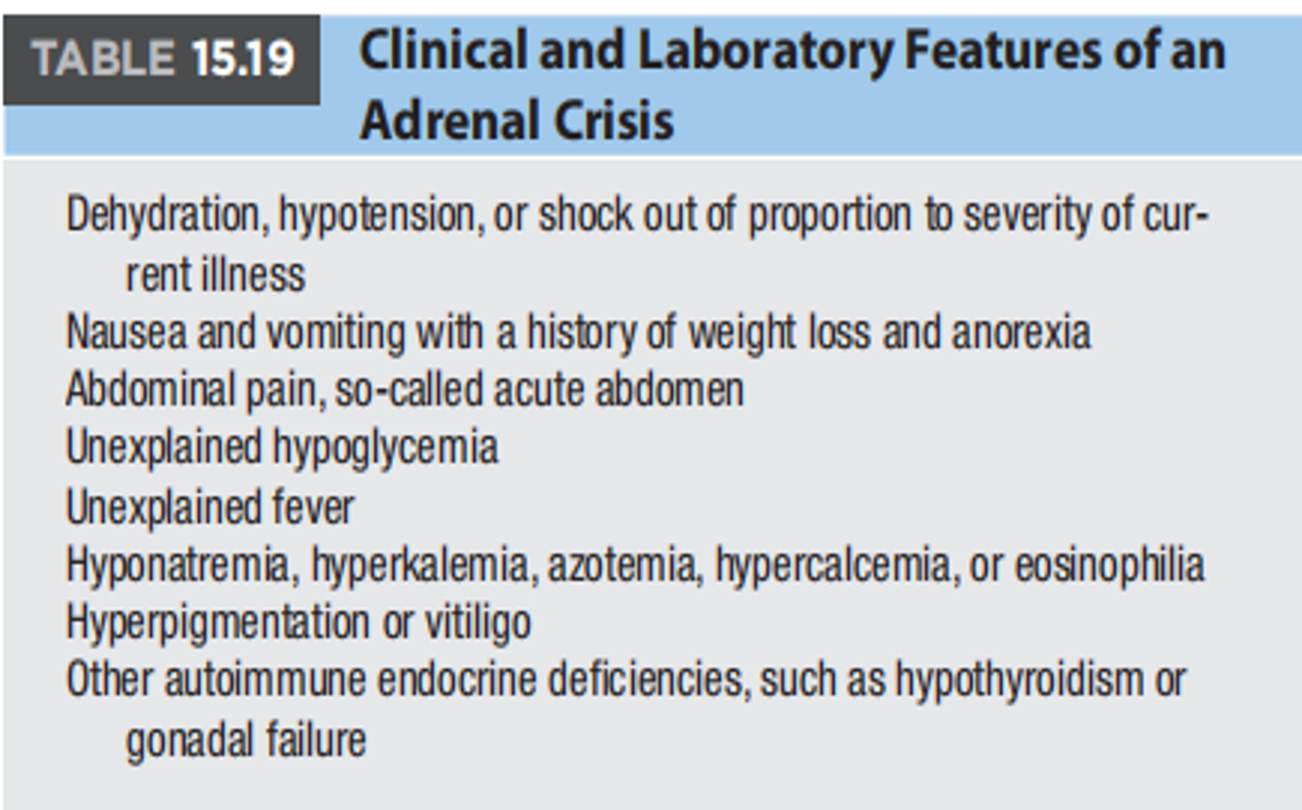
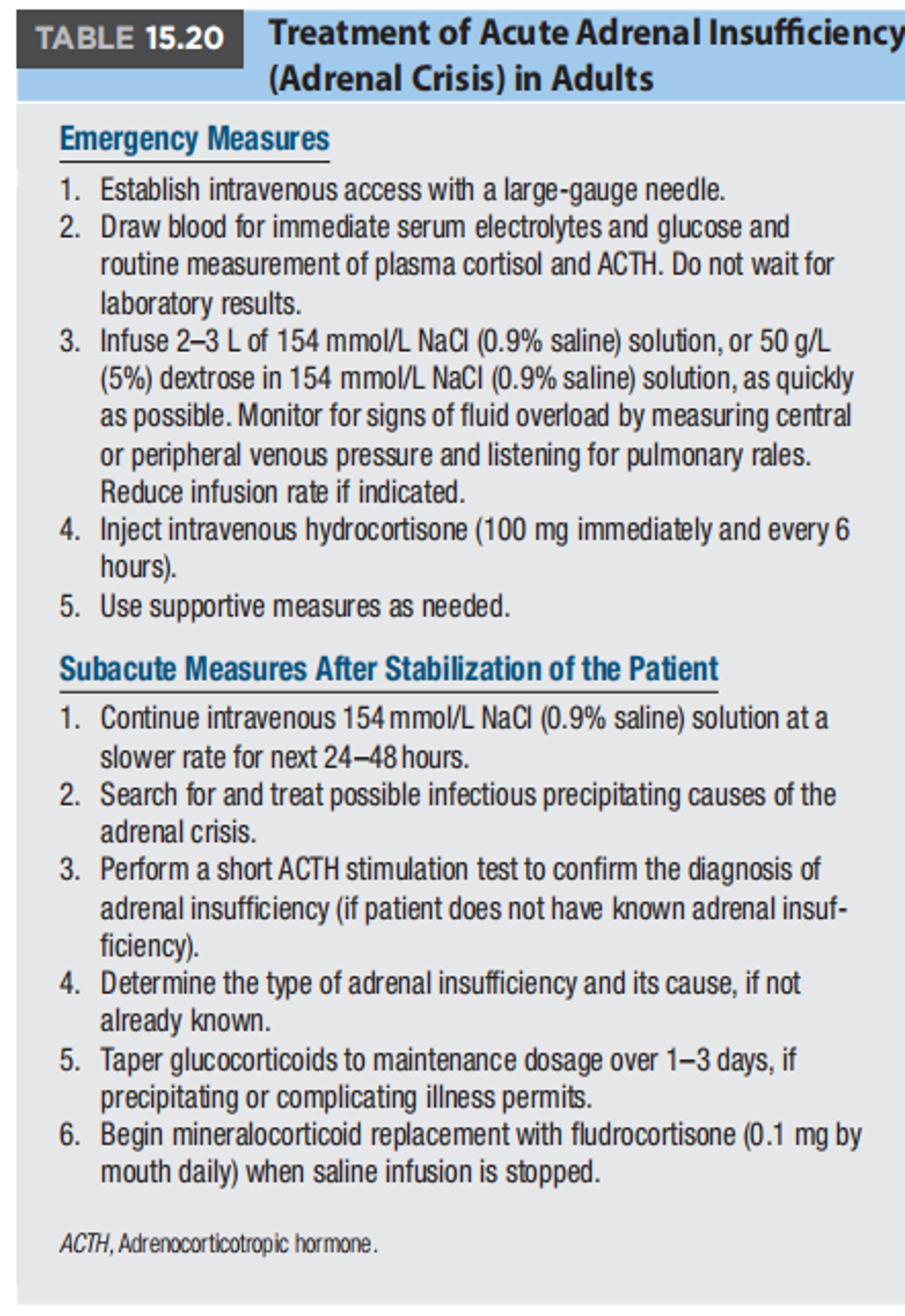
Acute Adrenal Crisis (Addisonian Crisis)
- A medical emergency that can be triggered by stress, infection, or surgery in patients with chronic adrenal insufficiency.
- Symptoms include:
- Severe Hypotension
- Shock
- Confusion
- Fever
Management of Adrenal Crisis
- Hydrocortisone 100mg IV load followed by 50mg IV Q6H
- IV hydration
- Identify precipitating cause
- Educate patients on sick day rules –advise MedicAlert bracelet
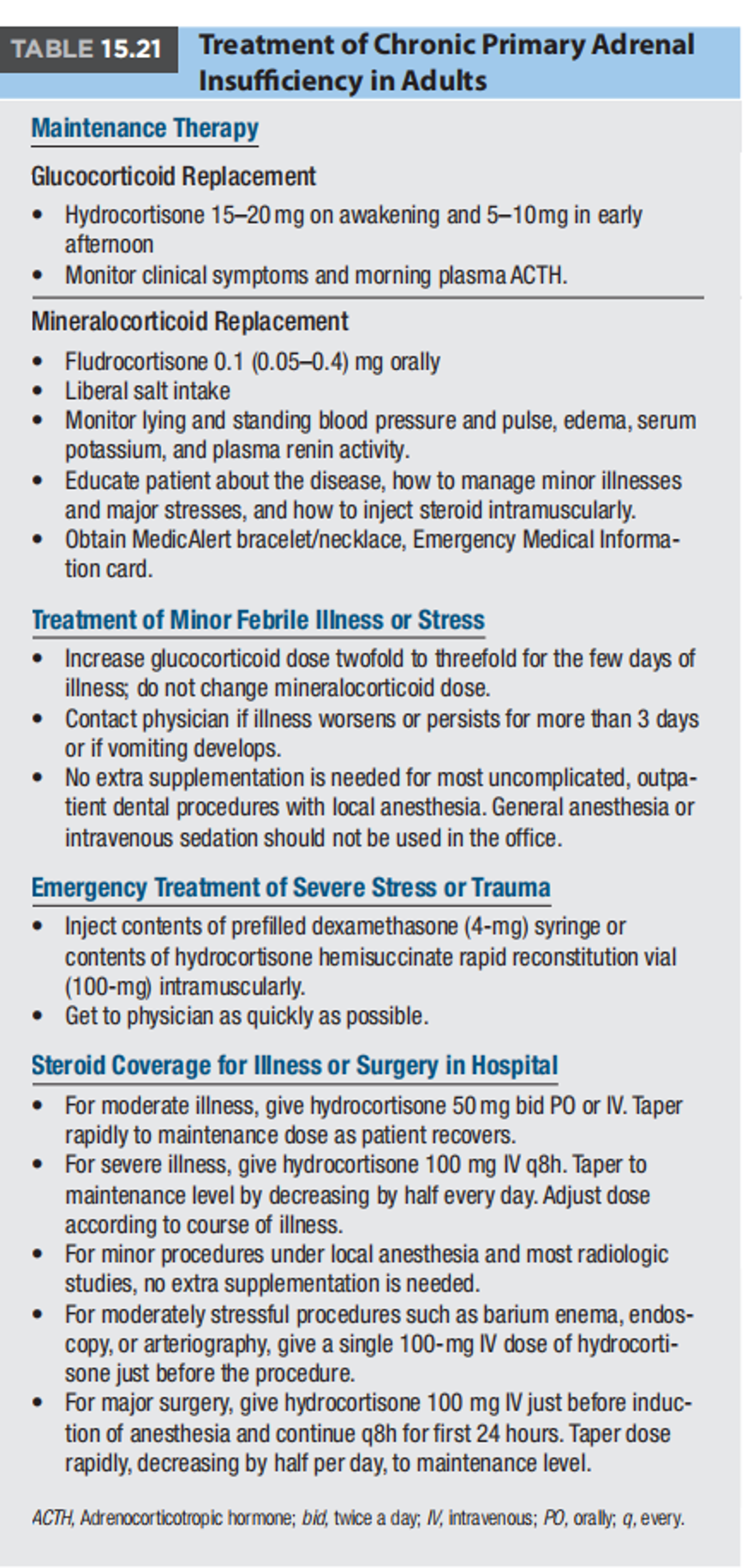
Treatment of Adrenal Insufficiency
- Glucocorticoid Replacement: Hydrocortisone is the most commonly used medication. Doses are adjusted based on individual needs.
- Mineralocorticoid Replacement (for Primary Adrenal Insufficiency): Fludrocortisone is used to replace aldosterone.
- Management of Adrenal Crisis: Requires immediate intravenous hydrocortisone, fluid resuscitation, and identification of the precipitating cause.
- Patient Education: Patients should wear a medical alert bracelet and be educated about “sick day rules” for increasing steroid doses during illness or stress.
-
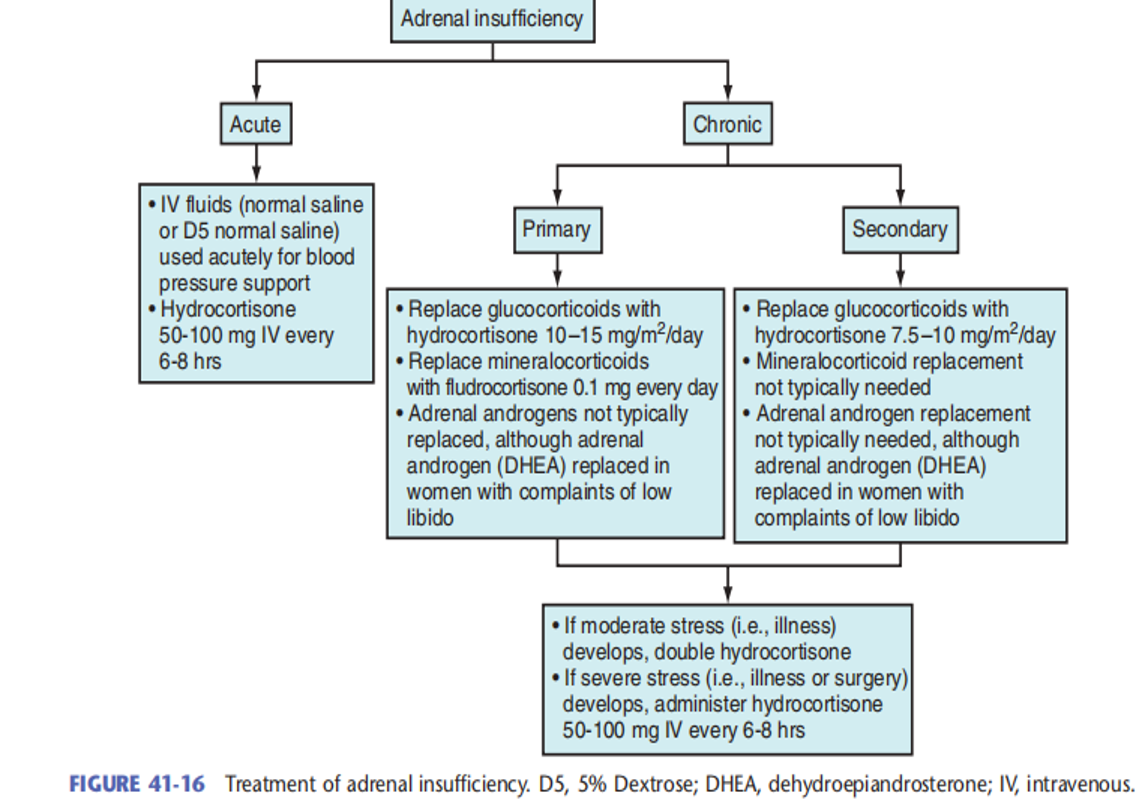
Adrenal insufficiency: treatment differs based on cause of adrenal insufficiency (e.g., primary versus secondary) as well as whether or not adrenal insufficiency is acute or chronic
-
Usual dose is hydrocortisone 10 to 12.5 mg/m2 /day
-
Oral dose is usually divided into 10 to 15 mg in the morning and 5 to 10 mg later in the day to mimic normal cortisol secretion pattern
-
The lowest dose that improves the patient’s symptoms should be used
- Dose should be increased during intercurrent illnesses
- All patients should wear a medical alert bracelet or necklace stating their adrenal insufficiency status
- Mineralocorticoid (fludrocortisone 0.05 to 0.2 mg/day) is used only in primary adrenal insufficiency
Summary
- Adrenal insufficiency is a serious condition requiring lifelong hormone replacement therapy.
- Early diagnosis and treatment are crucial to prevent complications, including adrenal crisis.
- Addison’s Disease (Primary Adrenal Insufficiency) is characterized by hyperpigmentation, hyponatremia, and hyperkalemia.
- Understanding the differences between primary and secondary adrenal insufficiency is essential for proper management.
Surgery
Hypofunction of adrenal cortex, leads to low levels of
- Glucocorticoids
- Mineralocorticoids (aldosterone)
- Androgens
Which test is used to diagnose adrenal insufficiency? a) Blood glucose test b) Thyroid function test c) ACTH stimulation test d) Lipid profile test