IM
Crohn’s Disease
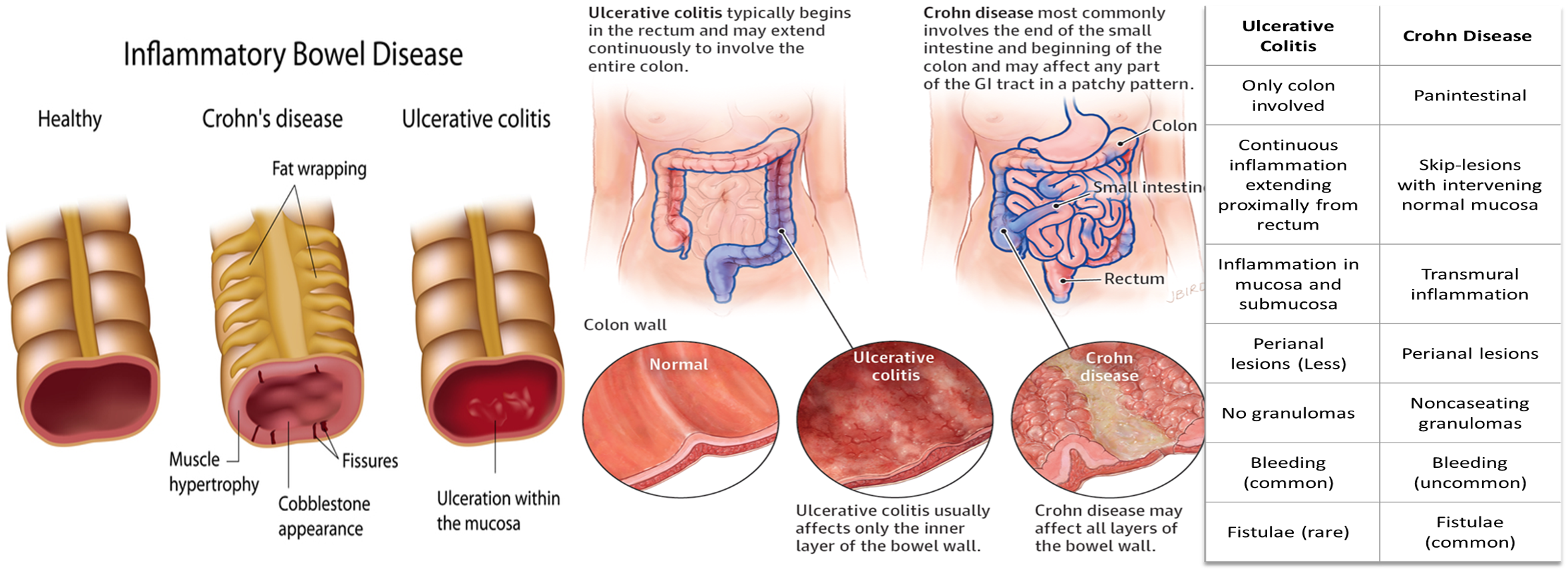
Locations and Layers Involved Limited to the colonic mucosa.
-
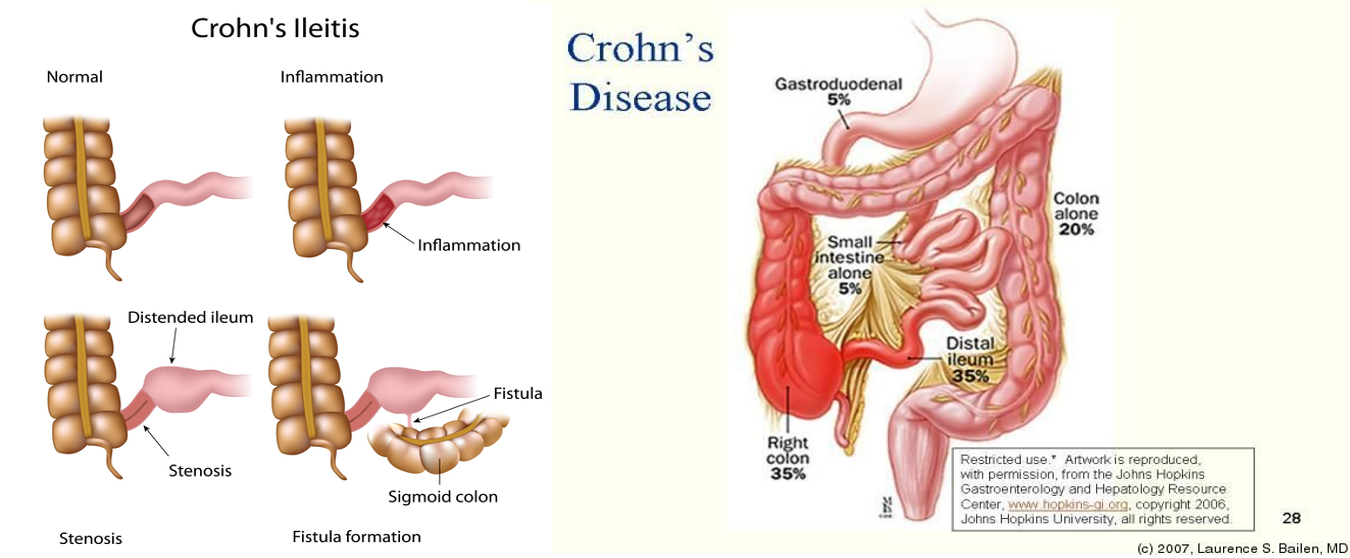
Anywhere from mouth to the anus with a special preference to the terminal ileum and cecum, but characteristically spares the rectum in most cases.
-
All layers of the bowel wall are involved (mucosa, submucosa, muscular layer, and outer serosa). It causes segmental disease.
Pathophysiology
NOD2; innate immune failure TH1 = IFN B TNF A; NCG IL12 + IL23 =TH 17 mucosal damage
- Causes: Interaction between
- Genetic (family history + NOD-2 mutation) and (Long arm C16; NOD2 protein)
- NOD2 Protein Function:
- Normally involved in recognizing bacterial components and triggering an immune response.
- Mutation leads to abnormal signaling, resulting in the release of cytokines in the nucleus.
- This abnormal cytokine release can cause phagocytes to engulf cells improperly.
- Failure of Innate Immune Response:
- The innate immune system fails to respond effectively due to the mutation.
- This failure necessitates the activation of the adaptive immune system.
- Adaptive Immune Response:
-
Cellular immunity becomes more prominent.
-
Granuloma formation occurs as a result of the adaptive immune response trying to contain the infection or inflammation.
-
Family History High risk >50% for twins
-
-
Environmental factors (western diet and smoking) and
- western food,
- Smoking (increased risk CD, protective to UC),
- NSAIDS (Reduce mucosal production),
- Antibiotics (Flush microbiome),
- western food,
-
Disturbed Tight Junction
-
Immune-dysregulation.
-
Hyperactivation of Th1:
-
Releases IFN-gamma and TNF-alpha causing general symptoms of the disease, transmural ulcers, and Non ceasating granuloma formation - similar to sarcoidosis.
-
secretes IL12 and IL23: Leads to activation of Th17 which in turn increases mucosal damage by neutrophil recruitment =/ Intraabdominal abcess
-
-
CD Histology
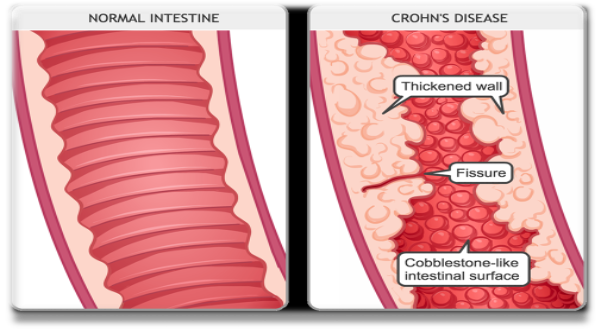
- Transmural ulcer
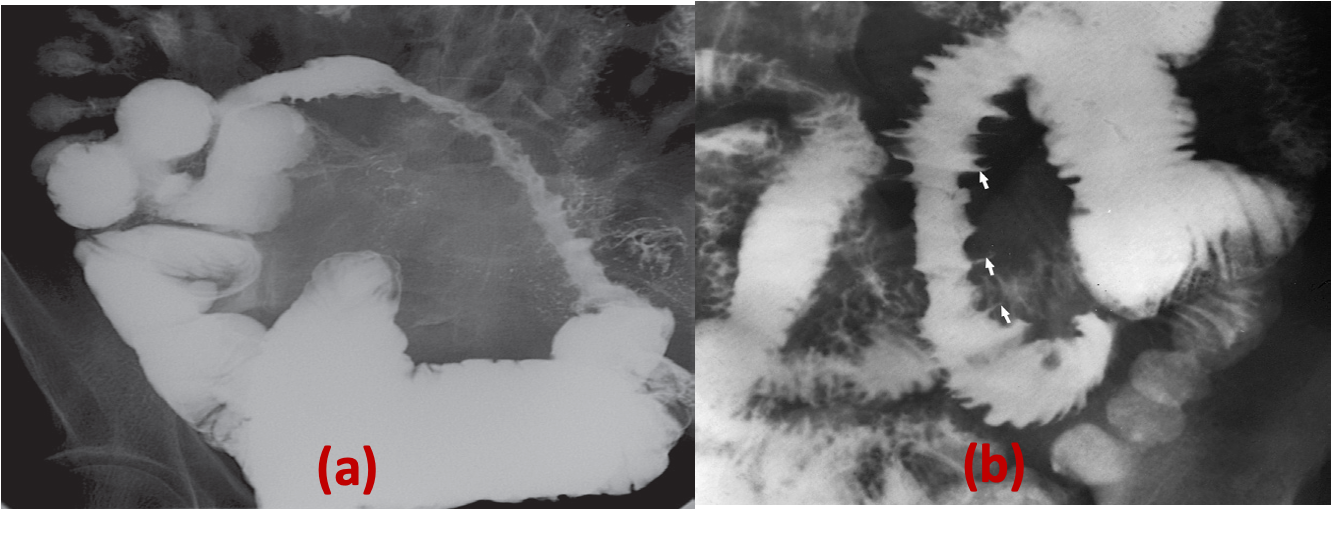
- Scattered lesions with relatively normal mucosa in between (classic cobblestone appearance)
- Non-caseating granuloma
- Reserved crypt architecture
CD Clinical Picture
-
Abdominal pain
-
Watery diarrhea/steatorrhea; due fat malabsorption
-
Weight loss
-
Fat-soluble vitamins deficiency due to malabsorption; may mimic malnutrition features of KADE Vitamin K deficiency, vitamin A Deficiency, Vitamin D Deficiency, Vitamin E Deficiency
-
B12 malabsorption leading to macrocytic anemia
-
Biliary stones and Kidney stones
- Kidney; bile acid not absorbed, resulting in high fat to large intestine - in colon resulting reabsorption of potassium, water - hydroxalate cc should pass fully in this case they are reabsorbed with calcium; when in steatorrhea due bile acid deficiency, oxylate connect with //// - calcium oxylate stone
-
Fistula formation between the intestine and other nearby structures like other intestinal lobes, skin, perianal region - could be from lobe to lobe of intestine; consequence= malabsorption | may open directly to the skin | may open to the urinary bladded with UTI’s; nematourea? cc | may open to the vagina recurrent infections | most likely on perianal fistulas
-
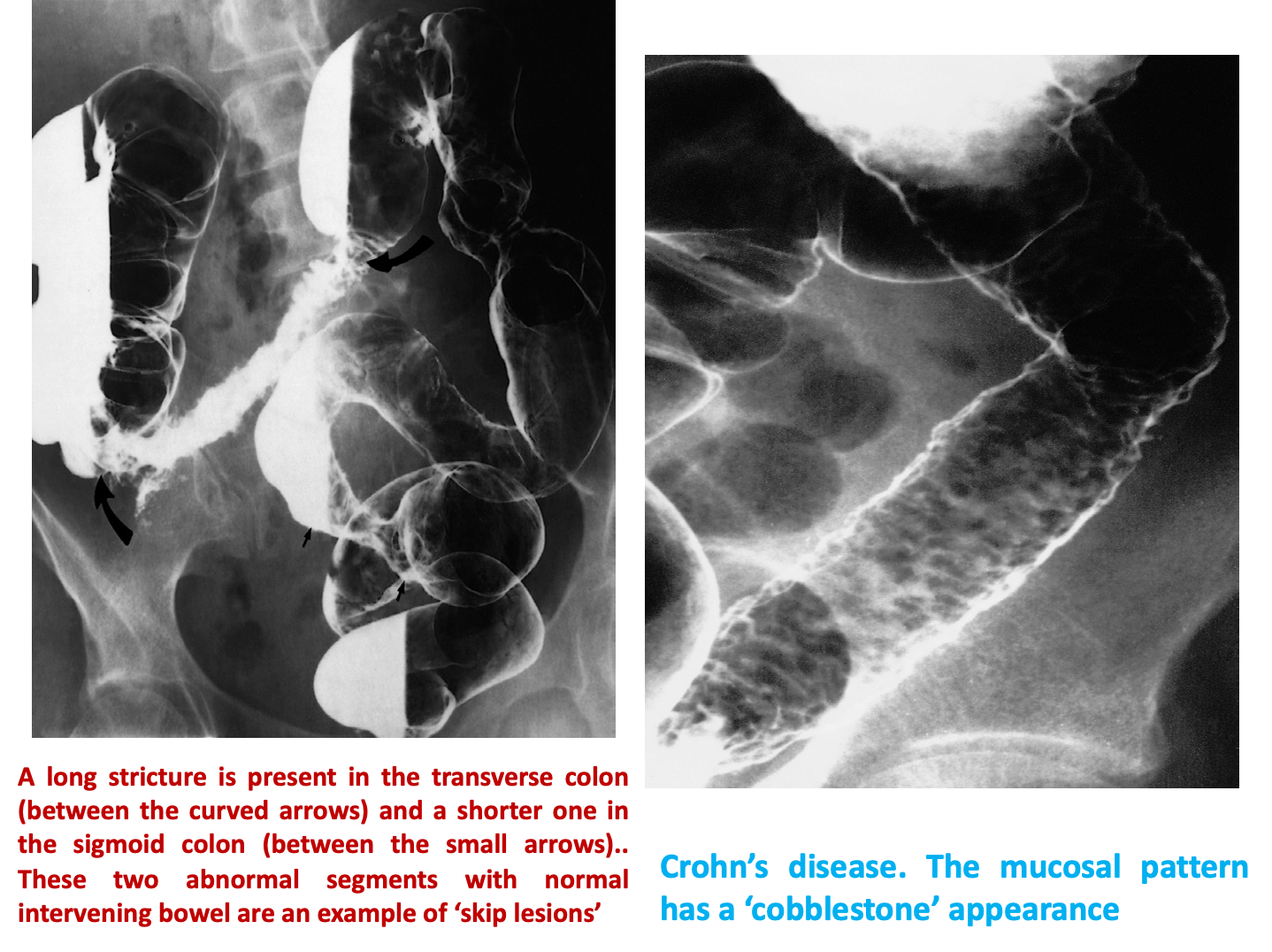
Stricture formation leading to obstruction
-
Small intestinal cancer
CL higher ration to bile
Specific Investigations
- Antibodies: Anti-saccharomyces cerevisiae antibodies (ASCA)
- Barium SBFT/enema: String sign
- Colonoscopy and biopsy: Skip lesions, cobblestoning, transmural ulcers
- MRI: Creepy Fat appearance.
- X-Ray: Air-fluid level and dilated loops to rule out SBO.
Treatment: CD
-
Mild to moderate disease:
-
Ileal disease flare is treated with oral budesonide; may result cushings then maintain remission with 6-MP or AZA; purine synthesis inhibitors; aptosis immune cells; immune compromised; resulting in Opportunistic infections. (SAME as UC)
-
Colonic UC flare is induced by 5-ASA and maintained by 5-ASA
-
-
Moderate to severe disease:
- Induction of remission with prednisone then maintain remission with AZA or 6-MP or infliximab; Maintenance + Remission do IFN-gamma to avoid reactivation of TB prior to administration
-
Severe/refractory disease:
Induction treatment: ciprofloxacin; DNA Gyrase inhibitor | Metrindiazole for UC (giving to CD only in fistulating crohns, abdominal abcess; otherwise it will increase intestinal obstruction due healed fibrosis)
Surgery
Surgery (not curative) mostly performed in patients with complications of the disease (strictures, fistulae, and perianal disease) ; generally, consists of conservative resection. - short bowel syndrome
Other notes
- backwashing terminal illeum through scopy
- 30% crohn involvement in rectum
- 40% terminal illeum
Surgery
Crohn’s disease
Disease could affect any part of GIT from mouth to anus, 50% of cases both small and large bowel are involved
Causes:
- Inflammation caused by an unusual strains of mycobacteria.
- Uncertain aetiology
- Cigarette smoking is a common risk factor
- Hereditary
- Immunological
It is characterized by full thickness inflammatory process of any part of GIT from lips to anal margin.
Pathological features include full thickness inflammation, edema, fissures/ulceration, non- caseating foci of epithelioid and giant cells.
A chronic disorder with exacerbation, remission and varied clinical presentation:
- Recurrent abdominal pain and diarrhea
- Weight loss
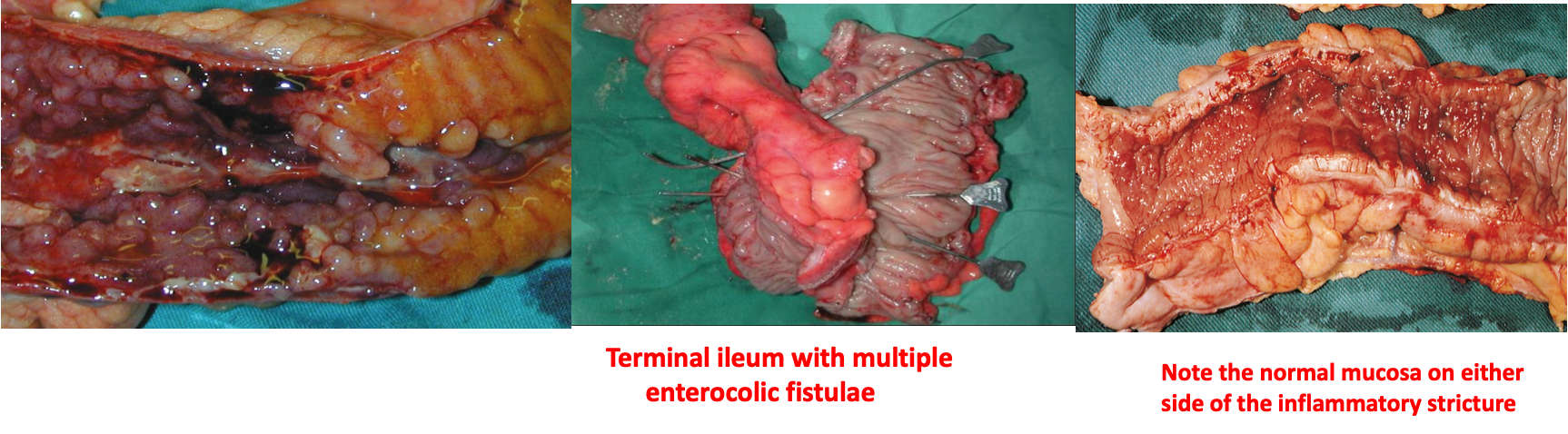
 Note the normal mucosa on either side of the inflammatory stricture
Note the normal mucosa on either side of the inflammatory stricture
Terminal ileum with multiple enterocolic fistulae
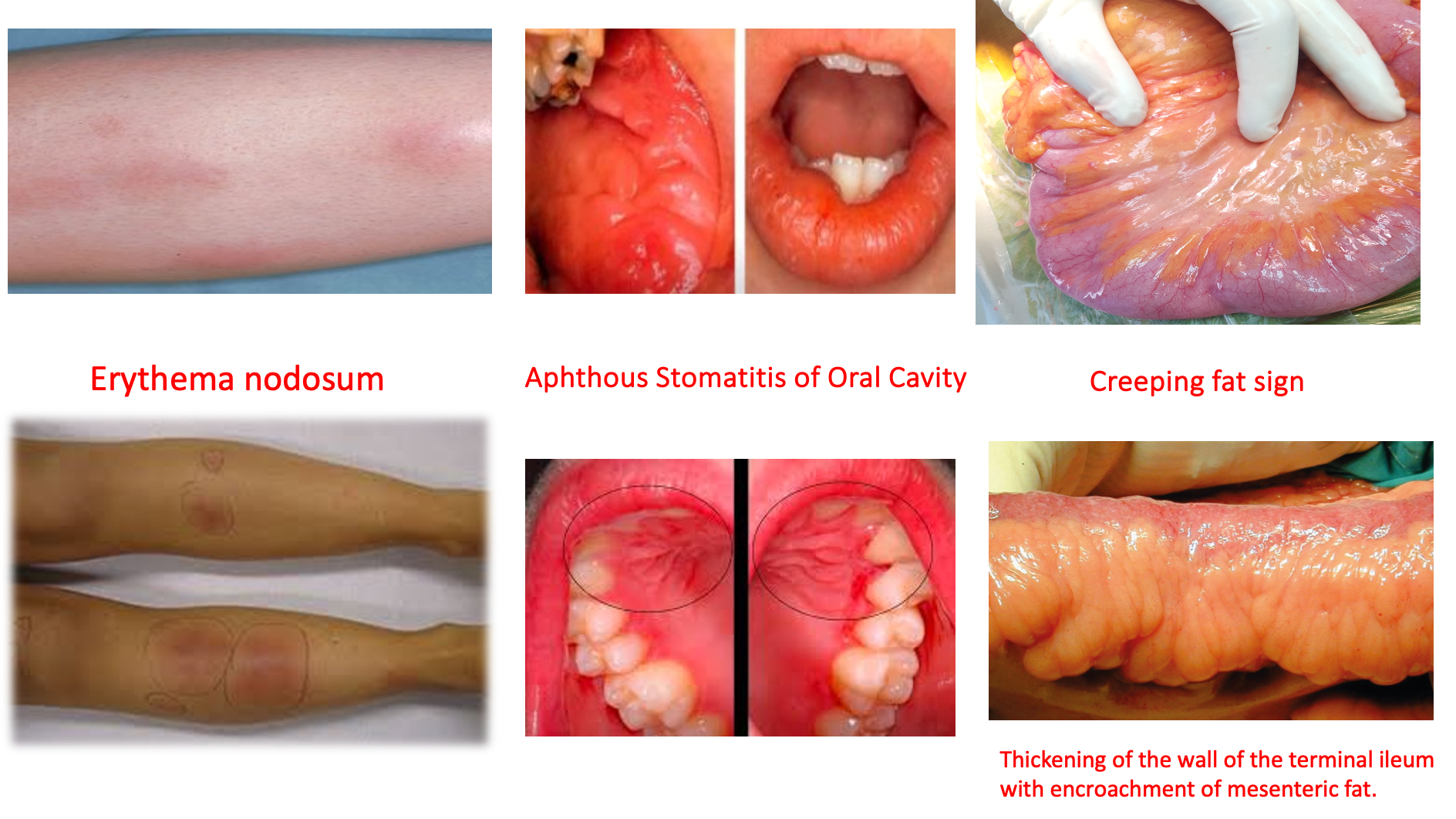
Creeping fat sign Thickening of the wall of the terminal ileum with encroachment of mesenteric fat.
Aphthous Stomatitis of Oral Cavity
Erythema nodosum
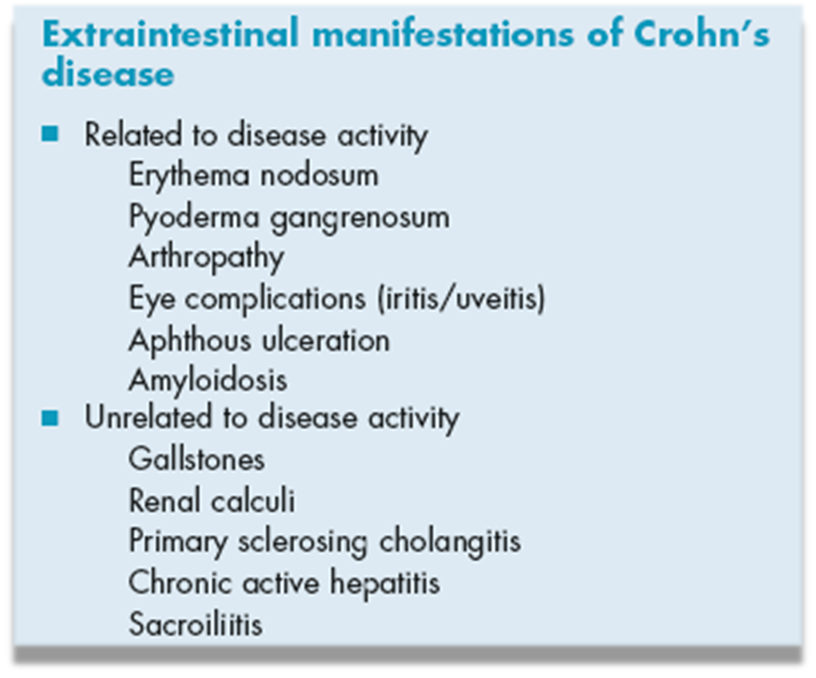
Symptoms of complications:
- Bowel obstruction( stricture – adhesions)
- Fistulation (to other organs)
- Anal, & perianal diseases (25%)
- Extra-intestinal
Investigations:
- Labs (WBS, Hb)
- Blood : Anemia, high C- reactive protein and low Vit-B12 levels
- Barium meal and follow through
- CT abdomen with oral and I/V contrast
- Colonoscopy/ with biopsy
- Capsule endoscopy/ Enteroscopy
Management:
- Medical:
- Nutritional correction-
- Corticosteroids-
- Aminosalicylates-
- Immunosuppression (azathioprine- 6 mercaptopurine)- Monoclonal antibodies
- Surgical: Resections, strictureplasty or colectomies.
Indications:
- Complications (perforation, fistulation, haemorrhage, abscess)
- Failure of medical therapy
- Perianal disease
- Malignancy
Imaging
Z It can affect any part of GIT but usually involve the small intestine specially the terminal ileum. Characteristic radiological features are
- skip lesion,
- aphthus ulcers,
- strictures,
- lymphadenopathy and
- fistula formation
A) Narrowing. There is a long stricture in the ileum due to Crohn’s disease. There is also separation of the abnormal segment from other loops of the bowel.
B) Ulceration. Abnormal loops of bowel in Crohn’s disease showing the ulcers as outward projections.